Cutaneous toxicities of targeted therapies in the treatment of hepatocellular carcinoma
2020-07-21TarikSilkJenniferWu
Tarik Silk, Jennifer Wu
1Internal Medicine, New York University School of Medicine, New York, NY 10016, USA.
2Hematology and Medical Oncology, Perlmutter Cancer Center, New York University School of Medicine, New York, NY 10016,USA.
Abstract Liver cancer accounts for 4.7% of all newly diagnosed cancers and 8.2% of cancer deaths annu-ally.Hepatocellular carcinoma (HCC) accounts for the majority of primary liver cancers. There are 2 curative strategies in HCC: resection and transplant. Unfortunately, 50% of patients who undergo resection will relapse in 2 years and many patients on transplant lists become ineligible for transplant due to disease progression. The majority of patients still require systemic therapies. Tyrosine kinase inhibitors have successfully extended the overall survival in patients with hepa-tocellular carcinoma. However, these treatments have been noted to cause severe side effects in-cluding liver toxicity, hypertension, gastrointestinal toxicity and cutaneous adverse effects. This article will focus on the adverse skin reactions seen during the treatment of hepatocellular carci-noma by various tyrosine kinase inhibitors. The focus will be symptomatology, management, and whether the development of cutaneous toxicities can be prognostic.
Keywords: Hepatocellular cancer, tyrosine kinase inhibitors, cutaneous toxicity, hand foot reaction syndrome
BACKGROUND
Liver cancer accounts for 4.7% of all newly diagnosed cancers and 8.2% of cancer deaths annually[1].Hepatocellular carcinoma (HCC) accounts for the majority of primary liver cancers[2]. As much as 50%of patients with HCC are diagnosed at early stages when curative treatments are possible[3]. There are 2 curative strategies in HCC: resection and transplant. Unfortunately, 50% of patients who undergo resection will relapse in 2 years and many patients on transplant lists become ineligible for transplant due to disease progression. The majority of patients still require systemic therapies. In 2008, the FDA approved the tyrosine kinase inhibitor (TKI) Sorafenib as the first systemic therapy for patients with inoperable hepatocellular cancer. Its approval was based on the overall survival (OS) benefit of Sorafenib compared to placebo in the first-line setting 10.7 monthsvs. 7.9 months, respectively[4]. Since Sorafenib’s approval,several other tyrosine kinase inhibitors have been added to the armamentarium against late-stage HCC.These new TKIs include Lenvatinib, Cabozantinib, and Regorafenib[5-7]. Cutaneous toxicities are frequently observed during targeted treatment of cancer, as many targeted therapies, including TKIs, inhibit growth factors found in the skin[8].
In this review, we will focus on the adverse skin reactions seen during the treatment of hepatocellular carcinoma by various tyrosine kinase inhibitors. The focus will be on symptomatology and management of these reactions. Additionally, this review will discuss whether the development of cutaneous toxicities can be prognostic.
Symptomatology and treatment for particular cutaneous toxicities are discussed with each major toxicity.The cutaneous toxicities of particular TKIs will be discussed within each TKI’s section along with the toxicity’s onset and suggested dose modifications of the TKI.
HAND FOOT REACTION SYNDROME
Risk factors and incidence
The incidence of hand foot reaction syndrome (HFRS) in the treatment of HCC varies depending on the TKI[9]. Predisposing factors to HFRS seen in TKI treatments include female gender, ECOG status 2 or lower, two or more organs involved, baseline lung/liver metastases, a baseline white blood count above 5.5 × 109cells/L, and the duration of the TKI therapy[10]. Frequency is also higher in Asian populations[11,12].Whereas incidences of HFRS are varied, symptomatology of HFRS is shared between TKIs.
Symptoms
Patients affected by HFRS experience a prodromal tingling sensation on their palms or soles which progresses to burning pain. Hand and foot erythema and edema develops with tense blistering and peeling with lesions evolving into areas of callus-like hyperkeratosis with surrounding erythema[13-16].
Lesions tend to develop over pressure-bearing surfaces, which may be related to the pathophysiology of their development.
Pathophysiology
Although competing hypotheses exist[9,17,18], the TKI dual inhibition of different receptors, such as VEGF and PDGFR, may be required to trigger dermatological symptoms. Damage occurs when TKIs block signaling pathways resulting in the alteration of repair mechanisms or distortion to microvascular structure in areas where there is frequent trauma or friction like the palms and soles[12,14,18].
Toxicity grading and treatment
Management of HFRS is based on expert knowledge from oncologists and dermatologists. Before TKI treatment begins, proper consultation with podiatry and dermatology should be made. A full-body skin examination with special attention paid to the hands and feet should be performed. Evidence of abnormal weight bearing can be corrected with mechanical support. Areas of baseline hyperkeratotic skin can be removed with manicures and pedicures[19,20]. During treatment, twice daily prophylactic application of a 20% urea-based cream has also been suggested by some experts to prevent HFRS[20,21]. When treatment is started patients should be advised to avoid tight footwear or gloves. Patients should protect their feet with insole cushions, shock-absorbing soles, and padded socks and wear gloves to protect their hands.Emollients can be used liberally.
At night, patients should continue to wear cotton gloves and socks to retain moisture. They should also avoid extreme temperatures and wash with tepid water[14,15,18,20,22].
Further recommendations are based upon the grade of HFRS severity. The toxicity grading of HFRS is characterized according to the National Cancer Institute. Grade 1 toxicity is characterized by minimal skin changes or dermatitis (i.e., edema, redness, or hyperkeratosis) but without pain. Grade 2 toxicity develops with skin changes (i.e., peeling, blisters, bleeding, fissures, edema, or hyperkeratosis) with pain and limits daily activities. Grade 3 toxicity is marked by severe skin changes (i.e., peeling, blisters, bleeding, fissures,edema, or hyperkeratosis) with pain that limits self-care[23].
Grade 1 toxicities can be managed with topical therapy usually with the continuation of the TKI dose[19,20,22].Topical treatments are similar to those used for prophylactic care. 20%-40% urea creams should be used on areas of hyperkeratosis twice a day[15,18,20,22].
Grade 2 toxicities are managed with topical therapy and dose reductions if necessary. Areas of hyperkeratosis should be treated with urea base keratolytic[16]. 0.05% Clobetasol ointment should be applied to erythematous areas twice daily[15,20,22]. Topical 2% lidocaine cream can be used for analgesia[20,22].
For Grade 3 toxicities in addition to the above treatments, dose interruption and reduction is required.Other strategies include the use of pyridoxine with doses of 50-150 mg/day[20,22,24].
Of note, in one uncontrolled study of 12 patients who developed HFRS when taking Sorafenib, the majority of patients that were treated twice daily with 40% urea cream in combination with tazarotene 0.1% cream or fluorouracil 5% cream saw a ≥ 2-grade improvement in symptoms[25][Figure 1].
RASH
Symptoms
Rashes observed with TKI treatment vary and can develop as a macule, papule, maculopapular,erythematous, and/or pruritic. Rashes often develop on the trunk and extremities or scrotum[15,26-28]. Facial and scalp erythema similar to seborrheic dermatitis has been noted with Sorafenib.
Treatment
The treatment of rashes seen during TKI therapy is once again based upon the toxicity grade. Grade 1 toxicity is described as macules/papules covering < 10% body surface area (BSA) with or without symptoms(e.g., pruritus, burning, tightness). Grade 2 toxicity is characterized by macules/papules covering 10%-30%BSA with or without symptoms (e.g., pruritus, burning, tightness); limiting instrumental activities of daily living (ADL), or a rash covering > 30% BSA with or without mild symptoms. Grade 3 toxicity is defined by macules/papules covering > 30% BSA with moderate or severe symptoms; limiting self-care ADL[23].
In general, patients with rashes should be advised to use perfume-free soaps, apply moisturizers, and wear loose comfortable clothing[22,29]. Topical corticosteroids and antihistamines may also be useful with mild rashes[22,30]. Dose reductions and interruptions of the TKI should also occur based on prescribing information for severe rashes. With proper management, most rashes have been noted to resolve in less than 6 weeks[27]. Additionally, some rashes may resolve spontaneously without symptomatic treatment as can be seen in patients with facial and scalp erythema[26,27][Figure 2].

Figure 1. Clinical spectrum of HFRS of grade 1 (A,D) grade 2 (B,E) and grade 3(C,F). Used with permission from Lipworth et al.[13],Copyright © 2009 Karger Publishers, Basel, Switzerland. HFRS: hand foot reaction syndrome

Figure 2. Example of rash on the trunk with TKI treatment. Used with permission under the Creative Commons Attribution License. (http://creativecommons.org/licenses/by/2.0)[31]. TKI: tyrosine kinase inhibitor

Figure 3. Subungual splinter hemorrhages in a patient on Sorafenib. Reprinted from Ishak et al.[33]
SCROTAL ECZEMA
Symptoms
Scrotal eczema appears as erythematous macules[32].
Treatment
Scrotal lesions seen with TKIs have been treated with athletic supporters to reduce friction and barrier ointments/pastes such as zinc oxide and menthol. Topical steroids can also be used[15,32].
SUBUNGUAL SPLINTER HEMORRHAGES
Symptoms
Subungual splinter hemorrhages appear as multiple subcentimeter longitudinal brown to black lines beneath the distal nail plate. They are asymptomatic[26].
Treatment
Subungual splinter hemorrhages do not require treatment as they tend to spontaneously resolve[15,26,27][Figure 3].
ALOPECIA
Symptoms
Alopecia may occur with thinning or patchy hair loss. Complete alopecia has been seen in patients with renal cell carcinoma treated with Sorafenib. Alopecia can involve loss of hair on the body as well as the scalp[26].
Treatment
Alopecia produced by TKIs although distressing to patients has not been shown to require dose modification. Alopecia has spontaneously resolved in some patients despite continued treatment[26].

Figure 4. Example of stomatitis seen with TKI treatment. Used with permission under Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0)[39]. TKI: tyrosine kinase inhibitor
STOMATITIS
Symptoms
Stomatitis or oral mucositis may manifest as dry mouth, oral sensitivity, dysphagia, or taste changes[29,34].Ulcers may also occur[22].
Toxicity grading and treatment
Like HFRS, prevention may be the best strategy. Prophylactic measures include good oral hygiene by brushing teeth with a soft-headed toothbrush and fluoride toothpaste after meals and before sleep. Flossing once a day and using alcohol-free mouth rinses four times daily is encouraged. Dentures should be cleaned daily. Patients need to avoid spicy and sticky foods, as well as alcohol and tobacco[29,34,35].
Further recommendations are based upon the grade of stomatitis severity. Adverse events of stomatitis are characterized according to the National Cancer Institute. Grade 1 toxicities are described as asymptomatic or mild symptoms. Grade 2 toxicities are characterized by moderate pain or ulcers that do not interfere with oral intake. Grade 3 toxicities involve severe pain interfering with oral intake[23].
When adverse events do occur, grade 1/2 events can be managed with magic mouthwash or swish spit rinses with 0.9% sodium bicarbonate or 0.9% saline- containing mouthwash[36,37]. Magic mouthwashes typically contain a mixture of diphenhydramine, viscous lidocaine, nystatin, dyclonine magnesium hydroxide, or aluminum hydroxide, and occasionally corticosteroids. However, bland saline rinses may be just as effective as magic mouthwashes[36]. Topical anesthetics, mucosal coating agents, and/or benzydamine HCl may be administered as needed for pain relief, but patients should be advised to avoid eating or performing oral hygiene when their mouth is numb. Grade 3 events require dose interruption and reduction[22,34,38][Figure 4].

Figure 5. Example of erythema multiforme. Image author James Heilman, MD. Obtained under Creative Commons license Attribution-Share Alike 3.0 Unported. https://creativecommons.org/licenses/by-sa/3.0/deed.en
ERYTHEMA MULTIFORME
Symptoms
Erythema Multiforme is typically a self-limited acute skin reaction that has been reported to occur within the first week of TKI treatment for HCC[40-42]. Lesions described in the case reports were targetoid erythematous lesions spread over the trunk and extremities. In one report, a patient developed painful oral lesions and, in general, oral lesions are found in up to 60% of people with erythema multiforme[42,43].Erythema multiforme is diagnosed clinically based on the patient’s history and physical examination. It usually has fixed lesions for a minimum of 7 days.
Treatment
Treatment involves medication discontinuation. Additionally for mild disease oral antihistamines with or without topical steroids are prescribed[42,44]. If painful mucosal erosions are present, they can be treated with high potency topical corticosteroid gels and magic mouthwashes. If oral lesions prevent sufficient oral intake, studies have recommended systemic glucocorticoids, including prednisone 40-60 mg daily with dosage taper over 2-4 weeks[42,44][Figure 5].
STEVENS-JOHNSON SYNDROME AND TOXIC EPIDERMAL NECROLYSIS
Symptoms
Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN) have both been reported to occur in patients with HCC treated with TKIs[40,45]. These are both life-threatening reactions that usually begin 4-28 days after taking the offending medication. SJS and TEN are a spectrum of epidermal necrolysis with SJS occurring with less than 10% skin detachment and TEN when there is greater than 30%. Anything in between is called SJS-TEN[46,47]. Flu-like symptoms usually precede cutaneous manifestations. Initial lesions are usually erythematous, irregularly shaped, and can first appear on the face, upper trunk, and proximal extremities. Necrotic lesions coalesce and slough off either spontaneously or with applied lateral pressure (as seen in Nikolsky’s sign) revealing the red underlying dermis.

Figure 6. Example of Toxic Epidermal Necrolysis. Image author Afro Brazilian. Obtained with permission under Creative Commons license Attribution-Share Alike 3.0 Unported. https://creativecommons.org/licenses/by-sa/3.0/deed.en
Treatment
Treatment involves a multidiscipline approach. The TKI must be stopped and the patient should be transferred to the intensive care unit or burn unit. Supportive care measures involve thermoregulation with an ambient temperature of 28-32 degrees Celsius. If a respiratory compromise is suspected, these patients can be intubated. Administration of fluid replacement is advised at 0.7 mL/kg/(% affected area) along with a 5% albumin solution at 1 mL/kg/(% affected area)[46,47]. Systemic corticosteroids are the most common treatment for SJS/TEN, a suggested protocol is intravenous dexamethasone at 1.5 mg/kg pulse therapy(given for 30-60 min) for 3 consecutive days[46,48]. Cyclosporine and Etanercept have also shown benefit[49,50].Daily skin treatment is recommended with a daily antiseptic bath containing a solution of chlorhexidine 1/5000 or with a chlorhexidine spray. Skin debridement should be avoided because necrolytic sheets act as a natural biological dressing. Nonadhesive dressings are used to cover pressure points[49,50][Figure 6].
TYROSINE KINASE INHIBITORS USED FOR HCC TREATMENT
Tyrosine kinase inhibitors, including Sorafenib, Lenvatinib, Cabozantinib, and Regorafenib are small molecules that attack cancers by inhibiting the activity of receptor tyrosine kinases which are responsible for tumor-promoting pathways such as proliferation and angiogenesis[51].
SORAFENIB
Sorafenib cutaneous toxicities and toxicity incidence
Sorafenib was FDA approved for the treatment of HCC in 2008 after a phase three randomized placebocontrolled trial showed that it extended patient survival. Safety results of that study reported that 80% of patients taking Sorafenib experienced an adverse event with the majority of patients experiencing grade 1 or 2 dermatological events. These events and the percentage of patients reporting them included: alopecia(14%, grade 3: 0%), dry skin (8%, grade 3: 0%), HFRS (24%, grade 3: 8%), pruritus (8%, grade 3: 0%), rash and/or desquamation (16%, grade 3: 1%)[4]. Similar adverse events were also seen in another study that investigated Sorafenib therapy in an Asian-Pacific population[11]. Other cutaneous toxicities reported with Sorafenib include sublingual splinter hemorrhage which occurs in as many as 60%-70% of patients as well as case reports of scrotal eczema[32,52].
The onset of cutaneous toxicity with Sorafenib
HFRS occurs within days or months after starting Sorafenib, but most commonly manifests during the first 6 weeks of therapy[22,26,27]. Rashes usually present on the extremities and/or the trunk within the first to the second month of treatment[22]. Scrotal rashes have been seen between the 2nd and 12th weeks of therapy[22,27]. Alopecia observed in patients treated with Sorafenib occurs within four months of treatment[26,27]. The subungual splinter hemorrhages appear within the first 2 months of treatment[26,27].
It is recommended that physicians see their patients in 2-week intervals for the first 2 months of Sorafenib treatment to manage skin toxicities[20,22].
Dose reductions
The starting dose of Sorafenib is 800 mg daily. Dose reductions for skin toxicity are seen in Tables 1, 2, and 3[38].
LENVATINIB
Lenvatinib cutaneous toxicity and toxicity incidence
In a phase 3 trial, Lenvatinib was shown to be non-inferior to Sorafenib for OS in the first-line treatment of HCC that was not amenable to curative or local therapy[13]. Cutaneous toxicities seen with Lenvatinib include: HFRS (27%, grade 3: 3%), alopecia (3% grade 3: 0%) and rash (10%, grade 3: 0%)[7].
The onset of cutaneous toxicity with Lenvatinib
The onset of Lenvatinib’s cutaneous toxicities for the treatment of HCC has not been described. However,their onset has been documented during the use of Lenvatinib for thyroid cancer[28]. The median time to the first onset of HFSR was 5.9 weeks and 7.3 weeks for rash. Most rashes occurred during the first cycle of therapy. Whereas HFRS could occur throughout therapy.
Dose reductions
Lenvatinib for HCC is dosed depending on body weight with patients 60 kg or greater started at 12 mg daily whereas those less than 60 kg starting at 8 mg daily. Dose reductions for skin toxicities are displayed in Tables 1, 2 and 3[53].
CABOZANTINIB
Cabozantinib cutaneous toxicity and toxicity incidence
Cabozantinib has been approved as second-line therapy for patients with HCC who have progressed on Sorafenib. In phase 3 CELESTIAL trial, Cabozantinib treated patients’ median OS was 10.2 months(95%CI: 9.1-12.0) compared to 8.0 months (95%CI: 6.8-9.4) in patients treated with placebo. Cabozantinib cutaneous toxicities and incidences include: HFRS (46%, grade 3: 17%), stomatitis (13%, grade 3: 2%), and rash (12%, grade 3 < 1%)[6].

Table 1. Hand foot reaction syndrome and tyrosine kinase inhibitor treatment modification
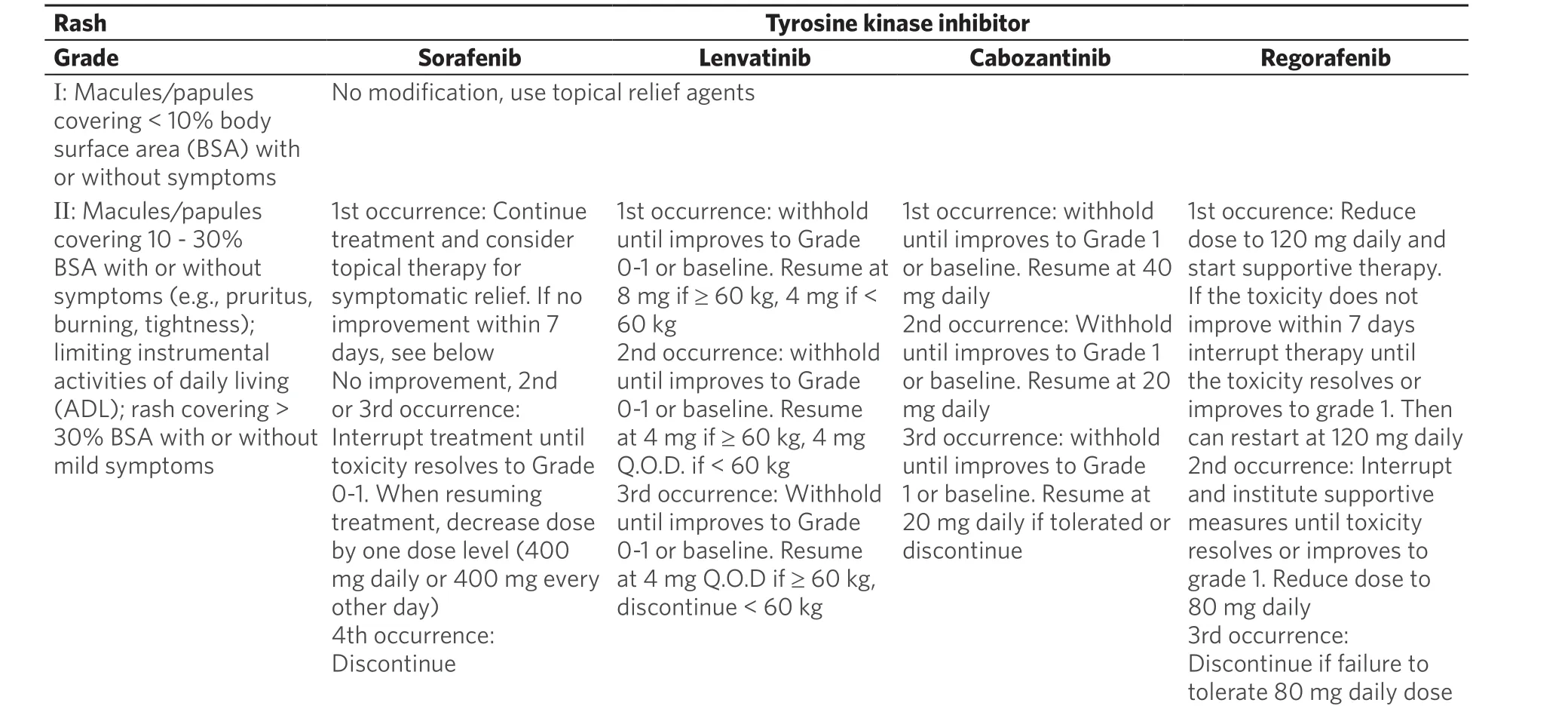
Table 2. Rash and tyrosine kinase inhibitor treatment modifications
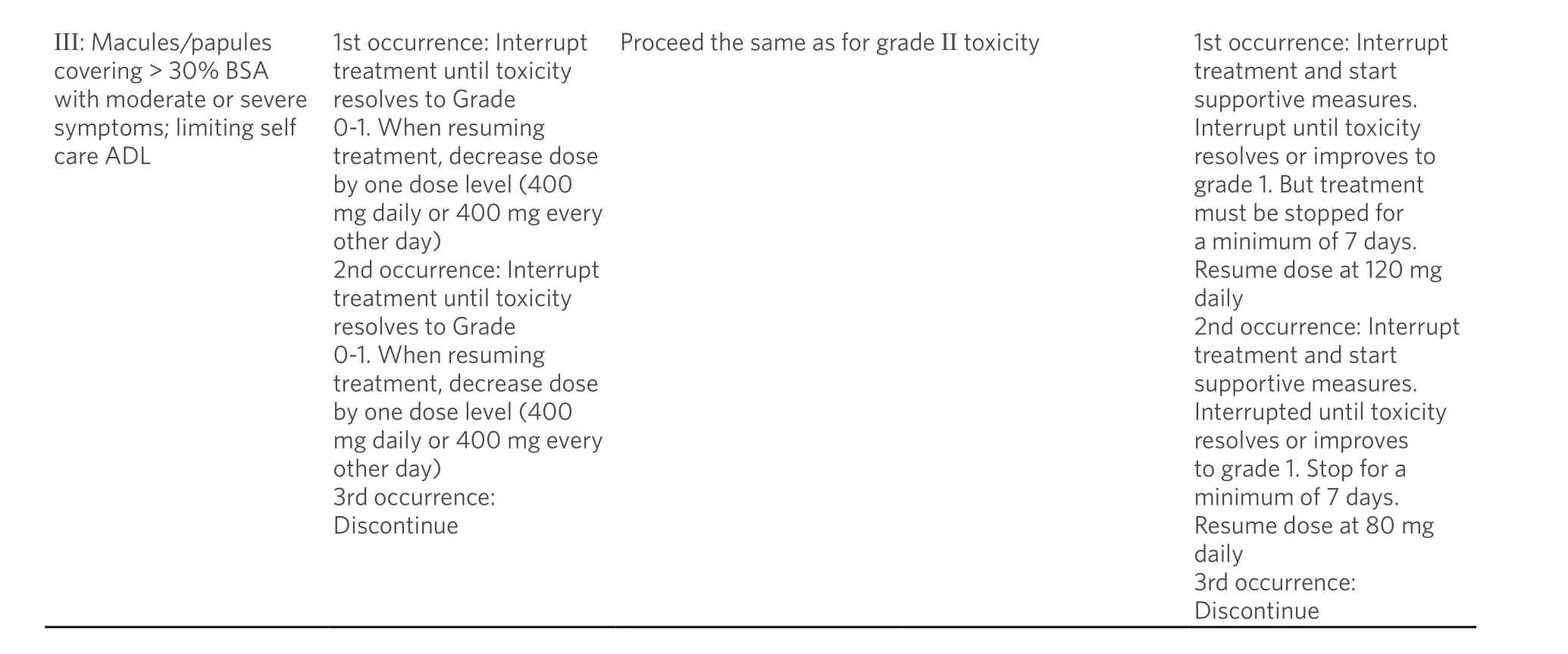
III: Macules/papules covering > 30% BSA with moderate or severe symptoms; limiting self care ADL 1st occurrence: Interrupt treatment until toxicity resolves to Grade 0-1. When resuming treatment, decrease dose by one dose level (400 mg daily or 400 mg every other day)2nd occurrence: Interrupt treatment until toxicity resolves to Grade 0-1. When resuming treatment, decrease dose by one dose level (400 mg daily or 400 mg every other day)3rd occurrence:Discontinue Proceed the same as for grade II toxicity 1st occurrence: Interrupt treatment and start supportive measures.Interrupt until toxicity resolves or improves to grade 1. But treatment must be stopped for a minimum of 7 days.Resume dose at 120 mg daily 2nd occurrence: Interrupt treatment and start supportive measures.Interrupted until toxicity resolves or improves to grade 1. Stop for a minimum of 7 days.Resume dose at 80 mg daily 3rd occurrence:Discontinue
The onset of cutaneous toxicity with Cabozantinib
The onset of cutaneous toxicity with the use of Cabozantinib to treat HCC has not been described.However, the onset has been documented in the treatment of progressive urothelial carcinoma by Zuoet al.[15]and in renal clear cell carcinoma by Choueiriet al.[54]About half of the patients in each study treated with Cabozantinib developed HFRS with a median onset of 4-5 weeks. Additionally In the study by Zuoet al.[15]skin changes, including xerosis and scrotal erythema, developed within approximately 5 weeks of Cabozantinib treatment.
Dose reduction
The starting dose of Cabozantinib is 60 mg daily for the treatment of HCC. Dose reductions for skin toxicities are displayed in Tables 1, 2 and 3[55].
REGORAFENIB
Regorafenib Cutaneous Toxicity and Toxicity Incidence
Regorafenib is another TKI approved for second-line therapy of HCC. The RESORCE trial showed that in patients whose HCC progressed on Sorafenib, those subsequently treated with Regorafenib had improved median OS to 10.6 months (95%CI: 9.1-12.1) compared to 7.8 months (95%CI: 6.3-8.8) in those treated with placebo[5]. A follow up study also found that patients sequentially treated with Regorafenib after Sorafenib had improved OS from the start of Sorafenib treatment to death on study compared to placebo control. 26.0 months (95%CI: 22.6-28.1) for Regorafenib and 19.2 months (95%CI: 16.3-22.8) for placebo[56].
In the RESORCE study, all patients receiving Regorafenib experienced an adverse event. Cutaneous toxicities related to Regorafenib and their incidences include HFRS (53%, grade 3: 13%) and stomatitis (13%grade 3: 1%). Of note, 2% of patients suffering from HFRS discontinued Regorafenib treatment[5].
The onset of cutaneous toxicity with Regorafenib
Regorafenib induced HFRS occurs early in treatment with one study showing a median time to the first occurrence of 15 days[57]. Onset of stomatitis usually occurs between 5 and 14 days after treatment initiation[58].
Monitoring of patients should occur frequently especially early in treatment. Patients should be seen at least every 1-2 weeks during the first two cycles and every 4-6 weeks thereafter[14,59-61].
Dose reduction
The recommended starting dose of Regorafenib is 160 mg daily for 21 days followed by 7 days of a dosing free interval to complete a 28-day cycle. Treatment is continued until disease progression or unacceptable toxicity. Dose reductions with Regorafenib are seen in Tables 1, 2, and 3[62].
The incidences of the most common cutaneous toxicities and their toxicity grade are summarized for each tyrosine kinase inhibitor in Table 4.
ADVERSE EVENTS AND EFFICACY OF TKIS
The relationship between patients experiencing adverse events and treatment efficacy has been noted by multiple investigators. In a study of 65 patients treated with Sorafenib, patients who developed at least grade 1 skin toxicity had tumor control rates of 48.3% versus 19.4% in patients who did not develop skin toxicity[63]. Another study of Sorafenib showed a positive association between higher-grade skin toxicity(> grade 2) and disease control when compared to patients who developed lower grade toxicity or had no skin toxicity[64]. An association was also seen with adverse events and overall survival in patients treatedwith Lenvatinib[65]. Similar results were also noted for Cabozantinib with patients who experienced any grade HFRS having improved median overall survival and progression-free survival compared to those who did not develop HFRS[66]. The development of HFRS and rash was also associated with overall survival in patients treated with Regorafenib for metastatic colorectal cancer[67]. Although these associations have been documented with TKIs, a physiologic relationship has not been described. But it has been postulated that the association between cutaneous toxicity and treatment efficacy could be caused by variations in pharmacokinetics as both the toxicity and the response may be dose-dependent[65]. It has also been suggested that patients who develop skin toxicities may have tyrosine kinase polymorphisms that are more sensitive to drug inhibition which results in greater anti-tumor control but more skin toxicity[61].More investigation is warranted but if treatment efficacy is dose-dependent then symptomatic relief of cutaneous toxicity is warranted to maintain medication compliance to achieve maximum results. However,if treatment efficacy is pre-determined by tyrosine kinase polymorphism then further genetic screening is warranted to determine who will benefit most from TKI therapy.

Table 4. Incidence of TKI induced cutaneous toxicities during HCC therapy

Table 5. Recommendations for adverse event management
CONCLUSION
Tyrosine kinase inhibitors have successfully extended the overall survival in patients with hepatocellular carcinoma[4-7]. However these treatments have been noted to cause severe side effects including liver toxicity, hypertension, gastrointestinal toxicity and the discussed cutaneous toxicities[68]. These cutaneous toxicities tend to occur during the first and second months of treatment and can be managed with symptomatic treatment and dose reductions if necessary. Additional prophylactic measures can help prevent the manifestation of the some of most common cutaneous toxicities including HFRS and stomatitis. It is in these authors’ opinions on and others that the monitoring of TKI treated patients for cutaneous toxicities should be conducted every 2 weeks for the first few months of treatment and a baseline dermatological exam is also necessary[22,58,68]. A summary of recommendations for the management of cutaneous adverse events are displayed in Table 5. As cutaneous toxicities have also been seen with more recently developed TKIs, including Afatinib and Dorafenib, it appears as more TKIs are used to treat HCC that these cutaneous toxicities will remain as treatment side effects requiring careful management[69,70].
DECLARATIONS
Authors’ contributions
Made substantial contributions to conception and design of the review article: Silk T, Wu J
Availability of data and materials
Not applicable.
Financial support and sponsorship
None.
Conflicts of interest
All authors declared that there are no conflicts of interest.
Ethical approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Copyright
© The Author(s) 2020.
杂志排行
Hepatoma Research的其它文章
- Stereotactic body radiation therapy for primary liver tumors with adverse factors
- Immunotherapy of hepatocellular carcinoma with infection of hepatitis B or C virus
- Systemic therapy for advanced cholangiocarcinoma:new options on the horizon
- Post liver transplant recurrence in patients with hepatocellular carcinoma: not necessarily the end of the road!
- The transcontinental variability of nonalcoholic fatty liver disease
- Prognostic ability of inflammation-based markers in radioembolization for hepatocellular carcinoma
