SOFA、SIRS、qSOFA评分和乳酸对儿童脓毒症预后的判断价值
2020-10-09吴云朵林小飞顾小海
吴云朵 林小飞 顾小海


[摘要] 目的 評价乳酸及序贯器官衰竭评分(SOFA)、全身炎症反应综合征评分(SIRS)、快速序贯器官衰竭评分(qSOFA)评分对儿童脓毒症患者预后的评估价值。 方法 回顾性分析2016年1月—2018年12月江苏省淮安市妇幼保健院儿科普通病房及重症病房且符合Sepsis-3诊断标准的259例患儿的临床资料,根据预后将其分为存活组(241例)和死亡组(18例)。受试者工作特征曲线(ROC)评估两组乳酸、24 h内SOFA、SIRS及qSOFA对患者预后的预测价值。 结果 死亡组乳酸水平、SOFA、SIRS、qSOFA评分高于存活组,差异均有高度统计学意义(均P < 0.01)。SOFA评分诊断脓毒症患儿死亡的临界值为7.5分,敏感度为68.8%,特异性为80.0%;qSOFA评分诊断脓毒症患儿死亡的临界值为1.5分,敏感度为68.8%,特异性为80.0%;乳酸诊断脓毒症患儿死亡的临界值为1.75 mmol/L,敏感度为93.8%,特异性为40.0%。 结论 与SIRS评分比较,SOFA、qSOFA评分对于儿童脓毒症预后的判断更有价值,而传统指标乳酸有很好的敏感性,是判断脓毒症患儿预后的可靠指标,但特异性低。
[关键词] 儿童脓毒症;序贯器官衰竭评分;快速序贯器官衰竭评分;全身炎症反应综合征评分;乳酸
[中图分类号] R720.597 [文献标识码] A [文章编号] 1673-7210(2020)08(b)-0074-04
[Abstract] Objective To investigate the prognostic value of sequential organ failure assessment (SOFA), systemic inflammatory response syndrome (SIRS) score, quick sequential organ failure assessment (qSOFA) score and lactate level in pediatric sepsis. Methods A total of 259 pediatric patients with Sepsis-3 diagnosis in general and intensive care units of Huai′an Maternal and Child Health Hospital of Jiangsu Province from January 2016 to December 2018 were retrospectively analyzed. They were divided into survival group (241 cases) and death group (18 cases) according to the prognosis. Receiver operating characteristic curve (ROC) was used to assessed the predictive value of lactate level, SOFA within 24 h and SIRS and qSOFA for prognosis of patients. Results Lactate level, SIRS, SOFA and qSOFA scores in death group were higher than those in survival group, and the differences were all highly statistically significant (all P < 0.01). The cut-off value for the death of sepsis by SOFA score was 7.5 points, the sensitivity was 68.8%, and the specificity was 80.0% respectively. The cut-off value for the death of sepsis by qSOFA score was 1.5 points, the sensitivity was 68.8%, and the specificity was 80.0%. The cut-off value for the death of sepsis by lactate value was 1.75 mmol/L, the sensitivity was 93.8%, and the specificity was 40.0%. Conclusion Compared with SIRS score, SOFA and qSOFA scores have better prognostic accuracy in predicting the prognosis of children with sepsis. Although lactate level has good sensitivity and is a reliable indicator for the prognosis of children with sepsis, but its specificity is low.
[Key words] Pediatric sepsis; Sequential organ failure assessment; Quick sequential organ failure assessment; Systemic inflammatory response syndrome score; Lactate
儿童脓毒症是重症患儿主要死亡原因之一,而脓毒症的定义也在经常修订,最近的Sepsis-3定义强调脓毒症区别于单纯性感染是由于宿主对感染的反应失调而产生威胁生命器官功能障碍的结果[1]。Sepsis-3的验证队列基于成人人群,目前认识到应为“儿童人群制订类似的更新定义关系”[2]。但是,目前的小儿脓毒症定义基本上仍基于败血症、代表研究、基准测试、编码的主要障碍和质量监控[2-3]。Sepsis-3中序贯器官衰竭评分(SOFA)作为脓毒症的诊断标准。自从Sepsis-3共识发表以来,与以前的脓毒症标准比较,重症监护室(ICU)中进行的几项成人研究报道SOFA和快速序贯器官衰竭评分(qSOFA)评估预后的准确性更好[4-7]。因该评分在儿童与成人中反映器官功能的部分变量的正常范围不同,故SOFA和qSOFA评分在儿童中应用受限,而本研究中的评分根据年龄进行调整后来判断对小儿脓毒症预后的预测价值。
1 资料与方法
1.1 一般资料
回顾性分析2016年1月—2018年12月江苏省淮安市妇幼保健院儿科普通病房、儿科重症病房(PICU)259例脓毒症患儿的病例资料。纳入标准:①符合Sepsis-3诊断标准(根据年龄进行相应的调整)[1];②年龄28 d~14岁。排除标准:①住院时间≤24 h者;②既往有严重的肝肾功能不全者。根据预后将患儿分为存活组(241例)和死亡组(18例)。
1.2 疾病诊断标准
根据SOFA评分标准[8],将心血管指标由成人平均动脉压(MAP)<70 mmHg(1 mmHg=0.133 kPa)更改为收缩压小于同年龄的第5百分位值。qSOFA评分标准[9]:神志改变、收缩压≤100 mmHg、呼吸频率≥22次/min,其中符合1项记1分,呼吸频率和收缩压通过使用特定年龄段来定义。全身炎症反应综合征评分(SIRS)[10]标准:体温>38℃或<36℃、心率>90次/min、呼吸>20次/min或动脉血二氧化碳分压(PaCO2)<4.3 kPa、白细胞(WBC)数>12.0×109/L或<4.0×109/L或幼稚细胞>10%,符合1项记1分。
1.3 方法
收集两组性别、年龄、体温、C反应蛋白(CRP)水平、血培养结果、WBC水平、感染部位等一般资料;收集24 h内乳酸水平、SOFA、SIRS、qSOFA评分。乳酸检测方法:采集患者桡动脉血0.5 mL,肝素抗凝,全自动血气分析仪(ABL90雷度血气分析仪,雷度米特医疗设备上海有限公司)定量检测。
1.4 统计学方法
采用SPSS 17.0统计学软件进行数据分析,符合正态分布计量资料用均数±标准差(x±s)表示,两组间比较采用t检验;不符合正态分布用中位数(M)四分位数间距(Q)表示,两组间比较采用秩和检验。计数资料用率表示,组间比较采用χ2检验;受试者工作特征曲线(ROC)预测乳酸水平及SOFA、SIRS、qSOFA评分对脓毒症患儿死亡的诊断效能。以P < 0.05为差异有统计学意义。
2 结果
2.1 两组一般资料比较
两组性别、血培养(+)、感染部位比较,差异无统计学意义(P > 0.05);死亡组年龄低于存活组,死亡组体温、CRP水平、WBC水平高于存活组,差异均有统计学意义(均P < 0.05),见表1。127例(49.0%)患者需要经历儿童重症监护室(PICU)住院时间≥3 d。
2.2 两组乳酸水平及SOFA、SIRS、qSOFA评分比较
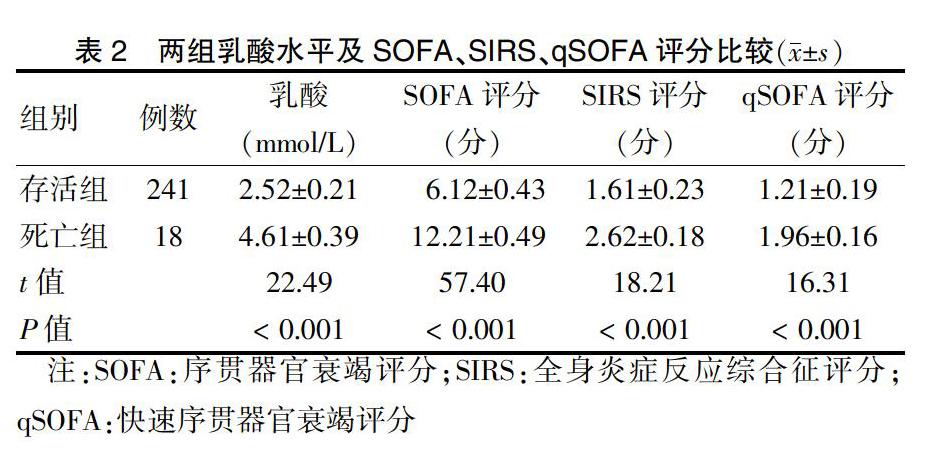
死亡组乳酸水平及SOFA、SIRS、qSOFA评分高于存活组,差异均有高度统计学意义(均P < 0.01)。见表2。
2.3 乳酸及SOFA、SIRS、qSOFA评分对脓毒症患儿死亡的诊断效能
SOFA评分诊断脓毒症患儿死亡的临界值为7.5分,敏感度为68.8%,特异性为80.0%;qSOFA评分诊断脓毒症患儿死亡的临界值为1.5分,敏感度为68.8%,特异性为80.0%;乳酸诊断脓毒症患儿死亡的临界值为1.75 mmol/L,敏感度为93.8%,特异性为40.0%。见图3、表3。
3 讨论
Sepsis-3定义在儿童中的应用未得到普遍接受,且存在争议[11-12],其定义的临床数据主要来源于美国ICU住院的成年患者,SOFA评分已被提议为成人筛查工具,用于判断器官功能障碍,而为了进一步快速简便的应用于临床,又提出了qSOFA评分的概念,该评分在急诊室中能够很好的应用。本研究主要分析普通病房或PICU 24 h内评分,可能因无法记录疾病的严重程度峰值,而导致评分降低[13]。尽管不显著,但SOFA、qSOFA评分在判断ICU转移和死亡率方面高于SIRS评分。儿童与成人SOFA反映器官功能部分变量的正常范围不一样,其主要区别在循环系统中低血压及反映肾功能的肌酐、尿量的标准,儿童应该根据年龄作出相应调整,将心血管指标由成人的MAP<70 mmHg更改为收缩压小于同年龄的第5百分位值[14-15]。本研究因样本量少未对肾脏的肌酐变量进行调整,其他均与原始SOFA评分标准相同。两项研究均说明SOFA评分在儿童中应用同样有效,但SOFA评分中各项生理值是否需要根据年龄进行调整,如何调整,尚有待进一步探讨且需通过进行更多的临床研究来验证其有效性,本研究结果显示其相对于传统的SIRS评分能更好评估脓毒症的预后。
传统指标乳酸,虽然特异性不足,但仍是小儿脓毒症诊治過程中非常可靠的指标之一。研究显示[16-17],乳酸是儿童脓毒症严重程度的最佳预测指标之一,此外,乳酸被建议用于早期的风险分层[18-19]。Sepsis-3标准认为脓毒症休克是脓毒症的一个特定阶段,这其中乳酸水平是个重要指标,李玖军等[20]研究结果显示,儿童脓毒症休克定义为在脓毒症基础上,乳酸水平 >2 mmol/L。本研究因相对较小的样本量和少量不良事件可能阻碍了补液无法纠正的低血压及血乳酸水平的这一分析,因此,较大样本量的研究将会进一步进行。既往针对儿童的研究报道指出,PICU中乳酸水平的升高与死亡风险之间存在密切而独立的联系[21]。乳酸是无氧酵解情况下糖的代谢产物,可反映组织缺血缺氧的情况。脓毒症时乳酸异常升高,升高程度与病情严重程度和病死率呈正相关。Ceneviva等[22]的一项针对儿童脓毒症的研究提示,在急诊就诊的脓毒症患儿中,乳酸水平高于4 mmol/L与死亡率相关,但敏感性较低,本研究结果显示,死亡组乳酸水平明显高于存活组(P < 0.05),曲线下面积为0.9,与以往的研究[22]一致。而Sepsis-3也将乳酸作为诊断脓毒症休克的诊断指标之一,虽然组织缺氧、肌肉活动增加、酒精中毒以及严重肝肾功能不全等可导致高乳酸血症,但是乳酸水平的升高依然是脓毒症很强的评估预后指标。故Sepsis-3标准可以应用在儿童中,但是如何根据儿童特点进行调整,尚需大规模的临床观察评估。本研究的局限性有:①只列举乳酸一项传统指标;②本研究为单中心、回顾性研究,样本量少,可能还需要结合其他传统指标、多中心、前瞻性随机对照试验研究等综合判断。总之,围绕脓毒症的定义及诊断标准的争论仍会继续[23]。
[參考文献]
[1] Singer M,Deutschman CS,Seymour CW,et al. The third international consensus definitions for sepsis and septic shock(Sepsis-3)[J]. JAMA,2016,315(8):801-810.
[2] Schlapbach LJ. Time for Sepsis-3 in children? [J]. Pediatr Crit Care Med,2017,18(8):805-806.
[3] Schlapbach LJ,Kisson N. Pediatric sepsis definitions-an urgent need for change [J]. JAMA Pediatr,2018,20181(172):4.
[4] Seymour CW,Liu VX,Iwashyna TJ,et al. Assessment of clinical criteria for sepsis:for the Third International Consensus Definitions for Sepsis and Septic Shock(Sepsis-3)[J]. JAMA,2016,315(8):762-774.
[5] Raith EP,Udy AA,Bailey M,et al. Prognostic accuracy of the SOFA score,SIRS criteria,and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit [J]. JAMA,2017,317(3):290-300.
[6] Wang JY,Chen YX,Guo SB,et al. Predictive performance of quick Sepsis-related Organ Failure Assessment for mortality and ICU admission in patients with infection at the ED [J]. Am J Emerg Med,2016,34(9):1788-1793.
[7] Freund Y,Lemachatti N,Krastinova E,et al. Prognostic accuracy of Sepsis-3 criteria for in-hospital mortality among patients with suspected infection presenting to the emergency department [J]. JAMA,2017,317(3):301-308.
[8] Vincent JL,Moreno R,Takala J,et al. The SOFA(Sepsis-related Organ Failure Assessment)score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine [J]. Intensive Care Med,1996,22(7):707-710.
[9] Dorsett M,Kroll M,Smith CS,et al. qSOFA Has Poor Sensitivity for Prehospital Identification of Severe Sepsis and Septic Shock [J]. Prehosp Emerg Care. 2017,21(4):489-497.
[10] Arvaniti V, D′Amico G, Fede G, et al. Infections in patients with cirrhosis increase mortality four-fold and should be used in determining prognosis [J]. Gastroenterology,2010,139(4):1246-1256.e12565.
[11] Angus DC,Seymour CW,Coopersmith CM,et al. A Framework for the Development and Interpretation of Different Sepsis Definitions and Clinical Criteria [J]. Crit Care Med,2016,44(3):e113-e121.
[12] Simpson SQ. New Sepsis Criteria:A Change We Should Not Make [J]. Chest,2016,149(5):1117-1118.
[13] Matics TJ,Sanchez-Pinto LN. Adaptation and Validation of a Pediatric Sequential Organ Failure Assessment Score and Evaluation of the Sepsis-3 Definitions in Critically Ill Children [J]. JAMA Pediatr,2017,171(10):e172352.
[14] Ha EJ,Kim S,Jin HS,et al. Early changes in SOFA score as a prognostic factor in pediatric oncology patients requiring mechanical ventilatory support [J]. J Pediatr Hematol Oncol,2010,32(8):e308-e313.
[15] Jhang WK,Kim YA,Ha EJ,et al. Extrarenal sequential organ failure assessment score as an outcome predictor of critically ill children on continuous renal replacement therapy [J]. Pediatr Nephrol,2014,29(6):1089-1095.
[16] Scott HF,Brou L,Deakyne SJ,et al. Association between early lactate levels and 30-day mortality in clinically suspected sepsis in children. [J]. JAMA Pediatr,2017, 171(3):249-255.
[17] Schlapbach LJ,MacLaren G,Straney L. Venous vs arterial lactate and 30-day mortality in pediatric sepsis [J]. JAMA Pediatr,2017,171(8):813.
[18] Tavaré A,O′Flynn N. Recognition,diagnosis,and early management of sepsis:NICE guideline [J]. Br J Gen Pract,2017,67(657):185-186.
[19] Shetty A,MacDonald SP,Williams JM,et al. Lactate ≥2 mmol/L plus qSOFA improves utility over qSOFA alone in emergency department patients presenting with suspected sepsis [J]. Emerg Med Australas,2017,29(6):626-634.
[20] 李玖軍,邹凝,潘佳丽.儿童脓毒症诊断标准及鉴别诊断[J].中国中西医结合儿科学,2015,7(4):289-292.
[21] Schlapbach LJ,MacLaren G,Festa M,et al. Prediction of pediatric sepsis mortality within 1 h of intensive care admission [J]. Intensive Care Med,2017,43(8):1085-1096.
[22] Ceneviva G,Paschall JA,Maffei F,et al. Hemodynamic support in fluid-refractory pediatric septic shock [J]. Pediatrics,1998,102(2):e19.
[23] Barea-Mendoza JA,Cortés-Puch I,Chico-Fernández M. Conflicts of interest in the new consensus based definition of sepsis and septic shock(sepsis-3)[J]. Med Intensiva,2017,41(1):60-61.
(收稿日期:2020-03-17)
