Obstetrical and gynecologic challenges in the liver transplant patient
2020-12-25IoannisZiogasMuhammadHayatGeorgiosTsoulfas
Ioannis A Ziogas, Muhammad H Hayat,Georgios Tsoulfas
Ioannis A Ziogas, Medical School, Aristotle University of Thessaloniki, Thessaloniki 54124, Greece
Muhammad H Hayat, Department of Medicine, Division of Gastroenterology, Hepatology and Nutrition, Vanderbilt University Medical Center, Nashville, TN 37212, United States
Georgios Tsoulfas, Department of Surgery, Papageorgiou University Hospital, Aristotle University of Thessaloniki, Thessaloniki 54622, Greece
Abstract An increasing number of childbearing agewomen undergo liver transplantation (LT) in the United States. Transplantation in this patient subgroup poses a significant challenge regarding the plans for future fertility, particularly in terms of immunosuppression and optimal timing of conception. Intrapartum LT is only rarely performed as the outcome is commonly dismal for the mother or more commonly the fetus. On the other hand, the outcomes of pregnancy in LT recipients are favorable, and children born to LT recipients are relatively healthy. Counseling on pregnancy should start before LT and continue after LT up until pregnancy, while all pregnant LT recipients must be managed by amultidisciplinary team, including both an obstetrician and a transplant hepatologist. Additionally, an interval of at least 1-2 years after successful LT is recommended before considering pregnancy. Pregnancy-induced hypertension, pre-eclampsia, and gestational diabetes mellitus are reported more commonly during the pregnancies of LT recipients than in the pregnancies of non-transplant patients. As adverse fetal outcomes, such asmiscarriage, abortion, stillbirth, or ectopic pregnancy, may occur more often than in the non-transplant population, early planning or delivery either through a planned induction of labor or cesarean section is critical to minimize the risk of complications. No significant long-term physical or phycological abnormalities have been reported in children born to LT recipients.
Key Words: Liver transplantation; Pregnancy; Obstetric complications; Immunosuppression; Fetal outcomes; End-stage liver disease
INTRODUCTION
The first successful liver transplantation (LT) in humans was reported in 1963[1]. Since then, owing to the numerous advances in surgical technique, organ preservation, immunosuppression, anesthesia, and pre- and post-operative care, LT has gradually become the mainstay of treatment for the management of end-stage liver disease[2]withincreased survival and quality of life[3]. Out of the 173801 theLT performed in the United Sates over the past 30+ years (1988-2020), 20129 (11.6%) were in women of reproductive age (18-49 years) (based on Organ Procurement and Transplant Network data as of February 17, 2020). Transplantation in this patient subgroup poses a significant challenge regarding the plans for future fertility, particularly in terms of immunosuppression and optimal timing of conception[4,5], and thus obstetric consultation plays a vital role in the care of this patient subgroup. The aim of this review is to summarize the current state of evidence on (1) the association of the female reproductive system and end-stage liver disease; (2) the role and outcomes of LT during pregnancy; and (3) the outcomes of pregnancy after LT.
FEMALE REPRODUCTIVE SYSTEM AND END-STAGE LIVER DISEASE
It is well known that liver dysfunction can lead to infertility, sexual dysfunction, amenorrhea, and irregular menstrual bleeding in women of childbearing age[6,7]. This effect is mostly attributed to alterations in the hypothalamic-pituitary-gonadal axis and the metabolism of sex steroid hormones, which lead to hormonal imbalances, including hypogonadotropic hypogonadism and elevated estrogen levels[7,8]. Even though these alterations can be seen in chronic liver disease of any etiology, continuing alcohol consumption, particularly in the setting of alcohol-induced liver disease, may further exacerbate this dysfunction of the hypothalamic-pituitary-gonadal axis in female patients[9]. A survey assessing the incidence of menstrual cycle abnormalities in women before LT showed that 28% of the women reported irregular menses and another 30% amenorrhea, and these rates were lower in the chronic liver disease group compared to women with acute liver disease[10]. In addition, Sorrellet al[11]reported that around56% of women with severe liver disease were no longer sexually active at the time of evaluation for LT, while about 42% of them had decreased interest in being sexually active. The authors also mentioned that these high rates of sexual dysfunction, based on patient interviews, were mostly due to their chronic illness, fatigue, and change in their body image[11]. In contrast, in a survey conducted by Mass and colleagues[10], 77% of the women reported being sexually active before LT.
LT DURING PREGNANCY
Mild liver dysfunction is a phenomenon commonly observed during normal pregnancy[12], however, severe liver dysfunction is a rare occurrence that is associated with significant mortality for both the fetus and the mother[13]. Severe liver dysfunction during pregnancy can be precipitated by (1) thestate of pregnancy itself; (2) preexisting disorders;and (3) a condition impacting the liver coincidentally(Table 1)[14]. Severe liver disease, regardless of the etiology, in rare cases, necessitatesLT as the only definitive therapy[7]either during pregnancy or in the puerperium. For instance, while the overall mortality of the hemolysis, elevated liver enzymes, low platelet count syndrome is 2%-3%, the presence of overt hepatic complications increases the maternal mortality upto 50%, and in such cases LT may be considered[7]. However, it is essential to diagnose carefully the underlying pathologyand decide upon whether we can resort to medical treatment or early delivery.
Only a few case reports have described the rare instances where LT was performed during pregnancy or during the puerperium. The first intrapartum LT case was performed in 1989 at 27 wk of gestation, and the indication was drug-induced fulminant hepatic failure[15]. The outcome was favorable for the mother, but neonatal death was reported due to premature delivery. Since then, only a few such cases have been published to date. The first LT case during the puerperium was reported by Ockneret al[16]in 1990and was performedfor the management of multisystem failure due to acute fatty liver of pregnancy3 dpost-partum after a 37-wk gestation. A healthy child was delivered without any adverse event for the mother.
LT during pregnancy has been associated with several adverse effects for either the mother or the fetus/newborn. According to the previously published case reports on LT during pregnancy, maternal survival has been shown to be optimal in most occasions with graft rejection (25%), cholestasis (22%), infections (13%), and impaired renal function (6%) being the most common reported adverse events[14,15,17-33]. On the other hand, fetal/neonatal outcomes after LT during pregnancy are not encouraging due to the high rates of intrauterine fetal death, induced abortion due to the anticipation of severe fetal complications, pre-term delivery, and intrauterine growth restriction[14,15,17-33]. However, thorough and elaborative discussions should be conducted with the mother in terms of maintaining pregnancy, as in some instances, fetal survival without any compromise was proven to be feasible.
PREGNANCY AFTER LT
Restoration of the female reproductive system after LT
The first successful childbirth after LT took place in 1978 and, despite the decreased birth weight, was accompanied by optimal fetal and maternal outcomes[34]. Since then, several reports have demonstrated the feasibility of pregnancy after LT[35-47]. Notably, the restoration of menstruation and childbearing potential is successful in around 97% of previously fertile female LT recipients[48,49]. It has been reported that within some months after LT (in a significant number of cases even within 1 mo[6]), sex hormone levels and sexual function normalize either partially or completely with amenorrhea reported in 26%, irregular bleeding in 26%, and regular menses restoration in 48% of the female LT recipients of childbearing age[50,51]. While the resumption of normal cycle is commonly seen in a few months after LT, recipients are recommended to avoid conception up until a year due to potentially worse outcomes[52,53]. Hence, family planning and consultation by a multidisciplinary team including a transplant hepatologist are pivotal for the well-being of these patients. Consultation should begin before LT. Naturally, these patients are prescribed combined oral contraceptives and transdermal contraceptive patches, which have traditionally resulted in no pregnancies and no overall changes in biochemistries, rendering them safe post-LT[54,55]. Asingle-center cross-sectional survey study demonstrated that only 35% (n= 28/80) of the women received appropriate recommendations for effective contraception post-transplant and only 28% of them (n= 8/28) did use effective birth controlafter consultation[56]. Although the study showed no important change in the distribution of contraceptive methods used post-LT, it revealed an increase in the rate of hormonal contraception (pre-LT: 2%vspost-LT: 10%,P= 0.044), and the most common contraceptive method was condoms both pre- and post-LT (pre-LT: 66%vspost-LT: 55%,P= 0.223)[56]. Although barrier methods are easy to use and decrease the risk of transmission of sexually transmitted diseases and fertility is immediately restored with cessation, the failure rate is quite high. Hormonal contraception is more effective but may take a few months for fertility to restore after cessation, may induce withdrawal symptoms, and increase the risk of venous thromboembolism (if combined estrogen/progestin). The maindifferences between the oral contraceptive pills and the transdermal patches include lower effectiveness in women weighing ≥ 90kg, local reaction or visibility, and a higher rate of dysmenorrhea and breast pain[57].Lastly, intrauterine devices offer the highest level of effectiveness with a low incidence of uterus perforation but have not been well-studied in LT recipients to date.

Table 1 Causes of severe liver dysfunction during pregnancy
Masset al[10]showed that the percentage of women being sexually active after LT slightly decreased from 77% to 72% post-LT. Notably, a cross-sectional study failed to show any significant differences in the incidence of sexual activity, dyspareunia, satisfaction with sex life, amenorrhea, and dysmenorrhea when comparing female patients pre- and post-LT[58]. A meta-analysis investigating the effect of LT on posttransplant quality of life reported significant improvements in sexual function after LT compared to the pre-LT state[59].
Risk of immunosuppression during pregnancy
All LT recipients are on post-transplant immunosuppression in order to decrease the risk of organ rejection. All immunosuppressive agents are known to cross theplacenta and can enter thefetal circulation, with a possibility of resulting in deleterious fetal outcomes. However, there is evidencesuggesting that the use of immunosuppressive agents, such as asazathioprine and cyclosporine, during pregnancy was not associatedwith a significantly increased risk of birth defects[42,60]. In fact, an analysis of the National Transplantation Pregnancy Registry showed that the incidence of birth defects among live births with cyclosporine exposure was 4.9% and with tacrolimus exposure was 4.2%, which are comparable to the 3%-5% incidence in the general population of the United States[61]. On the other hand, data support that exposure to mycophenolic acidin uteroresulted in a 24% incidence of birth defects and in a significant increase of spontaneous abortions[62,63]. Common immunosuppression medication regimens used after LT and their potential adverse maternal and fetal outcomes are shown in Table 2[64,65]. In a recent meta-analysis[66], the most commonly used immunosuppressive agents after LT in pregnant womenwere tacrolimus (60%), sirolimus (27%), cyclosporine (20%), azathioprine (16%), and mycophenolate mofetil (3%). On meta-regression, the authors showed that sirolimus was less likely to lead to a live birth[66].
Mycophenolate mofetil is a commonly administered anti-proliferative agent that is used mostly as a second-line immunosuppressant in adults. There is a growing body of evidence suggesting that the use of mycophenolate mofetil in the first trimester can lead to spontaneous abortion (33%-45%) and congenital malformations (e.g.,cleft lip and palate)[67]. Therefore, mycophenolate mofetil and sirolimus are currently contraindicated in pregnancy[5]. A study showed that patients on cyclosporine were more likely to develop renal dysfunction than patients on tacrolimus[42], while another study showed that premature delivery and cesarean section were more commonly reported in patients on tacrolimus than on cyclosporine[68]. Calcineurin inhibitors (cyclosporine and tacrolimus) are generally considered safe during pregnancy, but the data in LT recipients are scarce[69-71]. The decision on the immunosuppressive regimen for the pregnant LT recipient is challenging and should always be made in accordance to maternal allograft function and after a thorough risk-benefit analysis. Regardless of the choice of immunosuppression regimen, it is recommended that maternal and fetal care is prioritized by obtaining frequent serial medication levels to assure therapeutic levels and to assess hepatic function, while avoiding toxicity. The Food and Drug Administration has graded the commonly used immunosuppressive regimens as shown in Table 2[72]. Since there is a risk of pregnancy while an LT recipient is still on immunosuppressive therapy, it is very important for the patient to be well-informed about the detrimental effects of these medications on the fetus and the mother[73].

Table 2 Potential adverse maternal and fetal outcomes of immunosuppressive medication in pregnant liver transplant recipients
Outcomes of pregnancy after LT
According to the available evidence, LT recipients have not been reported to experience higher rates of maternal mortality compared to the non-transplant population[64]. Studies examining the outcomes of pregnancy post-LT reported that the rate of graft rejection during pregnancy varies between 0%-20%[47,64]. Data have suggested the following to besignificant predictors of graft rejection during pregnancy: Age < 18 years at LT, Caucasian race, anddiagnosis of viral hepatitis[53]. Although there is no compelling evidence to date, studies suggest that a minimum of 1 year should pass after LT before considering pregnancy to allow for stabilization of graft function and immunosuppression requirements[67,74].
In a review article by Parharet al[64], pregnancy-induced hypertension was reported in 2%-43%, pre-eclampsia in2%-22%, and gestational diabetes mellitus in 0%-37.5%. In a more recent meta-analysis, the respective rates were 18.2%, 12.8%, and 7%, while eclampsia was observed in 2% of all post-LT pregnancies[66].
Generally, the rate of cesarean delivery is higher in LT recipients compared to the general non-transplant population (20%-100%), and a plausible explanation may be the higher rates of hypertension and pre-eclampsia during pregnancy[64]. Data from a meta-analysis showed that cesarean delivery and vaginal delivery are performed at similar rates in LT recipients (42.2% and 42.4%, respectively)[66]. Moreover, pre-term birth is seen in 27.8% of post-LT pregnancies[66]and ranges between 12.5%-50%[64].
The majority of pregnancies in LT recipients have a positive outcome, with a high rate of live births (fixed-effects meta-analysis: 77%, random-effects meta-analysis: 86%)[66]. Evidence suggests that the indication for LT is generally not associated with adverse pregnancy outcomes, except for Wilson’s disease, which has been associated with lower live birth rates[66]. However, 7.8% of LT recipients experience miscarriage, 5.7% abortion, 3.3% stillbirth, and 1.7% ectopic pregnancy[66]. Fetal distress is more often seen in LT recipients (10.3%-40%), while low birth weight (< 2500 g) is anotherfrequent complication (4.8%-57%)[64]. On the other hand, congenital abnormalities are relatively uncommon, and the rate is only slightly increased compared to that of the non-transplant population (0%-16.7%)[64].
As expected, designing a study evaluating the long-term outcomes of children born to LT recipients is challenging, and thus the data on long-term pediatric outcomes are scarce. Wuet al[43]followed six children until the age of 4 years, and reported that all of them had achieved all appropriate milestones and had normal physical and psychological development. Villeet al[75]followed children for longer varied periods (3 mo to 5 years post-partum), andno abnormal physical development, adrenal or respiratory insufficiency, or lymphopeniawas reported.
The data from the National Transplantation Pregnancy Registry for about 2000 solid organ transplant recipients indicate favorable outcomes forLT recipients compared to other solid organ transplant recipients (Table 3)[76].
Breastfeeding
The benefits of breastfeeding are well-described, particularly regarding the immunologic components of colostrum and breast milk. However, certain factors should be considered in LT recipients, as immunosuppressive medication are present in breast milk[77]. The levels of such medication in breast milk arelower than those during pregnancy, and hence the risk is slightly decreased (i.e.only 0.1% of eachsteroid dose reaches the breast milk)[78]. In fact, maternal use of prednisone during breast-feeding is allowed according to the American Academy of Pediatrics[79]. An analysis of the National Transplantation Pregnancy Registry showed that among 23 breast-feeding mothers of 29 infants (22 exposed to tacrolimus, three exposed to cyclosporine, four exposed to cyclosporine USP) gestational age was 26-41 wk and birth weight was 680-4097 g, while no serious adverse events were reported[77]. Currently, breast-feeding is not contraindicated in LT recipients on tacrolimus or cyclosporine. Additionally, there is not sufficient evidence to suggest that breastfeeding should be contraindicated in LT recipients on azathioprine[78,79]. Nevertheless, it is advised that when the mother is on tacrolimus, cyclosporine, corticosteroids, or azathioprine, the infant’s serum levels be monitored after the initial 1-2 wk of breastfeeding, as earlier may be due toin uteroexposure or levels from colostrum, and if significantly high, breastfeeding should cease[77]. Lastly, caution is warranted for medication of uncertain safety profile, including betalacept, sirolimus, and everolimus[77].
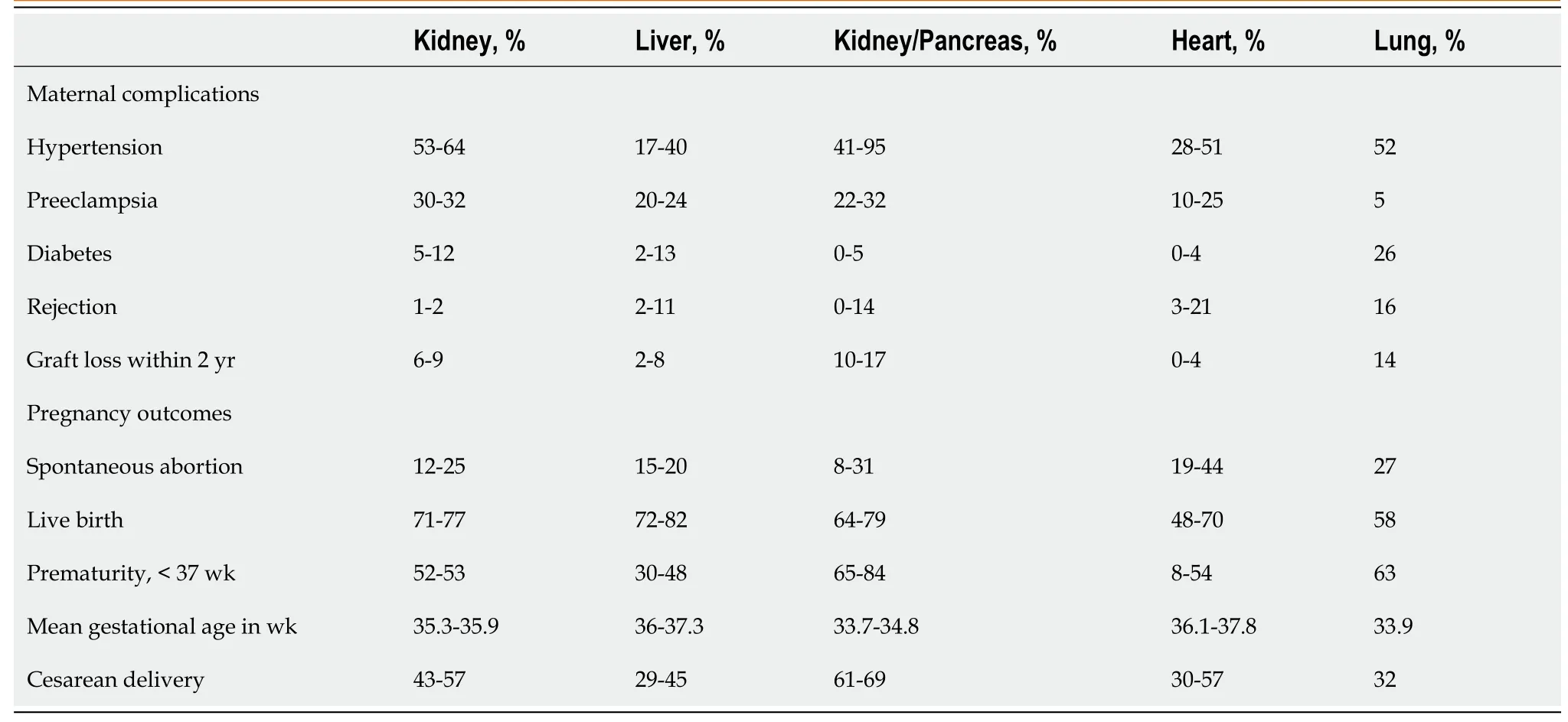
Table 3 National Transplantation Pregnancy Registry maternal and neonatal outcome data according to transplanted organ type[76]
CONCLUSION
In conclusion, an increasing number of LTs in the United States are being performed in women of childbearing age. Several indicationsnecessitatingLT as an intervention mayinclude pregnancy-specific (e.g., acute fatty liver of pregnancy and hemolysis, elevated liver enzymes, low platelet count syndrome)or pre-existing conditions (e.g., alcoholic or non-alcoholic liver disease). However, careful consideration is warranted in such cases as the maternal and fetal outcomes may be dismal. On the contrary, pregnancy outcomes in LT recipients are favorable, and newborns to pregnant LT recipients are relatively healthy. Discussions on pregnancy should be part of theregular pre-LT consultations in all females of childbearing potential. Current recommendations suggest an interval of at least 1-2 years after successful LT before considering pregnancy. All pregnant LT recipients should be managed by a multidisciplinaryteam, including both an obstetrician and a transplant hepatologist. As adverse fetal outcomes may occur more often than in the non-transplant population, early planning or delivery either through a planned induction of labor or cesarean sectionmightbecritical to minimize the risk of complications. Future studies examining long-term pregnancy-related outcomes of LT recipients and their children could advance the current state of knowledge.
杂志排行
World Journal of Transplantation的其它文章
- Torque teno virus in liver diseases and after liver transplantation
- Lenvatinib as first-line therapy for recurrent hepatocellular carcinoma after liver transplantation: Is the current evidence applicable to these patients?
- Donor-specific cell-free DNA as a biomarker in liver transplantation: A review
- Extracellular vesicles as mediators of alloimmunity and their therapeutic potential in liver transplantation
- Intraoperative thromboelastography as a tool to predict postoperative thrombosis during liver transplantation
- Exploring the safety and efficacy of adding ketoconazole to tacrolimus in pediatric renal transplant immunosuppression
