Titanium miniplates across the fourth and fifth carpometacarpal joints for coronal fractures of the hamate
2020-12-03SUNLiyingYANGYongLIZhongzheTIANWen
SUN Li-ying, YANG Yong, LI Zhong-zhe, TIAN Wen
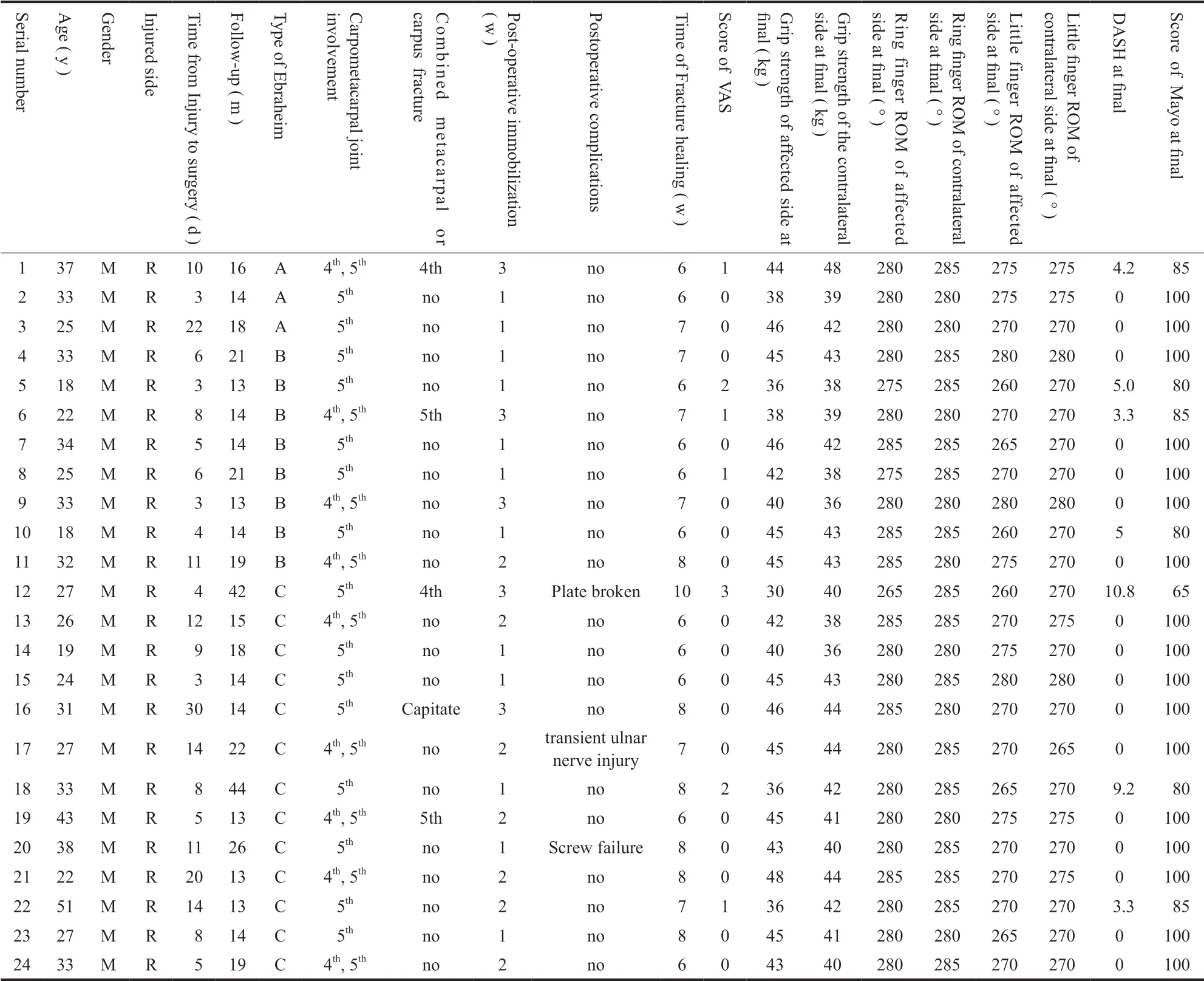
【Abstract】 Objective To evaluate the result of coronal fractures of the hamate with titanium miniplates across the fourth and fifth carpometacarpal joints. Methods From December 2011 to September 2018, 24 patients with coronal fractures of the hamate were managed with titanium miniplates across the carpometacarpal joints. All patients were males with an average age of ( 29.6 ± 7.9 ) years ( range: 18 - 51 years ). Ebraheim's classification of hamate fractures: 3 cases were of type A, 8 type B, and 13 type C. All fractures were exposed using the dorsal approach.After reduction, the fractures were fixed with titanium miniplates crossing the carpometacarpal joints dorsally. The Disabilities of the Arm, Shoulder and Hand ( DASH ), Visual Analogue Scale ( VAS ), MAYO Wrist Score, grip strength, and TAM ( total active motion ) of ring and little fingers were recorded to evaluate outcomes. Results All 24 patients were followed up for 13 - 44 months ( mean: 18.5 ± 8.3 months ). Hamate fractures healed within 6 -10 weeks ( mean: 6.9 ± 1.1 weeks ). Except two cases, all titanium miniplates and screws were removed at 3 to 6 months after surgery. Evaluation indexes at the final follow-up: DASH scores 0 - 10.8 ( mean: 1.7 ± 3.1 ); VAS 0 - 3 ( mean:0.5 ± 0.9 ); MAYO wrist scores 65 - 100 ( mean: 94.2 ± 10.0 ); grip strength ( 42.0 ± 4.4 ) kg on the injured side and( 41.1 ± 2.8 ) kg on the contralateral side; TAM of the ring and little fingers ( 281 ± 3 ) °, ( 271 ± 6 ) ° on the injured side, while ( 283 ± 3 ) ° and ( 272 ± 4 ) ° on the contralateral side; No statistical differences in the grip strength and TAM between the two sides. Conclusions Coronal fractures of the hamate can be fixed with titanium miniplates crossing the carpometacarpal joints. This procedure can provide stability and allow early motion, which in turn helps maintain joint reduction and obtain good hand functions.
【Key words】 Hamate bone; Fractures, bone; Fracture fixation, internal; Carpal bones
Introduction
Hamate fractures are relatively common among wrist fractures. In 1934, Milch first classified hamate fractures into body and hook fractures[1]. The most common hamate body fracture is the coronal plane fracture, which is usually caused by a hard strike to walls or the ground with a fist. Stable fractures with no obvious displacement can be treated conservatively, with immobilization. However, unstable fractures, fractures with obvious displacement, especially hamate body fractures combined with carpometacarpal subluxation /dislocation require surgical intervention[2-5].
Currently, closed reduction with percutaneous Kirschner wire fixation, open reduction with Kirschner wires and screw fixation are the commonly used surgical techniques. Kirschner wire fixation is not strong enough and subluxation may persist or recur in the postoperative period. Wharton et al[2]. reported that among patients who had Kirschner wire fixation, the rate of subluxation of the carpometacarpal joint was 33.3% at final follow-up. Hamate is mainly a cancellous bone and screw fixation alone may be strong enough, but early range of motion exercises are not possible and screw back out with recurrence of subluxation is a distinct possibility. Treatment of coronal plane fractures of the hamate body needs accurate anatomical reduction to restore the smooth articular surface while obtaining a strong fixation. This will allow us to start range of motion exercises and avoid carpometacarpal joint subluxation. However, the most commonly used surgical methods cannot meet the above requirements. There are certain advantages in using a titanium miniplate across the carpometacarpal joints after open reduction. The titanium miniplate itself can buttress and fix the fracture.Meanwhile, the carpometacarpal joints can be firmly fixed to avoid subluxation. In theory, this should be a reasonable fixation method for coronal plane fractures.
We treated 24 cases of coronal plane fractures of the hamate body between December 2011 and September 2018 using titanium miniplates across the carpometacarpal joints. This is a retrospective study with the aim of: ( 1 ) analyzing different types of injury mechanisms causing coronal fractures of the hamate body; ( 2 ) improving diagnosis and differential diagnosis of this type of fractures; ( 3 ) describing our surgical techniques and outcomes.
Materials and Methods
Inclusion and exclusion criteria
From December 2011 to September 2018, patients with a closed coronal fracture of the hamate body were included in the study. All patients were over 18 years old and injured less than one month.
Patients with open fractures, associated soft tissue injury ( vessel / nerve / tendon ) in both upper limbs,deformity of the affected upper limbs, anesthesia and surgical contraindications in preoperative examinations,or less than 12 months' follow up were excluded from the study.
Patient information
A total of 24 patients fit the inclusion criteria.All of them were male with an average age of ( 29.6 ±7.9 ) years ( range: 18 - 51 years ). The mean time between injury to operation was ( 9.3 ± 6.8 ) days( range: 3 - 30 days ). Pain, swelling and stiffness were observed on the ulnar side of the wrist with an obvious dorsal protuberance. Decreased grip strength was observed as well ( Tab.1 ).
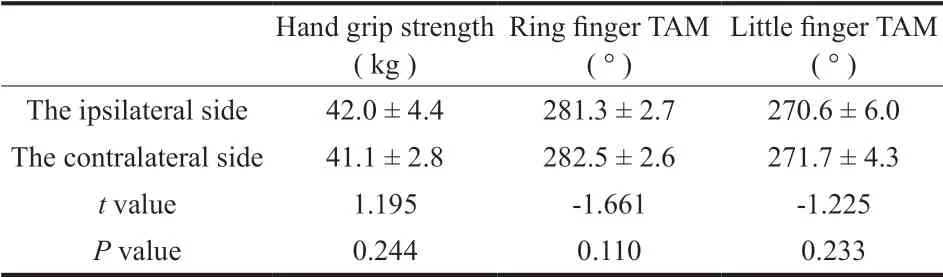
The method developed by Ebraheim et al[6]. was used to type the hamate body coronal plane fractures( Fig.1 ). Type A fracture line is through the coronal plane and the middle of the hamate body. Type B fracture line is oblique from the far end of the middle of the hamate body leading to the dorsal side and involving most of the carpometacarpal joint surface. Type Cfracture is an avulsion fracture of the distal dorsal edge of the hamate, which is usually complicated with dorsal carpometacarpal joint dorsal subluxation / dislocation[6].In this group of patients, Type A, B, and C fractures were seen in 3, 8, and 13 cases, respectively. In addition,4 patients had concomitant fourth or fifth metacarpal shaft or metacarpal base fracture, and 1 patient had a capitate fracture.
Tab.1 Postoperative hand grip strength and the total active motion( TAM ) of the ring finger and little finger
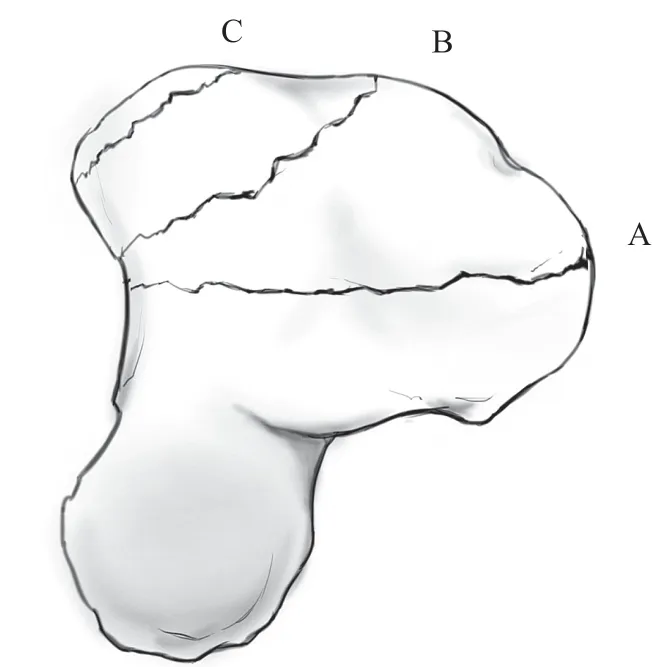
Fig.1 Types of hamate coronal plane fractures by Ebraheim et al( Type A fracture has the fracture line through the coronal plane and the middle of the hamate body. Type B fracture has an oblique fracture line from the far end of the middle of the hamate body leading to the dorsal side and involving most of the carpometacarpal joint surface.Type C fracture is an avulsion fracture of the distal dorsal edge of the hamate, which is usually complicated with dorsal carpometacarpal joint lateral dislocation )
Imaging examination
Routine wrist X-ray examination was obtained including anteroposterior, lateral, and 30° pronation views. The “not parallel” sign in the metacarpals on the lateral view of the wrist is an important indirect sign for the diagnosis of hamate body fracture and a direct sign for carpometacarpal joint dislocation ( Fig.2 ). Further computed tomography ( CT ) examination of the wrist can confirm the type of the hamate body fracture and the details of the dislocation.
Surgical methods
Brachial block was used with the patient supine and the upper limb on a hand table. An arm tourniquet was used ( pressure 280 mm Hg ). A longitudinal skin incision was made centered over the fifth carpometacarpal joint. The dorsal vein and the dorsal branches of the ulnar nerve were exposed and protected.The extensor digiti minimi was freed and retracted to the radial side to fully reveal the hamate body fracture and the dislocation of the carpometacarpal joint. Under direct vision, the fracture and dislocation were reduced,one or two Kirschner wires ( 1.0 mm ) were used to fix the metacarpal base and the hamate temporarily. A 5- or 6-hole straight titanium miniplate of the 2.0 mm fixation system ( Stryker, USA ) was used, which was placed on the dorsal side of the hamate and the metacarpal,and fixed with screws. If the hamate body coronal plane fracture was combined with dislocation of the fourth and the fifth carpometacarpal joints, two straight titanium miniplates were placed in a V shape ( Fig.2 ).Mini C-arm imaging system was used to check the fracture reduction and the position of internal fixation.If the results were satisfactory, the wound was washed;the periosteum and joint capsule were closed with 5 - 0 PDSII suture and the skin was closed with 5 - 0 silk suture. One subcutaneous drainage strip was placed, the incision was dressed, and plaster ( U-shape, ulnar side of the wrist ) was applied for 1 - 3 weeks.
Post-operation care
After removal of the drainage strip two days after surgery, the dressing was changed regularly. Depending on the type of the fracture and the surgeon's judgment on the strength of fixation, the plaster was removed 1 -3 weeks post-surgery. Flexion and extension exercises were started. A radiograph was obtained three months after the surgery confirming fracture union after which the plates could be removed.
Follow-up and efficacy assessment
Follow-up time and method
Follow-up visit was scheduled at 2, 4, 6, and 8 weeks as well as 3, 6, 9, and 12 months after the surgery; patients were then followed up every 6 months.For each scheduled follow-up visit, radiographs and clinical examinations were done.
Clinical assessments included grip strength of the injuried and contralateral hands, and the total active motion ( TAM ) of the ring and little fingers. Posterioranterior, lateral, and 30° pronated oblique radiographs were obtained to assess fracture healing and malunion.
Outcomes measurement
Functional improvement was evaluated using the Disabilities of the Arm, Shoulder and Hand ( DASH )Score and the Mayo Wrist Score ( MWS ). Pain was assessed using the Visual Analogue Scale ( VAS ).
Statistical analysis
SPSS17.0 statistical software ( SPSS Inc.,USA ) was used for statistical analysis. Injuried and contralateral hand grip, TAM of the ring finger and the little finger follows normal distribution. Comparison between groups was applied using paired t-test. The ɑ level ( i.e., significance level ) was 0.05 ( two-sided ).
Results
General information
All 24 patients were followed up for 13 to 44 months ( 18.5 ± 8.3 ) months. All hamate fractures united within 6 to 10 ( 6.9 ± 1.1 ) weeks. Plates were removed 3 to 6 months after the operation in 22 of the 24 patients.
Healing of fractures and dislocations
Fracture healing was determined based on the radiographs and clinical examinations. The criteria for fracture healing was the blurring or disappearance of fracture line and no obvious tenderness at the fracture /dislocation site. Before removing the plates, CT of the wrist was done as a final assessment for fracture healing.No nonunion or malunion occurred and carpometacarpal joint subluxation was observed ( Fig.2 ).
Functional evaluation
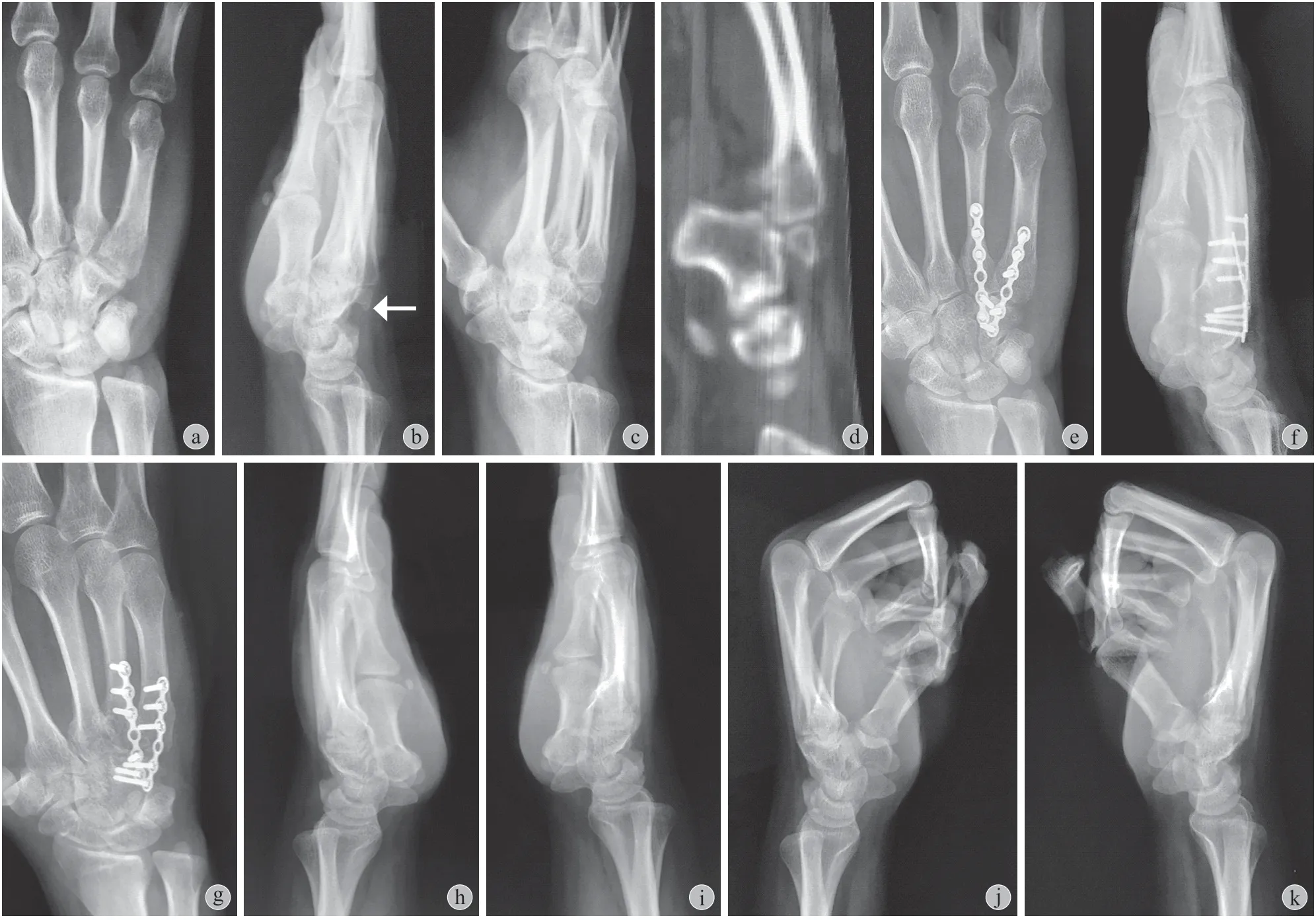
Fig.2 Images of typical case, a male patient aged 32 years who had hurt his right hand after hitting a wall with his fist a: Posteroanterior X-ray image shows the fourth and the fifth metacarpal proximal displacement and the disappearance of the space between the fourth and the fifth carpometacarpal joints; b: Lateral view shows the displacement of the fourth and the fifth metacarpal bases with the fracture fragment of hamate towards the proximal side and the dorsal side ( the arrow ), the “not parallel” sign in the shaft of the metacarpals is seen; c - d: ( c ) Oblique view and ( d ) Sagittal CT image show hamate body fracture and dislocation of the carpometacarpal joint; e: The hamate and the fourth and the fifth metacarpals were fixed with titanium miniplates through the carpometacarpal joint. Posteroanterior X-ray image shows restored carpometacarpal joint space; f - g: ( f ) Lateral view and ( g ) Oblique view shows that the “not parallel” sign of the metacarpal shaft was corrected. The hamate fracture and the dislocation of the carpometacarpal joint are reduced; h - k: Range of motion of the fourth and the fifth carpometacarpal joints at the final follow-up
At final follow-up, the DASH score was 0 - 10.8 with a mean of 1.7 ± 3.1; the VAS score was 0 - 3 with a mean of 0.5 ± 0.8; the MWS ( Mayo Wrist score ) was 65 - 100 with a mean of 94.2 ± 10.0; hand grip strength of the affected hand was ( 42.0 ± 4.4 ) kg, and ( 41.1 ±2.8 ) kg for the contralateral hand; TAM of the ring finger and little finger were ( 281 ± 3 ) ° and ( 271 ± 6 ) ° for the affected side, while ( 283 ± 3 ) ° and ( 272 ± 4 ) °for the contralateral side; No statistically significant differences were found in hand grip strength and TAM( Tab.2 ).
Surgery-related complications
There were no incidents of postoperative infection,delayed union, or malunion. One patient had transient postoperative ulnar nerve irritation, which recovered without treatment in three weeks. In addition, one patient had a loose screw at the distal end of the miniplate 4 months after surgery. In another patient the titanium plate broke at the carpometacarpal joint.Fractures healed fully in the two patients .
Discussion
1. Types of coronal plane fracture of the hamate body and the mechanism of injury
Typing of hamate fractures is relatively complicated. Due to limitations of early imaging technology, Milch[1]believed that most fracture lines of hamate fractures were oblique from the radial side to the dorsal side and were very close to the hamate hook. He also emphasized that such fractures had no obvious displacement and were suitable for conservative treatment. In 2005, Hirano et al[5]divided hamate fracture into Type 1 hamate hook fractures and Type 2 hamate body fractures on the basis of the Milch typing.Wherein the hamate body fractures were divided into two subtypes: ( 2a ) fractures of the coronal plane, and( 2b ) cross-sectional plane. Type 2a fractures were further divided into dorsal oblique fractures and isolated fractures of the coronal plane.
Tab.2 Basic information of patients
Coronal plane fractures are the most common hamate fracture. Cain et al[7]divided hamate body fracture and dislocation of carpometacarpal joint into three types. Type IA is a simple carpometacarpal joint dislocation; Type IB is a carpometacarpal joint dislocation with avulsion fracture of the distal dorsal edge of the hamate; Type II is a wider range dorsal comminuted fracture of the hamate; Type III is a coronal plane fracture of the hamate body. Ebraheim et al[6]further divided coronal plane fracture of the hamate body into three types. Type A fracture has the fracture line through the coronal plane at the middle of the hamate body; Type B fracture has an oblique fracture line from the middle of distal surface of hamate body leading to the dorsal side, and involving most of the carpometacarpal joint surface; Type C fracture is an avulsion fracture of the distal dorsal edge of the hamate,which is similar to Type I and Type II of the Cain classification. Ebraheim typing of the coronal plane fracture of the hamate body is relatively thorough and has covered more fracture types. It is more helpful in developing a reasonable treatment plan. Therefore, in this group we used the Ebraheim method to type the coronal plane fractures of the hamate body.
Thomas and Birch[8]suggested that the type of hamate body fracture is determined by the position of the wrist when the injury occurred. If axial stress is transmitted from distal to proximal, as the wrist is in ulnar deviation, the result is coronal plane fracture; if the wrist is in a neutral position or radial deviation,the result is a sagittal fracture. Hamate proximal fracture is common in more serious wrist fractures and dislocations, while medial tuberosity fracture is caused by direct violence in the ulnar side of the wrist. Among studies on the mechanism of coronal plane fractures of the hamate body, Cain[7]and Ebraheim[6]suggested that since the range of motion of the fourth and the fifth carpometacarpal joints was 15° and 30°, respectively,different types of coronal plane fracture occurred when the wrist was at different angles of flexion and extension. We have carried out an anatomical study and found a 28° palmar angle at the dorsal side of the distal hamate body ( Fig.3 ). Based on this finding, we hypothesize that when the carpometacarpal joint is at the neutral position, the axial stress may cause Ebraheim Type A fractures and Cain Type III fractures; while the carpometacarpal joint is at different degrees of flexion,axial stress may cause Ebraheim Type B or Type C fractures, and Cain Type I and Type II fractures. Since the flexion of the fourth and the fifth carpometacarpal joints is associated with the formation of a fist, greater flexion angle is more likely to cause Ebraheim Type B or Type C fractures, and Cain Type I and Type II fractures.Therefore, differential strength used to form a fist may lead to different types of coronal plane fracture of the hamate body.
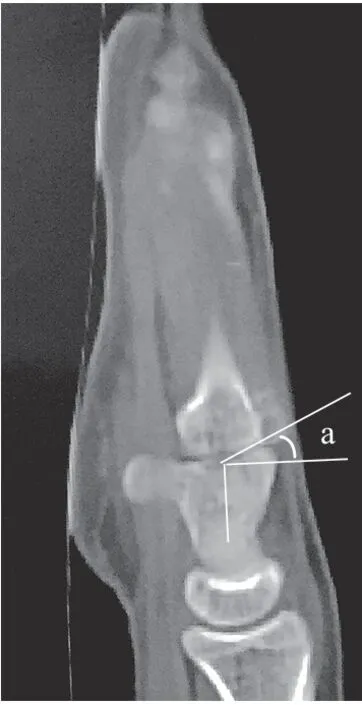
Fig.3 Sagittal computed tomography ( CT ) images of the fourth carpometacarpal joint palmar angle of the hamate
2. Diagnostic imaging characteristics of coronal plane fracture of the hamate body
Conventional wrist X-ray examination has a high rate of misdiagnosis for hamate body fracture.Ebraheim et al[6]reported a misdiagnosis rate of 45% at the first visit for hamate body fractures. For another group of patients reported by Bishop et al[9],the average diagnosis time was 10 months after injury. The results of an in vitro study using autopsy specimens by Andresen et al[10]. showed that wrist X-ray from the anteroposterior, lateral, and tangential to the carpal tunnel positions had a diagnosis rate of 39% for displaced hamate body fractures. Therefore,to diagnose hamate body fracture, in addition of taking the routine wrist X-ray from the anteroposterior and lateral positions, the pronation oblique position at 30° -45° is also very important. Hamate body fracture and dislocation of the carpometacarpal joint can be
confirmed by taking a pronated oblique image, and such images can increase the diagnosis accuracy to 72%[10].Besides, in the lateral X-ray image of the wrist, the "not parallel" sign in the shaft of the metacarpals is also an important indirect sign of coronal plane fracture of the hamate body and a direct sign of carpometacarpal joint dislocation. When the axis of the fifth, or the fourth and the fifth metacarpals and the axis of the second and the third metacarpals forms an angle, it indicates carpometacarpal joint dislocation and a possibility of complications of coronal plane fracture of the hamate body. CT examination is still the “golden standard” for the diagnosis of coronal plane fracture of the hamate body. CT tomography in different planes can accurately diagnose hamate body fracture and clearly demonstrate the type of the fracture[11]( Fig.2 ).
3. Clinical efficacy and operation techniques of using titanium miniplates through the carpometacarpal joints for the treatment of coronal plane fracture of the hamate body
Coronal plane fracture of the hamate body affects the smooth articular surface and damages the stability of the carpometacarpal joint. The titanium miniplate can buttress and fix the fracture to achieve reduction and the screws provide enhanced stability. Plate fixation provides enough rigidity and stability to start early range of motion exercises.
The technical points of this operative procedure include: ( 1 ) The dorsal branch of the ulnar nerve needs to be protected. ( 2 ) The dorsal side of the hamate body needs to be exposed fully. ( 3 ) Anatomic reduction of the fracture and the dislocation needs to be carried out accurately. For the fracture reduction under direct vision, the surface of the carpometacarpal joint should be restored as anatomically as possible. ( 4 ) Strong internal fixation of the fracture and dislocation is required. ( 5 ) The ulnar nerve along with its deep and superficial branches need to be protected. The ulnar nerve and its deep and superficial branches are located in the Guyon canal that is on the palm radial side of the hamate body. Since the screws used to fix the hamate need to be inserted in a position that is inclined to the ulnar side, attention should be paid when drilling the holes and fixing the screws to avoid injury to the ulnar nerve. In the fixation of the fourth carpometacarpal joint, the screw tends to the ulnar side and its length is usually 15-16mm. Among this series of cases, one patient had transient postoperative ulnar nerve injury symptoms that disappeared later without treatment. ( 6 )The internal fixation needs to be removed in a timely manner. Since the range of motion of the fourth and fifth carpometacarpal joint is 15° and 30° respectively,the titanium miniplate at the carpometacarpal joint level will have to bear repetitive stress that may lead to metal fatigue even miniplate break. Therefore, when the fracture and the dislocation have healed, the internal fixation should be removed 3 to 6 months after the operation. Among this series of cases, two patients had loosened and broken internal fixation, respectively.