Mesonephric adenocarcinoma of the uterine cervix with rare lung metastases:A case report and review of the literature
2020-05-13LiLiJiangDeMingTongZiYiFengKuiRanLiu
Li-Li Jiang, De-Ming Tong, Zi-Yi Feng, Kui-Ran Liu
Li-Li Jiang, Kui-Ran Liu, Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang 110004, Liaoning Province, China
De-Ming Tong, Department of General Surgery, Northen War General Hospital Heping Branch Hospital, Shenyang 110004, Liaoning Province, China
Zi-Yi Feng, College of Clinical Medicine Science, China Medical University, Shenyang 110013, Liaoning Province, China
Abstract
Key words: Cervical cancer;Mesonephric adenocarcinoma;Lung metastasis;Case report;Human papillomavirus;Cervix
INTRODUCTION
In early embryologic development, the mesonephric ducts play a pivotal role in the sexual differentiation.The mesonephric ducts give rise to the internal genitalia,including the epididymis, the vasa deferentia, the seminal vesicles, and the ejaculatory ducts in males.In females, in the absence of testis, the mesonephric ducts regress with some remnants persisting in the broad ligament, mesosalpinx, hilus ovarii, cervix, and vagina, but have no known function[1,2].Mesonephric adenocarcinoma (MNA) is considered to be the malignant transformation of mesonephric remnants and occurs in the distribution of mesonephric remnants (most common in the cervix)[3].Studies have shown that MNA occurs most often in adult women.The most frequent presenting symptom is abnormal vaginal bleeding, often with a visible cervical lesion[4].Only 48 MNAs have been reported in the literature,including the present case (Table 1);however, cases with pulmonary metastases are rare.We report a 48-year-old woman in whom an MNA was incidentally detected intra-operatively and she received postoperative chemotherapy.Rare lung metastases arose during follow-up.In addition, we performed a review of the existing literature.
CASE PRESENTATION
Chief complaint
A 48-year-old gravida 2 para 1 woman was admitted to our hospital for evaluation of an enlarged right inguinal mass and right adnexal cyst on physical examination.
History of present illness
The patient was admitted to our hospital for evaluation of an enlarged right inguinal mass and right adnexal cyst on physical examination.The right inguinal mass was first discovered two years ago and increased gradually.The right adnexal cyst was found by physical examination at another hospital half a month ago.There was no irregular vaginal bleeding, menstrual changes, or lower abdominal pain.The cervical ThinPrep cytological test (TCT) and human papillomavirus (HPV) testing were completed in the clinic, and the results were normal.
History of past illness
The patient underwent hemorrhoids surgery more than 10 years ago.She denied the history of diseases such as hypertension, diabetes, and heart disease.
Personal and family history
The patient’s personal and family history was unremarkable.
——加大大病保险倾斜力度,对农村贫困人口降低起付线50%、提高支付比例5个百分点、逐步提高并取消封顶线。
Physical examination upon admission
Body temperature, blood pressure, heart rate, respiratory rate, oxygen saturation, and chest examination were all normal.
Gynecologic examination
The vulva developed normally, and the vaginal unobstructed.The cervical size was normal, the surface was smooth, and there was no contact bleeding.A cystic mass of 5 cm × 3 cm was palpable in the right groin and could not return when recumbent.The uterus was anterograde with an irregular shape and poor activity.A cystic mass about 4 cm in diameter, irregular in shape and not tender, was palpable in the right adnexa.
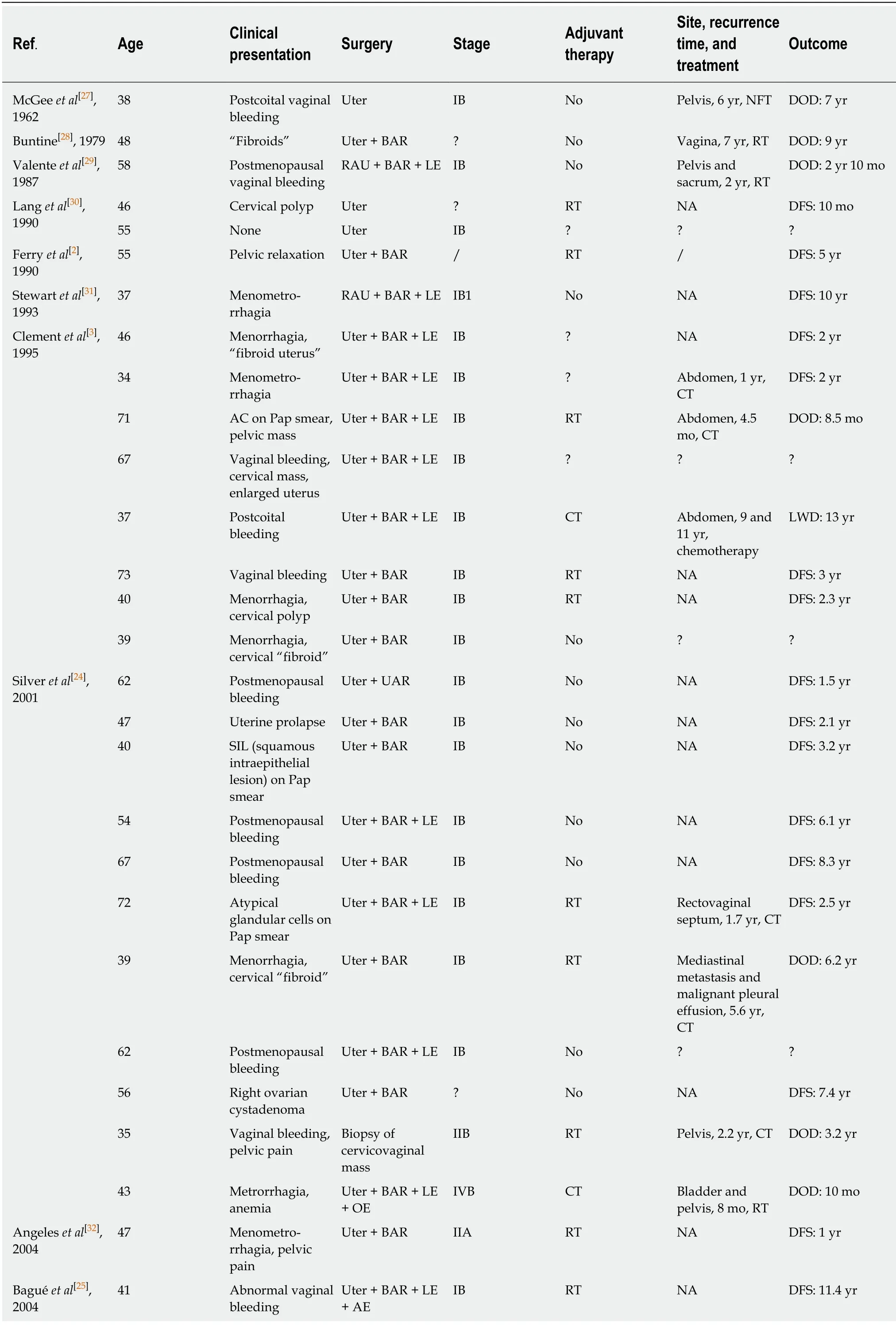
Table 1 Summary of cases of mesonephric carcinoma of the cervix
Laboratory examinations
On routine laboratory testing, the serum levels of CA-125, carcinoembryonic antigen(CEA), CA19-9, CA724, and alpha fetoprotein were within the normal ranges.
Imaging examinations
Transvaginal ultrasound revealed a cystic mass (4.3 cm × 2.3 cm) in the right adnexa and a few moderate echo clusters attached to the wall of the cystic mass, the largest of which was 0.8 cm × 0.7 cm in size.For further clarifying the diagnosis, the pelvic cavity magnetic resonance imaging examination was completed.It revealed a liquid area in the right iliac fossa (2.7 cm × 1.3 cm × 2.6 cm) (Figure 1A and B).Oval mixed signal shadows with a slightly longer T1 and T2 signal were observed in the right adnexal area, with a size of 2.6 cm × 3.0 cm and no enhancement after intensification(Figure 1C and D).
Pathological examination
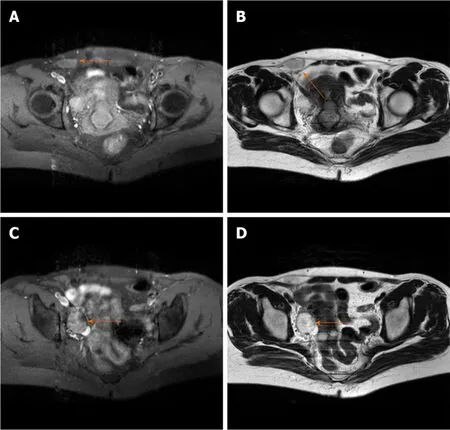
Figure 1 Pelvic cavity magnetic resonance imaging.
Grossly, a 4 cm × 3 cm tumor occupied the cervical canal and infiltrated the full thickness of the myometrium of the lower uterine body.The papilla in the inner wall of the right ovary was approximately 1 cm in size.Microscopically, atypical cells were seen, and the lesion infiltrated tubular and papillary structures in the cervix (Figure 2A).The tumor cells in the right ovary exhibited the same pattern of the cervix,suggesting that they may have metastasized from the cervix (Figure 2B).The immunohistochemical findings showed positive reactions in the tumor cells for CD10(Figure 2C and D), and focal positivity for pancytokeratin (CK) and calretinin.The Ki-67 proliferation index was slightly increased.The pathological examination revealed a malignant tumor in the lower uterine segment and cervical canal (middle renal duct adenocarcinoma was considered), and right ovarian metastasis, with no lesions and metastases found in the remaining resected tissues and lymph nodes.
FINAL DIAGNOSIS
The final diagnosis was an MNA of the lower uterine body and cervix with right ovarian metastatic cancer.
TREATMENT
The patient underwent an exploratory laparotomy.We noted that a 5 cm × 3 cm protuberant cyst of the right lower abdomen femoral sulcus extending to the round ligament and a cyst with an intact capsule had formed on the right ovary,approximately 4.5 cm × 3 cm in size.Thus, resection of the cyst in the right round ligament and a right adnexectomy were performed.Frozen section pathology reported a serous cystadenoma of the ovary with malignant transformation.Therefore, a hysterectomy, left salpingo-oophorectomy, pelvic lymphadenectomy,omentectomy, and appendectomy were performed.The patient received six cycles of adjuvant chemotherapy after surgery.
OUTCOME AND FOLLOW-UP
Thirty-two months later, multifocal lung nodules were found and confirmed to be metastatic lesions by puncture biopsy (Figure 3A-D).The patient underwent chemotherapy.She is currently alive and well undergoing targeted drug treatment.

Figure 2 lmmunohistochemical findings.
DISCUSSION
In early embryologic development, the mesonephric duct (also known as the Wolffian duct) plays a key role during the sexual differentiation stage.In males, the mesonephric duct gives rise to the internal genitalia, including the epididymis, vasa deferentia, seminal vesicles, and ejaculatory ducts.In females, the mesonephric ducts regress in the absence of testosterone.The remnants persist along the following trajectory, with the most common site being the cervix:The broad ligament;mesosalpinx;hilus ovarii;cervix;and vagina[1,2].The remnants of the mesonephric duct are often located in the lateral wall of the cervix but may also involve the entire cervix.MNA of the cervix is a rare tumor considered to be the malignant transformation of mesonephric remnants[4].To the best of our knowledge, 48 cases of cervical MNA have been reported in the literature, including our case (Table 1).
Studies have shown that MNA most often occurs in adult females.Of the 48 cases reviewed herein, the age ranged from 24-73 years, with an average age of 52.7 years.The most common symptom of MNA is abnormal vaginal bleeding from cervical lesions[4].Among the 48 cases (including this case), 17 had postmenopausal vaginal bleeding, 8 had menorrhagia, and 3 had postcoital vaginal bleeding initially.Other clinical manifestations include cervical masses and abnormal smears.There is a rare case of MNA which originally presented as pulmonary nodules.In addition, three cases in asymptomatic patients were detected incidentally.The patient reported herein was asymptomatic and MNA was noted intra-operatively and confirmed postoperatively.Unlike common squamous epithelial carcinoma, this type of cervical cancer is rarely discovered by cytologic testing.The age of onset is late and the incidence does not decrease with aging[5].Cervical cancer screening is the most important method in cancer prevention.Screening tests such as the Papanicolaou test(Pap smear) and TCT reduced the incidence and increased the 5-year survival rate of cervical cancer significantly[6].However, the accuracy of the current cervical cancer screening tests still needs to improve.In recent years, more biomarkers have shown their potentials in the screening, diagnosis, and monitoring of cervical cancer.Zhenget al[7]reported that plasma exosomal miR-30d-5p and let-7d-3p are valuable diagnostic biomarkers for non-invasive screening of cervical cancer and its precursors.Blood extraction is more convenient than TCT or Pap smear tests.They are expected to be applicated in clinical diagnosis with larger samples further[7].The differentially expressed miRNAs and related target genes analyzed by Gaoet al[8]prompted that they may be used as promising biomarker for the early screening of high-risk populations and early diagnosis of cervical cancer.In this way, we can offer better screening, diagnosis, and prognosis to the patients.

Figure 3 Thirty-two months later, multifocal lung nodules were found.
The mesonephric remnants of the cervix were first identified incidentally in total hysterectomy and cervical conization specimens;22% of mesonephric remnants reported were in the adult cervix[2,9].The remnants occasionally become hyperplastic,but rarely develop into MNA.Now, five categories of cervical mesonephric lesions have been described, as follows:Mesonephric remnants;lobular mesonephric hyperplasia;diffuse mesonephric hyperplasia;mesonephric ductal hyperplasia;and mesonephric carcinoma[10].Mesonephric remnants usually present with a lobular structure.The glandular duct has no cilia and is covered by a single layer of cuboidal epithelium.Eosinophilic secretions can be noted in the lumen.In the case of mesonephric hyperplasia, the number of glandular ducts increases, which can be divided into three categories according to the microscopic morphology:Lobular hyperplasia;diffuse hyperplasia;and ductal hyperplasia.Lobular hyperplasia(lobular growth) is characterized by multiple elongated tubules embraced by lobules.In 90% of cases, hyaline material that is pink in color and periodic acid Schiff reactionpositive can be seen in the lumen.The type of diffuse hyperplasia is rare.The number of mesonephric tubes is large and scattered, which can be easily misdiagnosed as adenocarcinoma, but the epithelial cells have no atypia or mitoses.Ductal hyperplasia is a feature of large ducts (single or multiple layers of pseudo epithelium), and there are often microscopic papillary changes in the epithelium[11,12].
MNAs usually present with florid mesonephric hyperplasia and a densely eosinophilic luminal secretion[13].Various morphologic patterns may be present, such as tubular, glandular, papillary, and reticular.MNAs show carcinomatous cell manifestations, with back-to-back arranged glands, blood vessels, and peripheral nerve infiltration.Residual mesonephric ducts around the tumor and most macroscopic mass can be seen[14].MNA should be distinguished from florid mesonephric hyperplasia[15].The former is rarer and MNA must be diagnosed after ruling out florid mesonephric hyperplasia.Sometimes, heteromorphic cells can be seen under the microscope, but the nuclear division does not exceed 1/10 high power fields[3,11].
In recent years, our gradual understanding and the increased number of MNA cases reflect the value of immunohistochemistry.If the morphologic diagnosis cannot be confirmed, immunohistochemistry can help further diagnose the disease.The immunochemical features of MNA include positivity for CAM5.2, CK7, and EMA,and reactivity for calretinine and CD10.CEA, CK20, estrogen receptor (ER), and progesterone receptor (PR) are usually negative[16].The primary value of CD10 immunostaining is to support a mesonephric origin when positive in a benign cervical lesion[17].Specifically, Cavalcantiet al[18]reported a previously unreported case of mixed MNA and high-grade neuroendocrine carcinoma of the uterine cervix in which calretinin was negatively expressed.It is well-known that HPV infection is closely related to the occurrence of cervical cancer;however, p16 is negative in MNA, thus p16 is not associated with high-risk HPV infections[19].PAX8 expression is strongly positive in both benign and malignant mesonephric lesions, while in common pathologic types of cervical adenocarcinoma, PAX8 is expressed in a variety of ways.Because PAX8 is expressed in a variety of lesion types, it is not reliable in the identification of benign and malignant cervical lesions[17].The immunoreactivity of PAX2 appears to be absent in MNA and cervical adenocarcinoma with the least variation, but PAX2 is diffusely positive in mesonephric hyperplasia, which can be used to distinguish mesonephric hyperplasia and MNA[12].As a transcription factor that plays an important role in the process of embryogenesis, development, and differentiation, GATA3 has been reported to be highly sensitive and specific to mesonephric lesions in the lower reproductive tract of females.GATA3 expression may be a marker of mesonephric lesions because it has been shown to be positive in all mesonephric remnants and hyperplasia and nearly all mesonephric carcinomas tested, and infrequent or absent in endocervical adenocarcinomas (usual and gastric types)[20-22].
The mixture of morphologic patterns is one of the most characteristic features of MNA.Therefore, its differential diagnoses include clear cell adenocarcinoma,endometrioid adenocarcinoma, serous adenocarcinoma, minimal deviation adenocarcinoma (malignant adenoma), and mesonephric hyperplasia[23].The biggest challenge of diagnosis proposed in the literature is to distinguish MNA from clear cell carcinoma[10];however, clear cell carcinomas usually present as cystic, papillary, or solid structures of varying degrees, which were previously classified as mesonephric carcinoma.Clear and nail cells are not present in mesonephric carcinoma, and there were no mesonephric remnants or hyperplasia around the tumor.Immunohistochemical staining for ER and PR can be positive, but CD10 is negative[23].When the MNA has an apparent ductal type, the MNA must be distinguished from endometrioid carcinoma of the cervix.If there are mesonephric remnants around the tumor and a lack of squamous cells, an MNA is likely to be diagnosed and immunohistochemical staining for ER, PR, and CEA are negative in MNA[24].The epithelium of MNA is sometimes similar to serous carcinoma, but the nuclear atypia of serous carcinoma is more evident and there are no eosinophilic substances in the lumen.Minimal deviation adenocarcinoma (adenoma malignum) includes abnormally-shaped endocervical glands embraced by characteristic benign mucinsecreting cells, whereas in mesonephric cells the intracellular mucin is almost absent[25].In contrast to mesonephric hyperplasia, MNA has no lobule structures and the nuclei present as a cytologic malignancy.The Ki-67 proliferation index is < 1% in hyperplasia and 15%-20% in MNA[24].
There is no explicit treatment for this rare disease.Based on the current cases described in the literature, treatment of MNA depends on its stage.The methods of operation include uterectomy with or without bilateral adnexal resection, pelvic lymphadenectomy, and adjuvant chemo- or radio-therapy[4].Among the 48 cases retrieved in this paper (including the present case), 33 were diagnosed as stage I(69%).All stage I patients underwent total hysterectomies, and postoperative adjuvant radiotherapy was administered to 8 patients, chemotherapy administered to 2, and combined radiotherapy and chemotherapy to 1.There was no significant difference in disease-free survival time between stage I patients receiving adjuvant therapy and those without adjuvant therapy.
Due to the rarity of cervical MNA, the biological behavior and prognosis of these tumors are unclear.It has been reported that the prognosis of MNA is worse than that of other histologic types.Previous studies have shown that the recurrence rate of stage I MNA patients is 32%, while the recurrence rates of early cervical adenocarcinoma and cervical squamous cell carcinoma are 16% and 11%,respectively[4,26].In the 48 cases reported in the literature, 15 (31.25%) had recurrences,with an average recurrence time of 2.8 years.The recurrence sites were diverse, most of which were the pelvis and abdominal cavity, and there were only two cases of lung metastasis, including the present case.Combined with previous studies, we can reasonably manage and closely follow patients with MNA of the cervix according to the current guiding principles of similar stages and pathologic results of cervical adenocarcinoma.
CONCLUSION
Combined with the cases retrieved in this paper, cervical smear examination of patients with MNA is often negative, most of which are confirmed by cervical biopsy or cone resection.The case reported herein had no cervical abnormalities, and the TCT and HPV tests were both negative.During surgery, the accessory masses were removed as planned and malignant changes were demonstrated, but the source could not be determined.Therefore, MNA with ovarian metastasis was diagnosed based on paraffin-embedded specimens postoperatively.After adjuvant treatment, rare lung metastases were detected after 2.8 years.We will continue to follow the patient.Therefore, the diagnosis is difficult.In future clinical studies, attention should be paid to the occurrence of rare cervical disease without symptoms.Continuous research should be conducted to increase the experience of diagnosis and treatment of this disease for the benefit of patients.
ACKNOWLEDGEMENTS
We thank the China Medical University for its support and the patient for permitting us to use her data to complete this article.
猜你喜欢
杂志排行
World Journal of Clinical Cases的其它文章
- Nutrition management in acute pancreatitis:Clinical practice consideration
- Bone disease in chronic pancreatitis
- Role of microRNAs in the predisposition to gastrointestinal malignancies
- Recurrent anal fistulas:When, why, and how to manage?
- Removal of biofilm is essential for long-term ventilation tube retention
- Neutrophil gelatinase-associated lipocalin does not predict acute kidney injury in heart failure
