肌瘤粉碎机降低隐匿性子宫平滑肌肉瘤的无病生存期
2020-12-14丁超张英丽朱笕青
丁超 张英丽 朱笕青
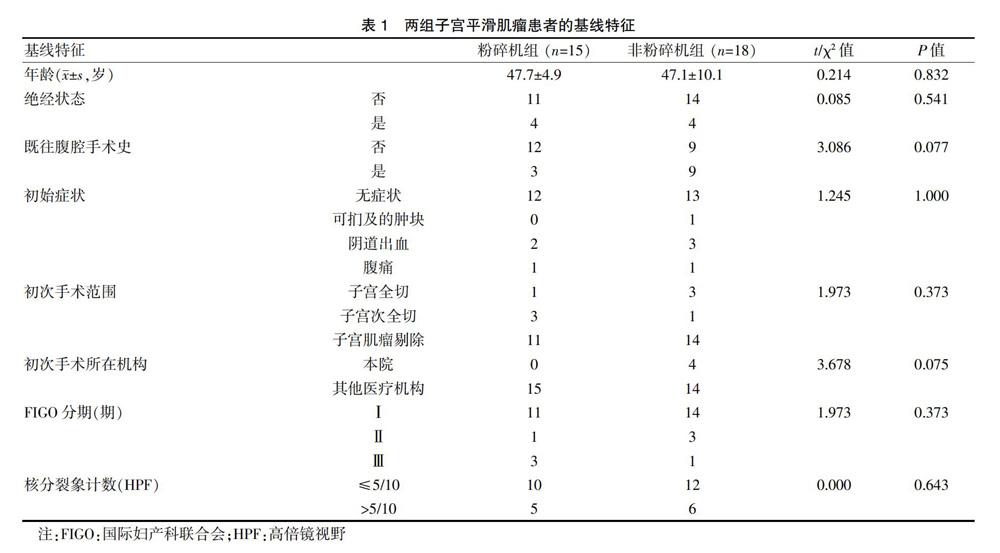
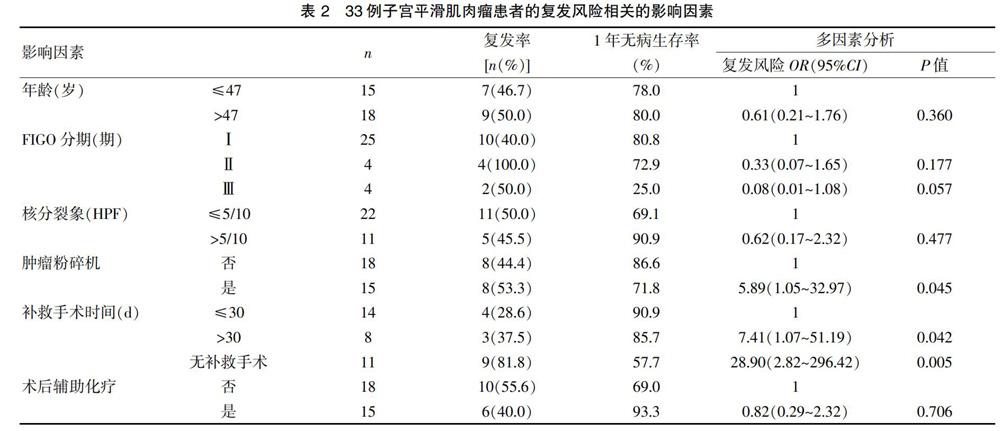
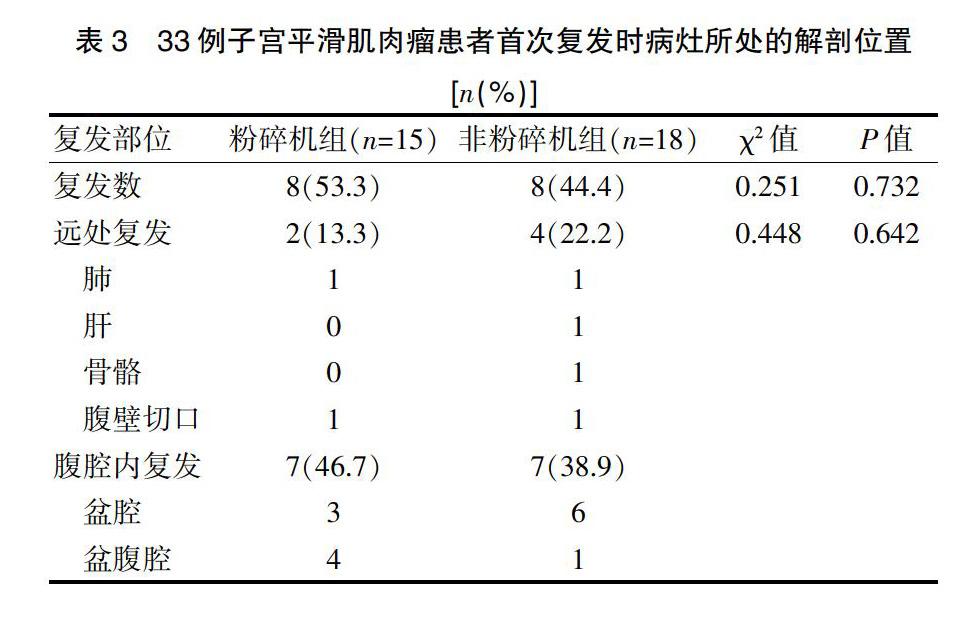
[摘要] 目的 评估腹腔镜手术中肌瘤粉碎机应用对隐匿性子宫平滑肌肉瘤患者的治疗结局所造成的影响。 方法 2008年1~12月共有33例隐匿性的、连续的子宫平滑肌肉瘤患者入组、随访(粉碎机组15例,非粉碎机组18例),观察指标为年龄、绝经状态、FIGO分期、核分裂象、补救性手术时间、是否行术后辅助化疗、随访情况(包括复发时间、复发部位)。结局指标为复发率、1年无病生存率与复发风险的比值比。 结果 肌瘤粉碎机的应用显著降低子宫平滑肌肉瘤患者无病生存期(P=0.045)。不做补救性手术(P=0.005)或者大于30 d后再做补救性手术(P=0.042)的无病生存期均显著地短于30 d以内做补救性手术。患者年龄、FIGO分期、核分裂象、术后辅助化疗等因素均与无病生存期无关。结论 腔镜中应用肌瘤粉碎机会显著减少隐匿性子宫平滑肌肉瘤患者无病生存期。对于这些患者,初次手术后及早做补救性手术,可以显著改善预后。
[关键词] 平滑肌肉瘤;子宫恶性肿瘤;粉碎机;子宫肌瘤剔除
[中图分类号] R737.33 [文献标识码] B [文章编号] 1673-9701(2020)29-0093-05
[Abstract] Objective To evaluate the effect of the application of myoma pulverizer in laparoscopic surgery on the treatment outcome of patients with occulted leiomyosarcoma of uterus. Methods Thirty-three cases of occulted and continuous leiomyosarcoma from January to December 2018 were enrolled and followed up (15 cases in pulverizer group and 18 cases in non-pulverizer group). The observation indicators were age, menopausal status, FIGO stage, nuclear fission, time of remedial surgery, whether adjuvant chemotherapy was performed after surgery, and follow-up (including recurrence time and recurrence site). Outcome measures were the recurrence rate, 1-year disease-free survival rate, and the odds ratio of recurrence risk. Results The application of myoma pulverizer can significantly reduce the disease-free survival of patients with uterine leiomyosarcoma(P=0.045). The disease-free survival of patients without remedial surgery(P=0.005) or with remedial surgery after more than 30 days(P=0.042) was shorter than that of patients with remedial surgery in 30 days. Age, FIGO stage, nuclear fission, and postoperative adjuvant chemotherapy were not associated with disease-free survival. Conclusion Endoscopic use of myoma pulverizer can significantly reduce disease-free survival in patients with occulted leiomyosarcoma of the uterus. For these patients, early remedial surgery after the initial operation can significantly improve the prognosis.
[Key words] Leiomyosarcoma; Uterine malignant tumor; Pulverizer; Myomectomy
子宮肉瘤是一种较为少见的子宫实体恶性肿瘤,约占女性生殖系统恶性肿瘤的3%[1]。子宫平滑肌瘤的肉瘤恶变率为0.13%~0.81%[2]。子宫平滑肌肉瘤(Uterine leiomyosarcoma,LMS)为子宫肉瘤的最常见病理类型,占30%~40%[3]。完整的全子宫切除是目前惟一有效的治疗方法。而其他疗法,如化疗、放疗、内分泌治疗、靶向治疗等,疗效均有限[4]。早期LMS没有特异性症状,术前检查很难与子宫平滑肌瘤鉴别[5]。临床上,LMS往往通过术中快速冰冻病理或术后常规病理检查意外发现。
肌瘤粉碎机是一种在腹腔内将肌瘤等较大病灶粉碎成条索状或碎片状,方便从腹腔镜置管孔取出的手术器械,也称为“旋切器”。一些研究显示,肌瘤粉碎机的应用会促进隐匿性LMS的腹腔内播散,并导致较差的预后[6-8]。2014年美国食品药品监督局(FDA)发布声明,认为腹腔镜肌瘤剔除术或者子宫切除术中应用肌瘤粉碎机,会增加癌症医源性扩散的风险,因此需要严格限定肌瘤粉碎机的应用范围[9]。FDA要求肌瘤粉碎机标签新增三条禁忌证:禁止用于子宫肌瘤怀疑恶变的妇科手术,禁止用于围绝经期或者绝经后女性,禁止用于切除组织能从阴道或者微创切口完整取出的手术[10]。但是有研究发现,肌瘤粉碎机所导致的较差预后并差异无统计学意义[11]。两项系统性综述均显示术中意外发现的子宫平滑肌肉瘤患病率很低,分别为1/8300[12]或1/10 000~13/10 000[13],远低于FDA所估计的患病率(1/498)[9]。因此FDA基于过高患病率估计而做出的决定是否科学客观,值得讨论。目前国内仍有很多医疗机构在使用肌瘤粉碎机,比如2017年一项国内研究提到[14],45例腹腔镜肌瘤剔除手术全部采用了肌瘤粉碎机,但未讨论这种器械使用所可能带来的风险。因为隐匿性子宫平滑肌肉瘤的患病率很低,而意外使用肌瘤粉碎机的病例更少,所以国际上对这方面的临床病例研究较少。对这种意外,应该采用哪种补救措施,能对患者的治疗带来获益,这方面的研究更是少之又少。
在國内,这种小概率事件没有引起足够的重视。国内使用肌瘤粉碎机的情况仍较普遍。诚然,肌瘤粉碎机在方便手术医生操作、减少手术时间等方面有积极的作用,“一刀切”完全禁用也不合理。未来可以改进肌瘤的取出方式,例如采用封闭式的粉碎旋切技术,或用取物袋套牢肿瘤并提拉至腹壁小切口,用手术刀切碎取出,或者从阴道穹窿做小切口取出等。1项系统性综述显示,子宫平滑肌肉瘤用肌瘤粉碎机取出瘤体,5年生存率为30%,而改用手术刀切碎取出后,5年生存期与开腹手术将瘤体完整取出的接近,分别为59%与60%[13]。一项随机对照的临床试验显示,对腹腔镜子宫肌瘤剔除术进行改进,将肌瘤标本放在自制标本袋中,再进行粉碎取出,此增加的保护措施理论上可降低意外肉瘤播散风险,但与传统手术相比,手术时间与住院时间并未显著延长[19]。此外,对于绝经前后的妇女,肌瘤短期内增大明显,以及影像学提示恶性可疑的患者,应禁用肌瘤粉碎机。对术中应用肌瘤粉碎机的情况,手术医师需要在术前将相关风险详尽告知患方,得到患方知情同意。
针对于已经发生的肌瘤粉碎机错误应用,或初次手术未行完整的子宫双附件切除的情况,均应该及时行补救性手术。补救性手术方式采用子宫双附件切除,并行彻底的腹腔探查、腹水脱落细胞检查,必要时行腹膜后淋巴结活检或者大网膜切除。Cao等[20]研究显示,初次手术与二次分期手术之间的时间间隔长短对预后并无影响,但本研究发现初次手术后30 d以上再行补救性手术,复发风险是30 d以内补救手术的7.41倍(1.07~51.19倍),而不行补救性手术的复发风险则更高,高达28.90倍(2.82~296.42倍)。既往的文献显示,化疗对肉瘤并不敏感,本次研究也发现术后辅助化疗并未对患者的无病生存期带来获益(P=0.706)。因此,及早、并彻底完整的手术切除,是子宫平滑肌肉瘤治疗的关键所在。
[参考文献]
[1] Olah KS,Gree H,Blunt S,et al. Retrospective analysis of 318 cases of uterine sarcoma[J]. Eur J Cancer,1991,27(9):1095-1099.
[2] Berchuch A,Rubin SC,Hoskins WJ,et al. Treatment of uterine leiomyosarcoma[J]. Obstet Gynecol,1988,71(6 Pt 1):845-850.
[3] Tavassoéli FA,Devilee P. World health organization classification of tumours in:Pathology and genetics of tumors of the breast and female genital organs[M].4th ed. IARC Press:Lyon,2003:62.
[4] Nam JH,Park JY.Update on treatment of uterine sarcoma[J].Curr Opin Obstet Gynecol,2010,22(1):36-42.
[5] Amant F,Coosemans A,Debiec-Rychter M,et al. Clinical management of uterine sarcomas[J]. Lancet Oncol,2009, 10(12):1188-1198.
[6] Anupama R,Ahmad SZ,Kuriakose S,et al. Disseminated peritoneal leiomyosarcomas after laparoscopic myomectomy and morcellation[J]. J Minim Invasive Gynecol,2011, 18(3):386-389.
[7] Park JY,Park SK,Kim DY,et al. The impact of tumor morcellation during surgery on the prognosis of patients with apparently early uterine leiomyosarcoma[J]. Gynecol Oncol,2011,122(2):255-259.
[8] Rekha W,Amita M,Sudeep G,et al. Unexpected complication of uterine myoma morcellation[J]. Aust NZJ Obstet. Gynaecol,2005,45(3):248-249.
[9] USFood and Drug Administration. Quantitative assessment of the prevalence of unsuspected uterine sarcoma in women undergoing treatment of uterine fibroids:summary and key findings[EB/OL]. Maryland:FDA Safety Communication,2014[2020-03-10]. https://www.fda.gov/media/88703/download.
[10] US Food and Drug Administration. Laparoscopic Power Morcellators[EB/OL]. Maryland:FDA Safety Communication,2020-2-25[2020-03-10]. https://www.fda.gov/medical-devices/surgery-devices/laparoscopic-power-morcellators.
[11] Morice P,Rodriguez A,Rey A,et al. Prognostic value of initial surgical procedure for patients with uterine sarcoma:analysis of 123 patients[J]. Eur J Gynaecol Oncol,2003, 24(3-4):237-240.
[12] Pritts EA,Vanness DJ,Berek JS,et al. The prevalence of occult leiomyosarcoma at surgery for presumed uterine fibroids:A meta-analysis[J]. Gynecol Surg,2015,12(3):165-177.
[13] Hartmann KE,Fonnesbeck C,Surawicz T,et al. Management of Uterine Fibroids[M/OL]. Rockville:Agency for Healthcare Research and Qualityj,2017[2020-3-10]. https://www.ncbi.nlm.nih.gov/books/NBK537742/
[14] 何麗娜,李慧,张泽慧. 腹腔镜子宫肌瘤剜除术与开腹子宫肌瘤剜除术的临床效果比较[J]. 中国性科学,2017, 26(12):37-40.
[15] Della BC,Karini H. Endometrial stromal sarcoma diagnosed after uterine morcellation in laparoscopic supracervical hysterectomy[J]. J Minim Invasive Gynecol,2010, 17(6):791-793.
[16] Park JY,Kim DY,Kim JH,et al. The impact of tumor morcellation during surgery on the outcomes of patients with apparently early low-grade endometrial stromal sarcoma of the uterus[J]. Ann Surg Oncol,2011,18(12):3453-3461.
[17] Pritts EA,Parker WH,Brown J,et al. Outcome of occult uterine leiomyosarcoma after surgery for presumed uterine fibroids:a systematic review[J]. J Minim Invasive Gynecol,2015,22(1):26-33.
[18] Lieng M,Berner E,Busund B. Risk of morcellation of uterine leiomyosarcomas in laparoscopic supracervical hysterectomy and laparoscopic myomectomy,a retrospective trial including 4791 women[J]. J Minim Invasive Gynecol,2015,22(3):410e4.
[19] Shi X,Shi L,Zhang S. A comparative study on the short-term clinical efficacy of the modified laparoscopic uterine comminution technique and traditional methods[J]. Mol Clin Oncol,2020,12(3):237-243.
[20] Cao H,Li L,Yang B,et al. Unexpected uterine sarcomas after hysterectomy and myomectomy for presumed leiomyoma:A retrospective study of 26,643 patients[J].Cancer Manag Res,2019,25(11):7007-7014.
(收稿日期:2020-02-09)
