Durable response to pulsatile icotinib for central nervous system metastases from EGFR-mutated non-small cell lung cancer:A case report
2020-04-22HuiYingLiYuXieTingTingYuYongJuanLinZhenYuYin
Hui-Ying Li, Yu Xie, Ting-Ting Yu, Yong-Juan Lin, Zhen-Yu Yin
Hui-Ying Li, Yu Xie, Ting-Ting Yu, Yong-Juan Lin, Zhen-Yu Yin, Department of Geriatric Oncology, Affiliated Nanjing Drum Tower Hospital of Nanjing University Medical School,Nanjing 210008, Jiangsu Province, China
Abstract
Key words: Non-small cell lung cancer; Central nervous system metastases; EGFR mutation; Pulsatile icotinib; Case report
INTRODUCTION
Central nervous system (CNS) metastases are a catastrophic complication of nonsmall cell lung cancer (NSCLC), including brain and leptomeningeal carcinomatosis.The incidence of brain metastases (BM) is 10%-40% in NSCLC patients, and the median overall survival (OS) time is estimated to be 7 mo[1,2].Leptomeningeal metastases (LM) are relatively rare, with an approximate incidence of 3%-5% among patients with NSCLC, but always imply a poor prognosis, with a median OS of only 3 mo[3,4].
The main treatment options for CNS metastases include tyrosine kinase inhibitors(TKIs), systemic chemotherapy, whole-brain radiotherapy (WBRT), intrathecal chemotherapy, and combined therapies.For epidermal growth factor receptor (EGFR)mutation-positive patients, TKIs are a standard treatment and have a high response rate.Icotinib hydrochloride, a highly specificEGFR-TKI, has shown reliable antitumour activity and has been approved as the firstline choice in advancedEGFR+NSCLC patients by the State Food and Drug Administration of China[5,6].Herein, we report the first case of a patient with CNS metastases fromEGFR-mutant NSCLC who benefited from “pulsatile” administration of high-dose icotinib after the invalidity of standard daily dosage.
CASE PRESENTATION
Chief complaints
A 68-year-old Asian male non-smoker presented with paroxysmal cough in December 2014.
History of present illness
He had no history of fever, hemoptysis, or weight loss.
History of past illness
He had no history of surgery, chronic diseases, or allergies.
Personal and family history
He had no smoking or drinking history.There was no specific family history of cancer or cancer related disease.
Physical examination upon admission
Physical examination was basically normal.
Laboratory examinations
Carcinoembryonic antigen level was 12.5 ng/mL (0-10 ng/mL), neuron-specific enolase was 15.9 ng/mL (0-16.3 ng/mL), and cytokeratin 19 fragment (CYFRA21-1)was 15.5 ng/mL (0-3.3 ng/mL).
Imaging examinations
Chest computed tomography (CT) showed a space-occupying lesion in the right upper lobe of the lung.
FINAL DIAGNOSIS
Lung cancer.
TREATMENT
Radical surgery by video-assisted thoracoscopic surgery (VATS) was carried out in January 2015.The clinical stage was pT2N2M0 IIIA according to the postsurgical pathology.Adjuvant chemotherapy with pemetrexed and oxaliplatin was applied for six cycles.The disease was controlled for over a year until August 2016, when the patient showed symptoms of headaches, nausea, and vomiting.The brain and leptomeningeal metastases were diagnosed by magnetic resonance imaging (MRI)(Figure 1).EGFRtesting revealed an exon 21 L858R point mutation.Icotinib 125 mg(three times daily) was administered orally, which decreased the CEA levels, relieved neurological symptoms, and stabilized the disease for 12 mo.However, a repeat MRI scan revealed enlarged brain lesions in August 2017 (Figure 2).After obtaining written informed consent, icotinib was adjusted to 1125 mg every 3 d.
OUTCOME AND FOLLOW-UP
The patient tolerated this treatment well, and the clinical symptoms of nausea,vomiting, and headaches were gradually alleviated.The value of his CEA remained in the normal range, and MRI findings exhibited significantly shrunken CNS lesions(Figure 3) without any notable side effects during treatment.At the last follow-up in September 2019, a repeat MRI scan of the brain revealed further reduced lesions(Figure 4).
DISCUSSION
At present, it is generally recognized thatEGFR-TKIs are a standard first-line therapy for NSCLC patients with targetedEGFRmutations, and they could significantly prolong the survival time[7].New-generation TKIs, such as osimertinib, have better CNS permeability and control rates[8].However, the therapy of CNS (brain and/or leptomeningeal) metastases from NSCLC is still challenging.
The main reason for progressive systemic disease in patients treated with TKIs is acquired TKI resistance, such as the T790M mutation, which is detected in two-thirds of all TKI tumour samples[9].It is worth noting that there is different expression of the T790M mutation in the CNS and extra-CNS sites.Some studies have shown that the T790M mutation rate is lower in intracranial lesions than in extracranial lesions[10,11].Therefore, it appears that the cause of CNS progression is different from the mechanisms of systemic progression.
Due to the restriction of the blood brain barrier (BBB), generations of TKIs have shown limited clinical efficacy within the CNS, especially in non-selected patients.Pharmacologic studies suggest that the cerebrospinal fluid (CSF) concentrations are higher in patients with CNS tumours than those in normal primates because of the disruption of the BBB caused by brain metastasis[12].Antitumour drugs still cannot reach sufficient drug concentrations in the brain parenchyma for BM or in CSF for LM.Thus, improving the penetration into the protected space is considered the key for successful CNS metastasis treatment.
Icotinib hydrochloride is the first small-moleculeEGFR-TKI exploited by the Chinese company[5,6].The phase 4 ICOGEN trial has confirmed the efficacy and safety of icotinib in patients with advanced NSCLC.InEGFR-mutated patients, the objective response rate (ORR) and disease control rate (DCR) were 49.2% (327/665) and 92.3%(614/655), respectively[13].Another two studies showed that in patients with advancedEGFR+ NSCLC, progression-free survival (PFS) associated with icotinib was longer than that with gefitinib and cisplatin/pemetrexed plus pemetrexed maintenance therapy[14,15].In addition, icotinib showed positive efficacy in the patients with acquiredEGFRLeu792H mutation after becoming resistant to the third-generation TKIs[16].For CNS disease treatment, some studies have indicated that icotinib has definite efficacy and could provide survival benefits[17,18].A phase 3 trial (BRAIN) was conducted to compare the antitumour activity between icotinib and WBRT in patients with multiple CNS metastases fromEGFR-mutant NSCLC.The median intracranial PFS of the icotinib group (10.0 mo) was much longer than that of the WBRT group (4.8 mo)[19].Furthermore, the combined treatment of icotinib and WBRT could further prolong the survival of the patients without increasing the occurrence of toxicity[20,21].However, drug resistance inevitably develops after 6-12 mo of treatment[22,23].A new therapeutic strategy is desperately in demand to overcome resistance.
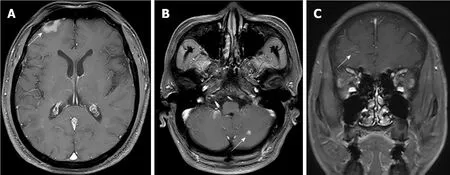
Figure 1 Baseline axial (A and B) and sagittal (C) T1w C+ craniocerebral magnetic resonance imaging showed the central nervous system metastases in the right frontal lobe (brain metastases and leptomeningeal metastases) and left cerebellar hemisphere (brain metastases) (white arrows).
Pulsatile administration, applying a high dose of medicine in a short time, has been effective for patients with TKI secondary drug resistance[24,25].Several studies demonstrated that pulsatile erlotinib had a proven impact on CNS metastasis inEGFR+ patients, with a median PFS of 2.7 mo, but median OS had no apparent difference from that of patients treated with standard-dose erlotinib[25-27].Liuet al[28]reported that higher-dose icotinib has good tolerability, practicability of long-period treatment, remarkable antitumour activity, and a favourable pharmacological profile.The present case obtained stable clinical remission for 12 mo with a standard dosage of icotinib (125 mg three times daily).Then, CNS lesions developed despite stable systemic control.He could not afford to try other expensive TKI.Thus, after full consultation with the patient, off-label pulsatile icotinib (1125 mg every 3 d) was administered.Until now, this new usage has lasted 25 mo and achieved a complete remission of neurological symptoms and almost vanished lesions without notable side effects.
This new mode for administration has the advantage that drug concentration in CSF and blood accumulates rapidly and effectively, which ensures adequate CSF penetration and better antitumour activity.When systemic disease is steady, pulsatile icotinib at an increased dose could overcome the drug resistance and is worth considering for isolated CNS progression.
CONCLUSION
In summary, pulsatile high-dose icotinib was well-tolerated, and achieved durable symptomatic remission, reduced CEA levels, and almost vanished lesions in this case.More clinical cases and further prospective studies are warranted to assess its safety and validity for treating CNS metastases from refractoryEGFR-mutant NSCLC.

Figure 2 Repeat axial (A and B) and sagittal (C) T1w C+ craniocerebral magnetic resonance imaging in August 2017 showed significantly enlarged lesions(white arrows).

Figure 3 Repeat axial (A and B) and sagittal (C) T1w C+ craniocerebral magnetic resonance imaging in May 2018 showed distinctly shrunken lesions(white arrows).

Figure 4 Repeat axial (A and B) and sagittal (C) repeat T1w C+ craniocerebral magnetic resonance imaging in September 2019 showed almost vanished lesions (white arrows).
杂志排行
World Journal of Clinical Cases的其它文章
- Awareness during emergence from anesthesia:Features and future research directions
- Risk factors for adverse cardiac events in adults with fulminant myocarditis during hospitalization
- Malignant tumors associated with Peutz-Jeghers syndrome:Five cases from a single surgical unit
- Pathogens causing diarrhoea among Bangladeshi children with malignancy:Results from two pilot studies
- One-year rotational relapse frequency following conventional circumferential supracrestal fiberotomy
- LINX® reflux management system to bridge the “treatment gap” in gastroesophageal reflux disease:A systematic review of 35 studies
