Management of an endoscopy center during the outbreak of COVID-19: Experience from West China Hospital
2020-12-10YuanGaoLianSongYeJiangDuQiongYingZhangBingHu
Yuan Gao, Lian-Song Ye, Jiang Du, Qiong-Ying Zhang, Bing Hu
Abstract Since the outbreak of the coronavirus disease 2019 (COVID-19), various measures have been taken to protect against the infection. As droplet and contact transmission are the main routes of COVID-19 infection, endoscopy centers are considered to be high-risk areas for exposure to COVID-19. We have undertaken several countermeasures in our endoscopic center during the pandemic, and have gained significant experience in terms of prevention and control of COVID-19. We here present our experience and strategies adopted for preventing hospital infection in our endoscopy center during the COVID-19 pandemic. We describe our management of the environment, endoscope, patients, and medical staff, and our self-made masks.
Key Words: COVID-19; Endoscopy center; Management; Hygiene
INTRODUCTION
Since the outbreak of coronavirus disease 2019 (COVID-19) in December 2019, China and many other countries have tried several measures to protect against the spread of infection[1-3]. Although the COVID-19 pandemic in China has been mostly under control[4,5], the number of infected people in European and American countries is noticeably increasing[5,6]. Due to the main routes of droplet and contact transmission[7], endoscopy centers have a high risk of exposure to COVID-19. As the most prestigious endoscopy center in western China, a total of 7135 diagnostic endoscopies and 643 therapeutic endoscopies were performed in West China Hospital from March 1 to April 10, 2020, which included 124 cases of endoscopic retrograde cholangiopancreatography, 55 of endoscopic submucosal dissection, 207 of endoscopic mucosal resection, and 224 of endoscopic ultrasound. Compared with the same period last year, we reasonably arranged the endoscopy schedule and minimized unnecessary endoscopy (Table 1). There were no hospital infections in medical staff and patients. In the current review, we present our experience and strategies adopted for preventing hospital infection in our endoscopy center during the COVID-19 pandemic.
MANAGEMENT OF ENDOSCOPY CENTER
Disinfection of the environment and endoscopes
Endoscopy centers generally have no rooms with negative-pressure laminar flow. Virus transmission might occur because patients undergoing upper gastrointestinal endoscopy cannot wear a mask, and fecal fluid might flow during lower gastrointestinal endoscopy[8]. Thus, disinfection of the environment and endoscopes is important.
Disinfection of the environment:In our center, 500 ppm chlorine-containing disinfectant was applied 1 or 2 times/d for disinfecting the surface of equipment and the ground. Doorknobs and chairs were wiped and disinfected with 1000 ppm chlorine-containing disinfectant for 2 or 3 times/d. Secretions were removed immediately, and the areas wiped with 2000 ppm chlorine-containing disinfectant. Natural ventilation was performed continuously.
Disinfection of the operation room:Here, 1000–2000 ppm chlorine-containing disinfectant was applied at least 2 times/d for ground disinfection. Disinfection with 75% alcohol was used for consoles and monitors. Electrosurgical workstations and treatment beds were wiped with 75% alcohol before and after each procedure. Disposable bedspread and pillowcases were used for each patient. An automatic air disinfection machine was applied in the operating room twice daily (05:00–7:00 and 19:00–21:00 h). Continuous ventilation was conducted using a fresh air ventilation system during working hours.
Disinfection of the resuscitation room:Surfaces of monitors and other instruments were wiped with 75% alcohol for disinfection. Additionally, sofas were wiped and disinfected with 1000–2000 ppm chlorine-containing disinfectant for 1 or 2 times/d. Floors were mopped with 1000–2000 ppm chlorine-containing disinfectant for 1 or 2 times/d. An automatic air disinfection machine was used for air disinfection in the operation room twice daily (05:00–7:00 and 19:00–21:00 h). Continuous ventilation was performed using a fresh air ventilation system during working hours.
Disinfection of the office area:The doorknobs in office areas were wiped and disinfected with 75% alcohol for 2–4 times/d. The desktops, chairs and cabinet surfaces were wiped and disinfected with 1000 ppm chlorine-containing disinfectant. The floor was mopped and disinfected with 1000 ppm chlorine-containing disinfectant. Continuous ventilation was carried out using a fresh air ventilation system during working hours.
Disinfection of the endoscopes:After preprocessing, the endoscope was immersed into a container with 0.2%–0.35% peracetic acid for predisinfection. Instruments should also be predisinfected using the solution with 0.2%–0.35% peracetic acid solution. Then, the endoscope was placed in a special container, sealed, and transferred to a clean and disinfected room. Standard cleaning and disinfection procedures were carried out after 10 min. Finally, total ethanol perfusion with 75% alcohol and full sterilization with 0.2%–0.35% peracetic acid were done before theapplication of endoscope to the next patient.

Table 1 Endoscopy indigestive endoscopy center of West China Hospital during the COVID-19 pandemic
After daily cleaning and disinfection, the cleaning tank, rinsing tank, perfusion device, and cleaning brush were thoroughly cleaned and disinfected with 0.2%–0.35% peracetic acid.
Enhancing access management system
Three special channels with eye-catching signs were set up, for entrance and exit of medical staff as well as patients. Dedicated staff were appointed for managing these channels and recording related information.
Entrance and exit channels for medical staff:Measurement of medical staff’s body temperature was undertaken before their entrance into a specific channel. In our center, staff without fever (< 37.3ºC) were allowed to enter the endoscopy center, and protective equipment, such as disposable mask, hat, and surgical gown were provided. The body temperature of the staff was measured again when they left work.
Entrance channel for patients:Patients who underwent secondary screening (see below) were allowed to enter our endoscopy center. Family members had no access to the endoscopy center. Entrance was permitted for one family member only if the patient was in serious condition.
Exit channel for patients:Patients who received endoscopic intervention had to leave the endoscopy center through an exit channel. Patients’ entrance was prohibited as well.
MANAGEMENT OF PATIENTS WITHOUT EMERGENCY
Prehospital management
Appointment scheduling for patients:Personal mobility and gathering might increase the risk of coronavirus transmission. Diagnostic appointment scheduling for asymptomatic patients without warning signs (e.g., unexplained weight loss), and therapeutic plans for patients with mild illness (e.g., small colorectal polyps) should be delayed. The appointment should be arranged according to the potential severity of illness. Priority should be given to patients who are old, frail, children, have a history of taking immunosuppressants, have diabetes, or to other immunocompromised patients. In our center, all patients were informed about the risk of virus infection, if they would like to receive endoscopy during the outbreak.
Patient survey and preparation prior to endoscopy:Dedicated staff contacted patientsviatelephone within 2 wk before their scheduled appointment, and inquired about the presence of the following symptoms and epidemiological history. Symptoms mainly included new-onset fever, cough, loss of appetite, and diarrhea. Epidemiological histories included residency in high-risk areas within 2 wk, and history of contact with COVID-19 patients and suspected cases within 2 wk. Patients with any of these symptoms and epidemiological history were referred to the fever clinic, and endoscopy was performed only after ruling out COVID-19 infection. More than 30 patients reported fever during telephone consultation, and they were ruled out for COVID-19 infection before undergoing endoscopy. Patients without these suspicious symptoms or epidemiological history also have to undergo chest computed tomography (CT) 3–5 d prior to endoscopy. Study showed that chest CT had a low rate of missed diagnosis of COVID-19 (3.9%, 2/51) and thus it can be used as a standard method for diagnosis of COVID-19 based on CT features and transformation rules[9]. Rapid diagnosis can control the potential spread early and optimize patient management. During the outbreak, a male patient with history of contact with people from Hubei Province was confirmed with COVID-19 after undergoing chest CT and following virus detection, although he declared suspicious symptoms during telephone inquiry. Our strategy aimed to prevent the transmission of the virus from such atypical patients.
Intrahospital management
We implemented a three-level screening strategy for patients who received endoscopy during the COVID-19 pandemic (Figure 1).
Primary screening in the gate of the main building:All patients had to wear face masks, and only patients without fever were allowed to enter the building. Dedicated staff rechecked the body temperature and investigated the epidemiological history of patients with fever. These patients were sent to the fever clinic outside the building, and were guided by the staff.
Secondary screening in the gate of endoscopy center:The body temperature, symptoms, epidemiological history, and the results of chest CT of each patient were recorded and checked. Patients without fever and epidemiological history, and with normal chest CT findings within 3–5 d were allowed to enter the endoscopy center for endoscopic operation after disinfection of their hands using alcohol-based hand rubs. With the gradual easing of the pandemic, the time requirement for chest CT can be extended to 2 wk before examination. Suspected patients were sent to the fever clinic for further examination, and guided by staff, while confirmed patients were quarantined in a special isolated ward.

Figure 1 Workflow of digestive endoscopy during the COVID-19 pandemic. COVID-19: Coronavirus disease 2019.
Tertiary screening in the operating room:When patients arrived at the operating room of the endoscopy center, an endoscopist and a nurse rechecked the information recorded by the secondary screening. Suspected patients were sent to the fever clinic, and guided by the staff, while confirmed patients were quarantined in a special isolated ward. The endoscopic operation was then carried out as usual for unsuspected patients.
Posthospital management:Follow-up was conducted when patients left our center. Dedicated staff contacted the patientsviatelephone and recorded any abnormalities. If a patient was diagnosed with COVID-19 during the follow-up period, all the related medical staff had to stop working, and be quarantined at their respective homes for at least 2 wk. Related patients would be contacted and quarantined as well.
MANAGEMENT OF MEDICAL STAFF
The work plan was adjusted according to the number of appointed patients, and with minimized medical staff on duty. All endoscopists, nurses, and healthcare personnel were trained in terms of infection control, as well as utilizing personal protective equipment properly during endoscopy (Table 2). All staff had to daily report and record their symptoms and epidemiological history. Staff with fever or epidemiological history of exposure were referred to the fever clinic and were quarantined. Four medical staff of our endoscopy center were under home quarantine for 14 d due to confirmed cases in their community.
Before daily working
All medical staff had to change their personal clothes and wear a gown before entering the endoscopy center. They had to enter the main building through a channel different from patients after measuring their body temperature. Before meeting patients, medical staff had to perform hand hygiene, and wear a disposable surgical gown, with a face mask, hat, goggles, gloves, and protective shoe covers.
During daily working
The symptoms and epidemiological history of patients were rechecked before further intervention. Staff had to maintain a distance from each patient in the explanation step before starting endoscopic intervention. Hands had to be washed before and after contact with each patient, after contact with a potential source of infection, and before and after wearing and removing personal protective equipment, including gloves[10].Three levels of protection were required in case of exposure to respiratory secretions, such as tracheal intubation, airway care, and sputum aspiration for general patients, as well as during performing any endoscopic procedure on confirmed or suspected COVID-19 patients[11]. The tissue samples obtained during endoscopy were stored in a fixed area and the endoscopy report was provided to avoid cross-infection.

Table 2 Prevention and control measures for each location
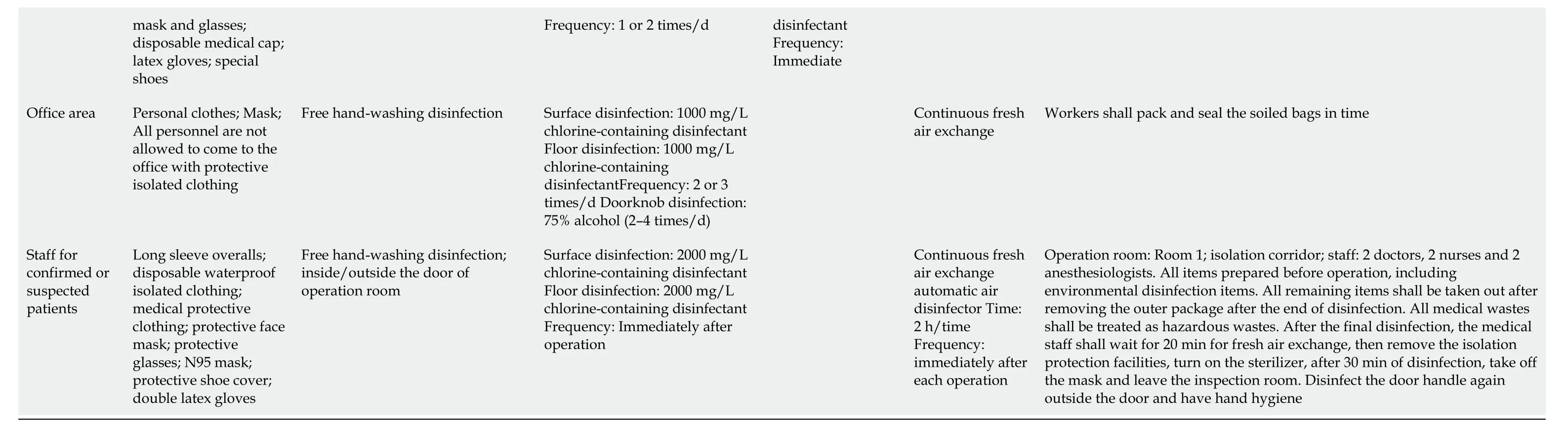
mask and glasses; disposable medical cap; latex gloves; special shoes Frequency: 1 or 2 times/d disinfectant Frequency: Immediate Office area Personal clothes; Mask; All personnel are not allowed to come to the office with protective isolated clothing Freehand-washingdisinfection Surface disinfection: 1000 mg/L chlorine-containing disinfectant Floor disinfection: 1000 mg/L chlorine-containing disinfectantFrequency: 2 or 3 times/d Doorknob disinfection: 75% alcohol (2–4 times/d)Continuous fresh air exchange Workers shall pack and seal the soiled bags in time Staff for confirmed or suspected patients Long sleeve overalls; disposable waterproof isolated clothing; medical protective clothing; protective face mask; protective glasses; N95 mask; protective shoe cover; double latex gloves Freehand-washingdisinfection; inside/outside the door of operation room Surface disinfection: 2000 mg/L chlorine-containing disinfectant Floor disinfection: 2000 mg/L chlorine-containing disinfectant Frequency: Immediately after operation Continuous fresh air exchange automatic air disinfector Time: 2 h/time Frequency: immediately after each operation Operation room: Room 1; isolation corridor; staff: 2 doctors, 2 nurses and 2 anesthesiologists. All items prepared before operation, including environmental disinfection items. All remaining items shall be taken out after removing the outer package after the end of disinfection. All medical wastes shall be treated as hazardous wastes. After the final disinfection, the medical staff shall wait for 20 min for fresh air exchange, then remove the isolation protection facilities, turn on the sterilizer, after 30 min of disinfection, take off the mask and leave the inspection room. Disinfect the door handle again outside the door and have hand hygiene
After daily working
Medical staff took off their disposable items in the exit channel, and put them in the medical waste bin. To save materials, we did not discard all protective materials after each operation. We changed gloves and disinfected hands after each operation. Other protective equipment was not be replaced if there was no secretions or splashes. A seven-step hand-washing method was applied. Body temperature was recorded before leaving the endoscopy center. Staff changed from their gown to personal clothes, and put the gown in a specific tub. When off duty, staff stayed indoors and cooperated with the epidemic prevention management of the community. The manager of the endoscopy center communicated with the hospital management team closely and regularly, monitored the outbreak closely, and changed the plans quickly to deliver sustainable and effective endoscopy services.
SELF-MADE ISOLATED MASK FOR UPPER GASTROINTESTINAL ENDOSCOPY
Based on the concept that patients with air-borne infectious disease should be isolated in negative pressure wards in order to prevent infection[8], a fully-enclosed “isolated mask” for patients undergoing upper gastrointestinal endoscopy was developed. The mask provided both oxygen inhalation and negative pressure (for suction of patients’ expulsion from mouth and nose) (Figures 2 and 3). The end of the mask cannula could be freely closed with a unidirectional flap at the entrance, which was fixed on the inside of the cannula to prevent patients’ expulsion from overflowing. There were two separate windows on the left and right sides of the mask bulge. One window was reserved for the oxygen tube, and the other was used for negative pressure suction.
The size of the window aperture was the same as the diameter of the tube, and it was sealed tightly. After the mask was inflated, it closely fitted the patient’s face to avoid expulsion leakage. The oxygen inhalation flow rate was adjusted to 6–8 L/min. The suction tube was connected to the central negative pressure system and the aspirated liquid (gas) was continuously removed to the hospital waste liquid (gas) treatment center. We have applied this isolated mask to 162 patients for respiratory isolation during upper gastrointestinal endoscopy (Figure 4). The gastroscopy process was smooth and the vital signs of the patients remained stable during and after the operation. No hospital infection occurred in our endoscopy center.
CONCLUSION
Our endoscopy center achieved effective epidemic prevention and undertook much diagnostic and therapeutic work during the COVID-19 pandemic. Several factors influenced the outcome of this management. First, experienced personnel led the overall situation and laid the foundation for success. We established a special prevention and control group at the beginning of the pandemic: The director as the team leader, the head nurse as the deputy team leader, and the infection control nurse and anesthetic medical team leader as the backbone. We quickly started our emergency procedures and adjusted the working mode in time: Delayed ordinary endoscopy, reduced the flow and aggregation of people, and kept special channels for patients with emergencies. In addition, we implemented a three-level screening mechanism and strengthened personnel access management. We improved the cleaning and disinfection of endoscopes and the environment. We formulated standards for pandemic protection in our endoscopy center, strictly implemented the health supervision of employees, and trained all staff in the use of personal protective equipment. Finally, although not used in large quantities, our innovative isolated mask played an important role. Our strategies may provide a comprehensive management for endoscopy centers during the COVID-19 pandemic.
As an infectious disease mainly transmitted by respiratory tract and contact, COVID-19 has its own special characters. The COVID-19 pandemic has attracted unprecedented global concern, which needs global unity. COVID-19 is transmitted from respiratory secretions, feces, and contaminated environmental surfaces. In addition, the virus is spread not only by patients with symptoms but also by asymptomatic individuals[9]. However, control of the pandemic can be realized through reasonable prevention and management. Other infectious diseases with the same or similar route of transmission can be managed by this method in medical environments with high risk of exposure, such as endoscopy centers. Some parts of this strategy (like three-level screening) can also be applied in community hospitals, which generally provide no endoscopic procedures for patients.
In conclusion, further protection of patients and medical staff is required during the outbreak of COVID-19 or other infectious diseases. We share our experience to provide valuable information for China and other countries that are suffering from the COVID-19 pandemic.

Figure 2 Outside surface of the mask.

Figure 3 Inside surface of the mask.

Figure 4 Use of mask during endoscopy.
杂志排行
World Journal of Gastroenterology的其它文章
- Role of betaine in liver disease-worth revisiting or has the die been cast?
- Gastrointestinal complications after kidney transplantation
- Is vitamin D receptor a druggable target for non-alcoholic steatohepatitis?
- Acetyl-11-keto-β-boswellic acid inhibits proliferation and induces apoptosis of gastric cancer cells through the phosphatase and tensin homolog /Akt/ cyclooxygenase-2 signaling pathway
- Endogenous motion of liver correlates to the severity of portal hypertension
- Longitudinal decrease in platelet counts as a surrogate marker of liver fibrosis
