Recurrent lymphoma presenting as painless, chronic intussusception:A case report
2020-04-22ParkerGirouxAndersonCollierMichaelNowicki
Parker Giroux, Anderson Collier, Michael Nowicki
Parker Giroux, Department of Pediatrics, University of Mississippi Medical Center, Jackson,MS 39216, United States
Anderson Collier, Division of Pediatric Hematology and Oncology, University of Mississippi Medical Center, Jackson, MS 39216, United States
Michael Nowicki, Division of Pediatric Gastroenterology, University of Mississippi Medical Center, Jackson, MS 39216, United States
Abstract
Key words: B-cell acute lymphoblastic leukemia; Tumor relapse; Intussusception; Case report; Anemia
INTRODUCTION
Gastrointestinal (GI) involvement by hematologic cancers (leukemia and lymphoma)related to malignant infiltration of the intestinal mucosal-associated lymphoid tissue is well documented.GI complications arising from these cancers include typhlitis,intestinal perforation, hemorrhage, and intussusception.Intussusception has been described both as the initial presentation of the cancer or as a later complication,almost universally presenting with abdominal pain due to bowel obstruction as a major symptom.Various diagnostic imaging studies have been used to diagnose intussusception, however, on rare occasions unsuspected intussusception has been made colonoscopy.Surgical resection or biopsy are the principle modes of documenting lymphoma as the underlying cause of intussusception when present.We report an adolescent with a history of acute lymphoblastic leukemia (ALL) who presented with anemia and was found at colonoscopy to have intussusception due to recurrent lymphoma.
CASE PRESENTATION
Chief complaint
A 13-year-old white male presented with iron-deficiency anemia and weight loss.
History of present illness
The patient had a past medical history of B-cell precursor ALL at 2-years of age.He achieved remission in 28 mo after completing standard risk chemotherapy treatment for ALL with doxorubicin and cyclophosphamide.At 7-years of age he developed cough, shortness of breath, and tiring easily.Echocardiogram was normal.Three months later he presented to the pediatric emergency room due to worsening pulmonary symptoms; a chest-x-ray showed hilar adenopathy and right-sided pleural effusion.Echocardiogram showed a large mass in the right atrium with a pericardial effusion.Computed tomography (CT) scan of the neck, chest, abdomen and pelvis with contrast revealed a 4.5 cm right sided mediastinal mass extending into the right atrium causing obstruction of the superior vena cava, right main pulmonary artery,and distal airway compression with paratracheal and mediastinal adenopathy.Flow cytometry was non-diagnostic for malignancy and bone marrow aspirate showed no evidence of infiltrative disease.Cardiac catheterization and biopsy of the tumor was initially interpreted as inflammatory myofibroblastic tumor, and chemotherapy was initiated with ifosfamide, doxorubicin, and celecoxib which achieved a decrease in tumor size.Following three courses of scheduled chemotherapy, cardiovascular surgery performed tumor resection.Final pathology was consistent with necrotic lymphoma consistent with recurrent B-cell lymphoma.He completed chemotherapy and began maintenance therapy.Eighteen months later he presented with weight loss and anemia.
Approximately 18-mo later, at 13 years of age, he was seen in pediatric gastroenterology clinic for iron-deficiency anemia, decreased oral intake, and weight loss of 5.7 kg.He did not have fatigue, malaise, shortness of breath, palpitations,melena, hematochezia, or abdominal pain.
Personal and family history
The patient was a student in good standing.Family history was negative for inflammatory bowel disease, polyp syndromes, and bleeding dyscrasias.
Physical examination
On physical examination he had no tachycardia or cardiac murmur, his lungs were clear to auscultation, his abdomen was soft, non-tender, without hepatosplenomegaly,there was no bruising, digital rectal exam revealed brown stool that was positive for fecal occult blood.
Laboratory examinations
Complete blood count revealed a normal white blood cell count (9200/mm3),microcytic anemia (hemoglobin = 9.0 g/dL, hematocrit = 30.9%, mean corpuscular volume = 61 fL), and thrombocytosis (platelets = 726000/mm3).Other laboratory values were normal including a liver panel, renal panel, lactate dehydrogenase and uric acid.
Imaging examinations
The patient underwent esophagogastroduodenoscopy (EGD) and colonoscopy.EGD results were unremarkable; however, a large, firm mass in the mid-ascending colon was discovered on colonoscopy and subsequently biopsied (Figure 1).The biopsy confirmed recurrent B-cell ALL.CT scan showed ileo-colonic intussusception (Figure 2) with the mass acting as the lead points.Pathology results showed a recurrent B-cell lymphoma in the ileum causing chronic intussusception.
FINAL DIAGNOSES
The final diagnosis was ileocolic intussusception due to intestinal relapse of B-cell ALL.
TREATMENT
The patient was admitted and started on chemotherapy including intrathecal methotrexate, cytarabine, and clofarabine.
OUTCOME AND FOLLOW-UP
His hospital course was complicated by febrile neutropenia, thrombocytopenia,anemia, and clostridium difficile infection.The patient was minimally responsive to chemotherapy, and palliative right hemicolectomy with primary anastomosis was performed 3 mo after diagnosis.This procedure was complicated by anastomotic leak,so the patient underwent bowel resection with ileostomy.The patient and family initially planned to proceed with bone marrow transplant.However, the patient no longer desired to pursue chemotherapy or transplant and was transferred to hospice care where he passed away 5 mo after relapse.
DISCUSSION
We report our patient to alert physicians to the subtlety to which intussusception can present, as well as to highlight the rare presentation and unusual diagnostic method utilized.Our patient was in remission and developed anemia, but was otherwise asymptomatic.He was found to have occult blood in his bowel movements.He underwent EGD and colonoscopy as part of the investigation and was found to have a luminal mass, biopsy proved to be a lymphoma.Colonoscopy as a modality for the diagnosis of intestinal lymphoma has only been reported once to date[1].After making the diagnosis of relapsed lymphoma in the small intestine as the cause of intussusception, we performed a literature search and found three large retrospective reviews and a number of case reports/series describing intussusception related to hematologic cancers in children.We review and report on the clinical features of intussusception related to hematologic cancers.
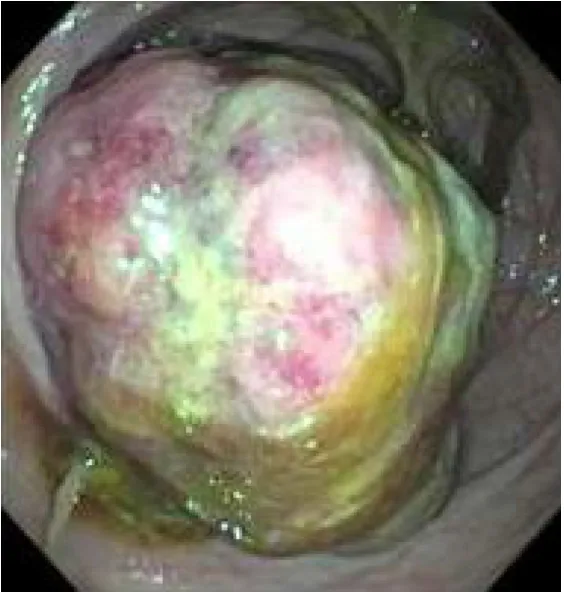
Figure 1 Findings at colonoscopy.
Intussusception resulting from GI involvement in hematologic cancers (leukemia and lymphoma) is a well-described, yet occurs rarely.In a retrospective review of 378 children identified with intussusception over 31-years, only 1.6% were found to have lymphosarcoma as a lead point[2].In two large retrospective reviews of children with Burkitt's lymphoma, the prevalence of developing intussusception was 6.7% in one study and 17.5% in the other[3,4].In a smaller study of children with primary abdominal non-Hodgkin's lymphoma, 25% developed intussusception[5].Intussusception has been reported less frequently in children with leukemia.In a study of 364 Taiwanese children with leukemia only 1 (0.3%) developed intussusception[6].In a study from the United Kingdom no intussusception was found in 800 children[7].
Combining the data from the retrospective reviews and case reports (Table 1) there were 74 patients with intussusception and a hematologic malignancy for review[8-22].The majority of patients were male (80.3%).The average age (8.0 ± 3.8 years) and median age (7.5 years) were higher than the typical age (< 2 years) of children with intussusception.Only two children were less than two years of age.The type of cancer was more commonly lymphoma (85.3%) than leukemia (14.3%), however, the data may be skewed as two large retrospective studies were done to assess for intussusception in children with lymphoma[3,4].
Intussusception as the initial presentation of hematologic cancer occurred in 47.6%of the patients (Table 2).Intussusception was seen as a complication of known cancer in the remaining patients; occurring more commonly during maintenance (19.0%) or at relapse of disease (19.0%), then during induction (14.3%).Where documented, most patients (89.7%) had an identifiable lead point; the most common lead point was the cancer (80.8%), followed by mucosal necrosis (7.7%), typhlitis (3.8%), hematoma(3.8%), and lymph node (3.8%).The majority of intussusceptions were ileo-colic(86.7%), followed by ileo-ileal (9.3%), ileo-ileo-colic (2.7%) and colo-colic (1.3%).Intussusception was acute in 60% of children and chronic in 40%.
All of the reported patients presented with abdominal pain and various combinations of abdominal distension, vomiting, and hematochezia (Table 1).The patient described herein was asymptomatic regarding GI complaints.He underwent colonoscopy as part of the evaluation for anemia and was found to have a large mass filling the colon lumen; biopsy of the mass showed recurrent lymphoma.
A number of children had a contrast enema performed in an attempt to reduce intussusception, the majority (85.7%) were not successful resulting in the need for surgery (Table 2).Overall, surgical intervention occurred in the vast majority (95.7%)of the children.A tissue diagnosis was most often obtained by surgical biopsy (77.8%);diagnosis was made by colonoscopic biopsies on 2 occasions (11.1%), by PET scan(5.6%) and at autopsy (5.6%) once each.
CONCLUSION
We report a young man with ALL relapse presenting with asymptomatic intussusception with the diagnosis being made with colonoscopic biopsies.This case should serve as a cautionary tale that serious complications resulting from ALL may occur despite minimal clinical symptoms.

Table 1 Characteristics of patients presenting with intussusception due to hematological malignancy
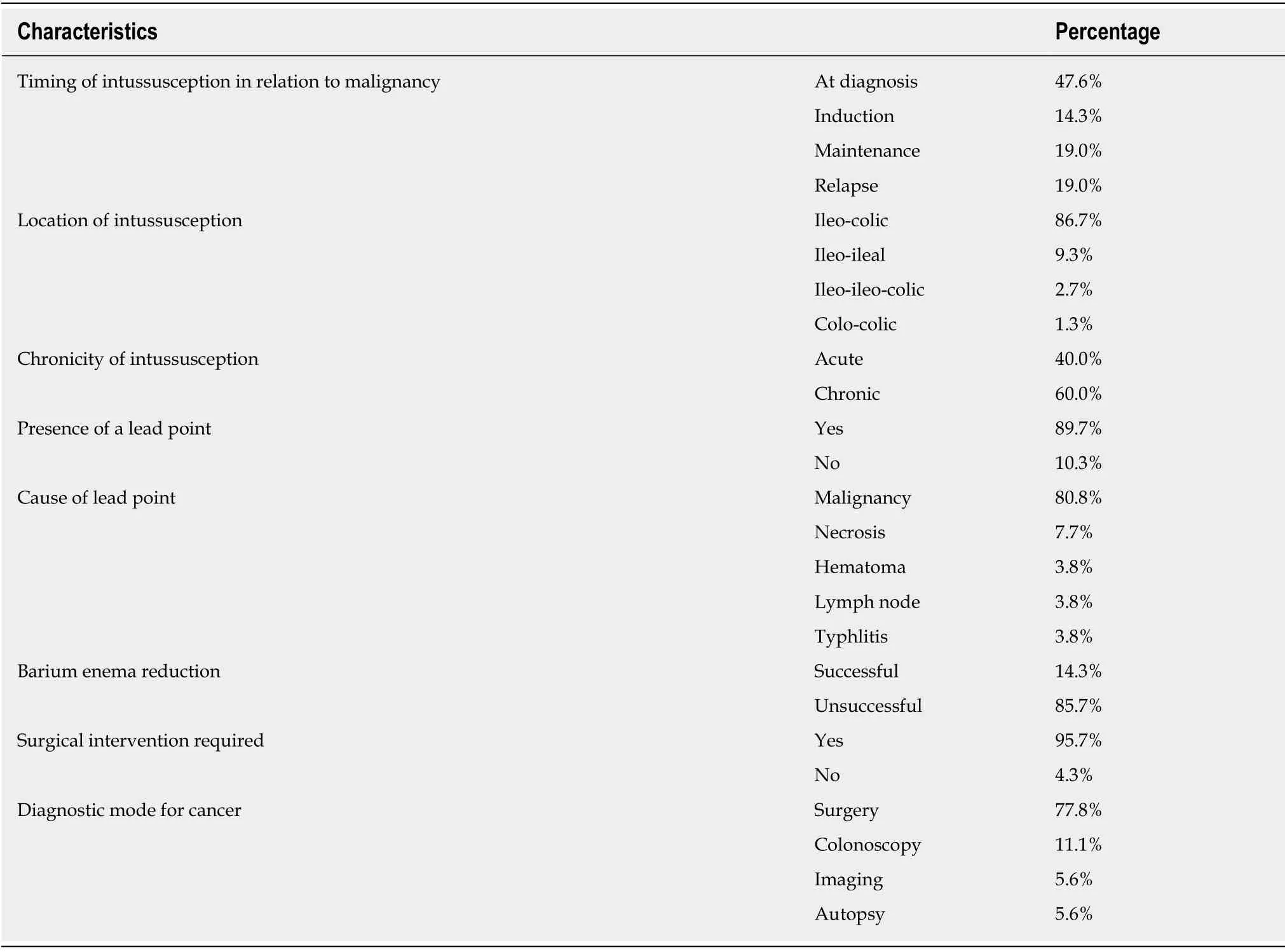
Table 2 Characteristics of the intussusceptions

Figure 2 Abdominal and pelvic computed tomography scan.
杂志排行
World Journal of Clinical Cases的其它文章
- Awareness during emergence from anesthesia:Features and future research directions
- Risk factors for adverse cardiac events in adults with fulminant myocarditis during hospitalization
- Malignant tumors associated with Peutz-Jeghers syndrome:Five cases from a single surgical unit
- Pathogens causing diarrhoea among Bangladeshi children with malignancy:Results from two pilot studies
- One-year rotational relapse frequency following conventional circumferential supracrestal fiberotomy
- LINX® reflux management system to bridge the “treatment gap” in gastroesophageal reflux disease:A systematic review of 35 studies