Effects of auricular point sticking on dry eye in myopia patients after SMILE surgery: a prospective randomized controlled clinical trial
2021-04-23ZhangDan张丹HuangXiaofei黄晓菲ZhaoYue赵越YangGuang杨光KongXiehe孔谐和ZhangCuihong张翠红HongJue洪珏YangYanting杨延婷LiuJie刘婕MaXiaopeng马晓芃
Zhang Dan (张丹), Huang Xiao-fei (黄晓菲), Zhao Yue (赵越), Yang Guang (杨光), Kong Xie-he (孔谐和),Zhang Cui-hong (张翠红), Hong Jue (洪珏), Yang Yan-ting (杨延婷), Liu Jie (刘婕), Ma Xiao-peng (马晓芃),
1 Shanghai Research Institute of Acupuncture and Meridian, Shanghai 200030, China
2 Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
Abstract
Objective: To observe the intervention effect of auricular point sticking on dry eye in myopia patients after small-incision lenticule extraction (SMILE) surgery.
Methods: This was a prospective randomized controlled study conducted among the myopia patients who received SMILE surgery at Eye and ENT Hospital of Fudan University. The post-SMILE operation patients who screened by the inclusion and exclusion criteria were randomized into a control group and a treatment group. Patients in the control group were given 0.1% fluorometholone and 0.5% carboxymethylcellulose sodium eye drops, while the treatment group was given additional unilateral auricular point sticking for 1 month. The patients were estimated using ocular surface disease index (OSDI), Schirmer tear test-1 (STT-1), tear film break-up time (TF-BUT), corneal fluorescein staining (CFS)score, corneal sensitivity (CS) and visual quality (VQ) at 1 d, 1 week and 1 month after surgery; the changes in anxiety and depression were also observed in the patients.
Results: Compared with the first day after operation, CS in the nasal region was improved in the treatment group, and the VQ score increased in the control group patients at 1 week after operation (both P<0.05); at 1 month after operation,the TF-BUT increased, CFS score decreased, CS in the central and nasal regions increased (all P<0.05), and VQ score increased (P<0.01) in the treatment group, and the CS in the central, upper, lower and nasal regions were improved (all P<0.05), and VQ score increased (P<0.01) in the control group. The between-group comparison showed that the differences in the change of TF-BUT were statistically significant at 1 week and 1 month after surgery, respectively (both P<0.05).
Conclusion: Auricular point sticking therapy can increase the TF-BUT and accelerate the repair of ocular surface function in post-SMILE patients.
Keywords: Auricular Point Sticking; Laser Therapy; Myopia; Postoperative Complications; Dry Eye Syndrome; Artificial Tears; Randomized Controlled Trial
Small-incision lenticule extraction (SMILE) is currently one of the conventional procedures in surgical treatment of myopia, featured by small incision and minimal invasion. It avoids complications resulting from mechanical microkeratomes for flap creation, and is more accurate, safer and more effective. Thus, SMILE has become the main-stream keratorefractive surgery in recent years. Dry eye (DE) is one of the most common complications and complaints in the early stage after SMILE surgery, not only affecting the surgical efficacy and bringing changes to vision, but also plausibly causing refractive regression[1-2]. The mechanism of DE after keratorefractive surgery is multifactorial, mainly including decreased nutrition supply to the corneal epithelium, declined corneal sensitivity (CS) affecting blink reflex, damage to the limbal goblet cells, and side effects of medications[3]. Early-stage DE after SMILE is mainly treated with artificial tears and usually takes 1-3 months to recover[4]. Despite certain mitigating effect of artificial tears on the ocular symptoms in DE and its convenience in use, the effectiveness and persistence of this treatment method are expected to improve.
Auricular points are distributed on the auricle and auricular point therapy treats diseases via stimulating these points. The stimulation varies from auricular point sticking, needling to electrical stimulation, among which,auricular point sticking is most frequently used. Electrical stimulation to auricular points was reported to improve DE symptoms[5], which inspired curiosity: if auricular point sticking can curb the DE symptoms after SMILE surgery? Since there is no report yet providing answers to this question, we conducted this prospective randomized controlled clinical trial to observe whether additional auricular point sticking can accelerate the repair of DE after SMILE based on the conventional artificial tears.
1 Materials and Methods
1.1 Study design
This was a prospective single-center randomized controlled clinical trial with subjects recruited from the Ophthalmology Department of Eye and ENT Hospital of Fudan University. The recruited patients all signed informed consent form. The study process is shown in Figure 1 in detail. This trial had completed the registration (http://www.chictr.org.cn/, No. ChiCTR-INR-16010074).

Figure 1. Process of the trial
1.2 Diagnostic criteria[6]
DE can be diagnosed with manifestation of one of any subjective symptoms including dryness, foreign body sensation, burning sensation, fatigue or discomfort in the eye, together with altered vision acuity, and tear film break-up time (TF-BUT) ≤5 s or Schirmer tear test-1(STT-1, without topical anesthesia, 5 min) ≤5 mm.
Or, the diagnosis can be confirmed when patient complained about one of the subjective symptoms including dryness, foreign body sensation, burning or fatigue sensation or discomfort in the eye, and TF-BUT >5 s but ≤10 s or STT-1 (without topical anesthesia, 5 min) >5 mm but ≤10 mm, in combination with positive corneal fluorescein staining (CFS).
1.3 Inclusion criteria
Conforming to the indication of SMILE surgery and having received the surgery; willing to participate in the trial, with good compliance; age between 18-40 years old;preoperative diopter of spherical power between -3.0 and -10.0 DS and diopter of cylinder power between 0 and -5.0 DC; in absence of DE symptoms prior to surgery;presenting with one or more of the following symptoms after surgery: dryness, foreign body sensation or burning sensation in the eye, visual fatigue and photophobia.
1.4 Exclusion criteria
Taking any medication that may affect the examination results 1 day ahead; having received any optical surgery or treatment within the previous 6 months before the first examination; having received temporary or permanent lacrimal punctum embolization within the previous 6 months before the first examination; coupled with other eye disorders; patients in pregnancy or breast-feeding; serious systematic diseases involving cardio-cerebrovascular system, liver,kidney or hemopoietic system and mental disorders.
1.5 Randomization and blinding
Simple randomization method was adopted for grouping and SPSS version 22.0 software was used for the generation of random numbers and allocation table.The patients were screened using the inclusion and exclusion criteria and the recruited participants were randomized into a treatment group and a control group at a ratio of 1:1. The allocation of participants was in the charge of one single researcher independently. The one who offered treatment was not involved in the checking of outcome measures and the one who performed outcome measures was not involved in the final data computing.
1.6 Statistical analysis
SPSS version 22.0 software was used for data analysis.The measurement in line with normal distribution were expressed as mean ± standard error of mean (x±SEM)and those not were expressed as median (lower quartile,upper quartile) [M (QL, QU)]. Comparison of measurement data was performed using Chi-square test.The generalized estimation equation was employed to analyze the repeated measurement data in the two groups which were not in line with normal distribution,so were the effects of intervention duration and methods on the treatment efficacy, as well as the interaction between the two intervention factors.Between-group comparisons of the changes in the parameters from 1 d after operation till 1-week and 1-month treatment, respectively, which did not conform to normal distribution, were performed using nonparametric test.P<0.05 indicated a statistically significant difference.
1.7 Interventions
1.7.1 Control group
The control group was given conventional postoperative treatment including 0.1% fluorometholone eye drops (Santen Pharmaceutical Co., Ltd., Japan),1 drop each time, 8 times a day, reduced by 1 time every 3 d, for 24 consecutive days, and 0.5% carboxymethylcellulose sodium eye drops (Allergan Pharmaceuticals, Ireland), 1 drop each time, 4 times a day, for a total of 1 month. The two eye drops were supposed to use separately at an interval of 10 min or longer, but the sequence did not matter.
1.7.2 Treatment group
In addition to the same intervention given to the control group, auricular point sticking was offered to the treatment group.
Auricular points: Eye (LO5), Pingjianqian (TG2i),Pingjianhou (AT1i), Liver (CO12), Spleen (CO13), Kidney(CO10) and Shenmen (TF4), (Figure 2).
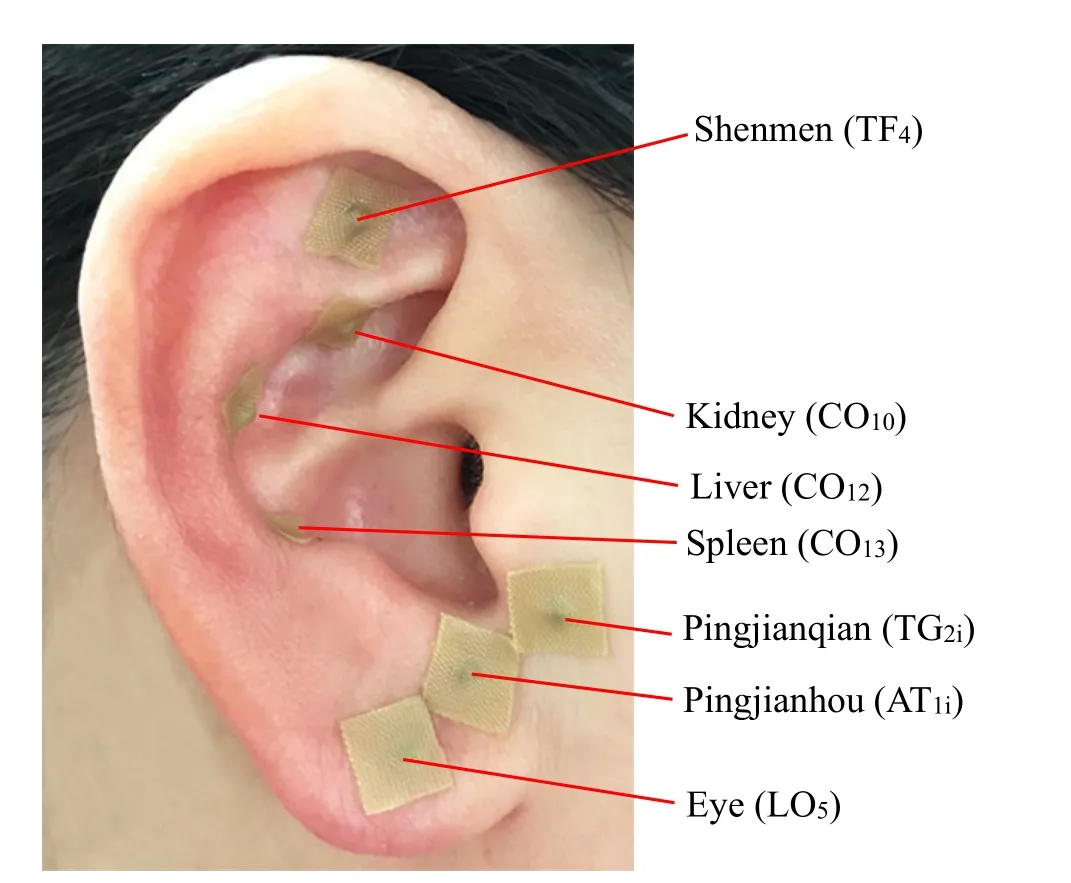
Figure 2. Illustration of the auricular points
Operation: TheNomenclature and Location of Auricular Points(GB/T13734-2008)[7]was referred to locate the auricular points. There is one magnetic bead stuck to each piece of plaster at the center (Figure 3,Suzhou Medical Appliance Factory, China). After standard sterilization of one ear, the auricular plasters were applied to the ear with the magnetic beads aiming precisely at the auricular points. Patients were required to press the points one by one every day, 30 times for each point each time, for 4 rounds each day with 4 h in between. One ear was treated each time and the two ears were treated alternately every 3 d for a total of 1 month.
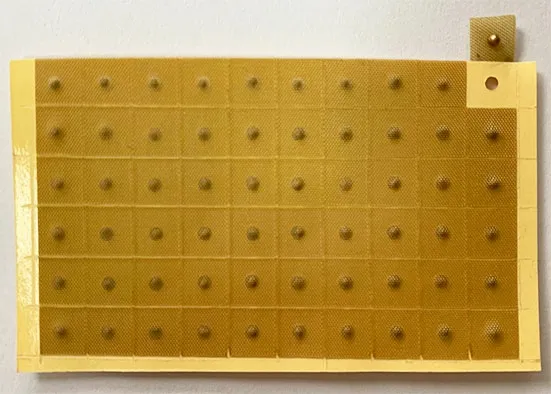
Figure 3. Magnetic auricular point plasters
1.8 Outcomes
1.8.1 Primary outcome measure
TF-BUT: Normal saline-wetted sodium fluorescein strips were used to stain the cornea and a slit lamp (66 VISION TECH Co., Ltd., China) was then used to observe the time till the first dry spot occurred on the cornea. The observation was repeated 3 times to obtain a mean value. Tear film was considered unstable when the mean value <10 s[8].
1.8.2 Secondary outcome measures
Tear meniscus height (TMH): Optical coherence tomography was taken for the measurement. Each eye was measured 3 times to obtain a mean value[9].
CFS and scoring: The observation of CFS was conducted following TF-BUT test using the slit lamp.Damaged cornea would present dots or patches of staining. The result was scored using a 12-point scale when cornea was divided into 4 quadrants: no staining,0 point; mild staining, 1 point; moderate staining, 2 points; severe staining, 3 points. The total score was in the range of 0-12 points. A higher score indicated more serious damage to the cornea[10].
STT-1 (without topical anesthesia, 5 min): A strip of graduated filter paper of 5 mm × 35 mm (Tianjin Jingming New Technological Co., Ltd., China) was gently put at the inferior fornix by the outer 1/3 and removed 5 min later to measure how long of the paper was moisturized. A length <10 mm indicated decreased tear secretion[11].
CS: A CS apparatus (Luneau Ophtalmologie, France)was adopted to detect CS. While the patient was looking straight forward, the examiner held the apparatus to perpendicularly touch the center of the cornea and the upper outer quadrant of bulbar conjunctiva with the end of the filament. Slightly bending of the filament seen by the examiner and sensing of the filament by the patient made a positive test result. The maximal length was used in the very beginning and reduced by 5 mm each time,until a positive result was achieved and recorded[12].
Subjective symptoms: Ocular surface disease index(OSDI) was adopted for evaluation. This scale mainly estimated the ocular symptoms, visual function and environmental factor covered by 12 questions which were scored 0-4 points each[13]. Total score = Sum of the component scores × 25 ÷ The number of answered questions. The total score ranged from 0 to 100 points. A higher score suggested more serious symptoms.
Visual quality (VQ) survey: This was implemented using a questionnaire which had two sections which were postoperative subjective symptoms evaluation and separate evaluation of the left and right eyes for the subjective symptoms. The sections scored each symptom in the range of 0-10 points. The general score was calculated finally. A higher score meant less and milder visual discomforts or symptoms and a better VQ[14].
Anxiety and depression evaluation: The hospital anxiety and depression scale (HADS)[15-16]was used. This scale contained two parts, anxiety and depression,covering 14 items which were scored 0-3 points each.The total score for both anxiety and depression was 0-21 points. Anxiety or depression symptoms were identified when the score >7 points. The abovementioned scales were completed by patients independently.
1.9 Safety evaluation
If any adverse events or reactions happened, records would be kept and proper treatment would be provided accordingly. When adverse reactions occurred, the severity would be estimated to see if the study should be ceased.
2 Results
2.1 Participants and baseline
A total of 75 eligible patients were recruited. They were randomized into a treatment group of 37 cases and a control group of 38 cases. By the end of treatment,there were 4 dropout cases and 33 completed cases in the treatment group, versus 5 dropout cases and 33 completed cases in the control group. The general data of the two groups are shown in Table 1.
2.2 Results of the primary outcome
On the first day after SMILE surgery, there was no significant difference in TF-BUT between the two groups(P>0.05), suggesting the comparability.
Compared with post-operation day 1, neither of the two groups showed significant change in TF-BUT after 1-week treatment (bothP>0.05); TF-BUT showed significant improvement after 1-month intervention in the treatment group (P<0.01), while there was no significant change in the control group (P>0.05). Details are shown in Table 2 and Table 3.
Between-group comparison of the changes in TF-BUT,at 1-week treatment and 1-month treatment,respectively, showed statistical significance (bothP<0.05). Details are shown in Table 4.
2.3 Results of the secondary outcomes
On the first day after SMILE surgery, there were no significant differences in TMH, STT-1, CFS and CS between the two groups (allP>0.05), indicating the comparability. Compared with post-operation day 1,there were no significant changes in TMH, STT-1 and CFS in the two groups after 1-week treatment (allP>0.05); no significant changes were observed in TMH and STT-1 after 1-month treatment in the two groups (allP>0.05),but CFS showed significant improvement in the treatment group (P<0.05). Compared with postoperation day 1, CS in the nasal region showed certain improvement in the treatment group after 1-week intervention (P<0.05), while no significant change was found in CS in the control group (P>0.05); after 1-month treatment, both groups showed marked improvement in CS in the central and nasal regions (allP<0.05). Details are shown in Table 2 and Table 3.
There were no significant between-group differences in the OSDI and VQ scores on the first day after SMILE surgery (bothP>0.05), indicating the comparability. The VQ score was significantly changed after 1-week treatment in the control group (P<0.05); the VQ score showed marked increases in both groups after 1-month intervention compared with the baseline (bothP<0.01),(Table 2 and Table 3).
There was no significant between-group difference in the HADS score between the two groups 1 d after SMILE surgery (P>0.05), indicating the comparability.Comparison of the changes in the HADS score between the two groups, at 1-week and 1-month treatment,respectively, showed that the differences were statistically insignificant (bothP>0.05), (Table 4).
There were no treatment-associated adverse events during the entire study.
3 Discussion
From photo-refractive keratectomy (PRK) to laserin situkeratomileusis (LASIK), till all-laser surgery and SMILE,laser keratorefractive surgery has gradually realized minimal invasion to the cornea in recent years,manifested by high safety, effectiveness and predictability. However, studies have shown that 20%-40% of the patients would experience a short period of DE after PRK surgery, and some patients are at risk of developing chronic dry eye disease (DED), affecting their health status[3,17]. Some research holds that the basic state of the ocular surface before surgery, the use of medication during and after surgery, the type and operation process of the surgery, and the postoperative corneal injury and recovery are all important factors in the development of DE after laser keratorefractive surgery[18].

Table 1. Comparison of the general data before SMILE surgery

Table 2. Comparison of each item among different time points in the treatment group [M (QL, QU)]

Table 3. Comparison of each item among different time points in the control group [M (QL, QU)]
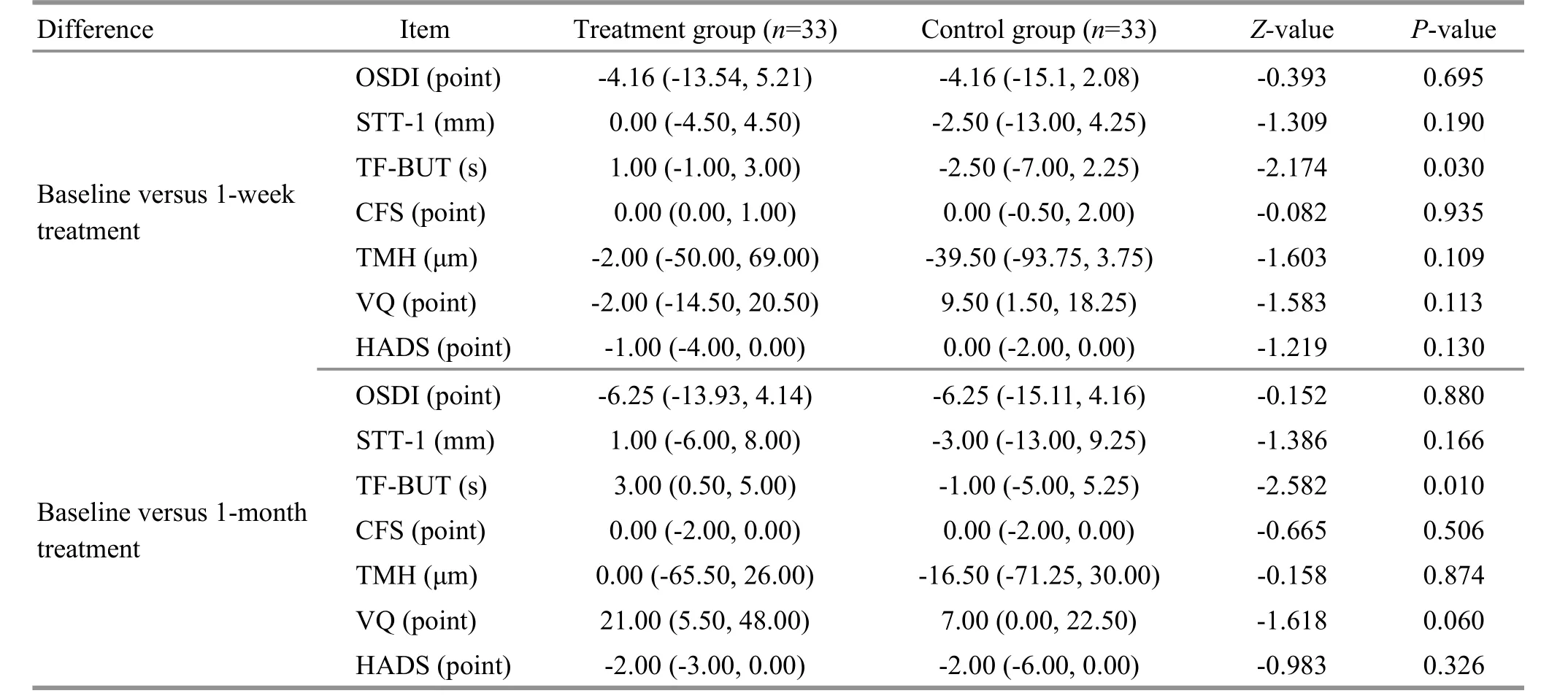
Table 4. Between-group comparison of the changes in OSDI, STT-1, TF-BUT, CFS, CS, TMH, VQ and HADS [M (QL, QU)]
SMILE is a novel type of laser keratorefractive surgery.It is featured by mild corneal response, early incision healing, minimal chance of infection, and fast vision recovery. It has been approved by the U.S. Food and Drug Administration (FDA) for treatment of myopia and myopic astigmatism in 2016 and 2018, respectively[19].Among post-SMILE complications, the reported rate of DE is nearly 56%, which is thus considered an significant factor affecting postoperative satisfaction of patients[20].Therefore, it is worthy of great attention to seek an efficient way to alleviate DE and improve the VQ of patients after SMILE.
Up to date, the pathogenesis of post-SMILE DE is still unclear. Zhang H,et al[21]believe that irregular corneal surface can directly influence the distribution of tears on the corneal surface, causing tear film instability, which is one of the crucial mechanisms in DE development after SMILE. Other research suggests that surgery-induced mild-to-moderate corneal inflammation may also be involved in the process of postoperative tissue damage and healing[22]. Combination of artificial tears or lubricants and anti-inflammatory drugs is a common intervention for patients after SMILE[1,23]. Nevertheless,there is no unified conclusion on the choice of drugs yet worldwide, though steroid hormones such as dexamethasone, fluorometholone and cyclosporine are majorly selected anti-inflammatory drugs, and sodium hyaluronate and carboxymethylcellulose sodium eye drops are commonly used to supplement tears[24-26]. In this study, patients in the control group were given fluorometholone and carboxymethylcellulose sodium eye drops. The results showed that VQ score increased after 1-week and 1-month treatment in the control group patients compared with the baseline, but DEassociated indicators showed insignificant changes.Although artificial tears can mitigate post-SMILE DE to a certain extent, DE usually lasts for 3-6 months, or even more than 6 months[1,27]. Moreover, the use of artificial tears is still controversial. It requires multi-center largesample clinical trials to confirm whether it should be offered on demand or on schedule and what dose is proper. Therefore, it is of great clinical value to explore effective therapies to prompt the tear film to return to a steady state in patients after refractive surgery.
A study used Chinese medication together with artificial tears to treat DE after SMILE, and the results showed that the efficacy of the integrated treatment won out that of artificial tears alone[28]. In recent years,auricular point sticking has gradually been used in the clinical treatment of various diseases, and the result is positive[29-31]. In the treatment of ophthalmological diseases, meta-analysis suggested that auricular point sticking can improve myopia in adolescents[32]. Auricular point stimulation has been proven to have a satisfactory therapeutic effect on DE, but there is no report yet on the effectiveness of auricular points in treating DE after SMILE[5]. In this study, patients in the treatment group were given additional auricular point sticking on the basis of the intervention offered to the control group.The results showed that TF-BUT was significantly prolonged after 1-month intervention in the treatment group and the changes in TF-BUT after 1-week and 1-month treatment were more significant in the treatment group than in the control group. Post-SMILE patients usually present DE characterized by short TF-BUT[21]. This study also showed that TF-BUT of the control group continued to decrease, while it maintained increasing in the treatment group. In addition, compared with the baseline, the CFS score was significantly reduced, corneal perception returned to normal and the VQ score increased after 1-month intervention in the treatment group, though there were no significant differences in the changes in the above items between the two groups.Although neither of the two groups showed marked change in the OSDI score after intervention, there was a significant between-group difference in the change of the HADS score. The above results suggested that additional use of auricular point sticking can increase the TF-BUT of patients after SMILE, help speed up the repair of ocular surface function, and improve the emotional state of patients. The mechanism of auricular point sticking is still a mystery, but it may be related to the local effect or central integration regulation induced by nerve stimulation[33]. The auricular points selected in this study distribute the mixed branch of the facial nerve, greater auricular nerve, and auriculotemporal nerve. Facial nerve is a mixed cranial nerve, mainly containing three fiber components. Among them, visceral motor fibers(parasympathetic fibers) are distributed in the lacrimal gland, submandibular gland and sublingual gland.Auricular points may stimulate the facial nerve to activate the secretion of tears, thereby mitigating DE.
This study was a prospective small-sample study to explore the intervention effect of auricular point sticking on DE in patients after SMILE. The results showed that on the basis of conventional medication, auricular point sticking can further improve the TF-BUT of patients after SMILE, help boost the recovery of the stability of tear film,and improve DE. As a simple non-drug external treatment method, it is worth recommending for the treatment of DE after SMILE. Nevertheless, this study had certain limitations. Firstly, the sample size was too small, so the results of the study expect to be confirmed by multi-center large-sample clinical studies; secondly,the follow-up work needs to be carried out, for 3 or 6 months following the intervention, to observe the longterm effect of auricular point sticking. Future studies should lay stress on these aspects.
Conflict of Interest
Author Ma Xiao-peng is a member of the Editorial Board ofJournal of Acupuncture and Tuina Science, and authors Yang Guang, Zhang Cui-hong and Hong Jue are the editors serving forJournal of Acupuncture and Tuina Science. The paper was handled by other editors and has undergone rigorous peer review process. Authors Ma Xiao-peng, Yang Guang, Zhang Cui-hong and Hong Jue were not involved in the journal’s review or decisions related to this manuscript.
Acknowledgments
This work was sponsored by the Youth Fund of National Natural Science Foundation of China (国家自然科学基金青年基金项目, No. 81904302); Scientific Research Project of Shanghai Municipal Health Commission (上海市卫生健康委员会项目, No. 201840174, No. 202040249); Shanghai Sailing Program (上海市青年科技英才扬帆计划项目,No. 19YF1445000).
Statement of Informed Consent
Informed consent was obtained from all individual participants.
Received: 15 April 2020/Accepted: 11 May 2020
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Review of systematic reviews of acupuncture for diabetic peripheral neuropathy
- Clinical observation on spleen-invigorating and qibenefiting pediatric massage for treating recurrent respiratory tract infection in children with cerebral palsy due to qi deficiency of spleen and lung
- Acupoint catgut-embedding therapy as promising treatment for non-alcoholic fatty liver disease
- Clinical observation of electroacupuncture with different frequencies for migraine without aura
- Warm needling moxibustion plus PKP for vertebral compression fracture due to kidney deficiency and blood stasis: a randomized controlled trial
- Evaluation of the prevention and treatment effects of acupuncture-moxibustion for Alzheimer disease based on various mouse models
