透明细胞肾细胞癌(CCRCC)合并多发性乳头状瘤(PA)1例
2019-10-09胡小木周仲文
胡小木 周仲文 倪 响 唐 峰
(1 复旦大学附属华山医院病理科 上海 200040; 2复旦大学附属中山医院病理科 上海 200032)
Papillary adenoma (PA) is a kind of unencapsulated tumors with tubupapillary architecture of low WHO/International Society of Urological Pathology (ISUP) grade and a diameter less than 15 mm[1].These tumors all shows no clinical symptoms and are usually discovered incidentally.PAs have no capsule but the borderline between them and renal cortex is usually clear.Morphologically,these tumors are often composed of cells with pale and scanty cytoplasm and round to oval nuclei.Cytogenetic studies have shown that it has frequent gains of chromosomes 7 and 17 and loss of the Y chromosome[2].
Clear cell renal cell carcinoma (CCRCC) is the most common malignant neoplasm occurring in kidney.The diagnosis can be easily made by combining the macroscopic image of multi-colored mass and histological presentation of clear cells together with abound vessels crossing them.Renal PA coexists with CCRCC is extremely rare which,to our knowledge,has only been reported in one literature,in which 6 cases was presented[3].While multiple PAs with CCRCC has never been reported.Since the accident discovery of PAs in our case,we believe that there could be more cases which were ignored by surgeons and pathologists.
Case presentationA 60 year-old man was referred to our hospital after suffering from lumbago without hematuria,dysuria or increase in urination frequency for two months.There was no family history of renal neoplasms or other family syndrome.The patient has a history of appendectomy and endoscopic excision of polyp located in stomach.From the image results of the patient’s local hospital,both type-B ultrasonic inspection and computed tomography (CT) only revealed a mass measuring 5.2 cm in diameter in left kidney.The further evaluation of CT angiography (CTA) demonstrated marked vascularity.After that,a nephrectomy was performed and the specimen was sent to pathology department.
Histopathology,immunohistochemistry and fluorescence in situ hybridizationThe specimen has been fixed in 10% buffered formalin and routinely processed to paraffin wax.Immunohistochemistry was performed on 3mm sections cut from paraffin blocks using antibodies:cytokeratin (CK;AE1/AE3),CK7 (OV-TL),vimentin (V9),CD117 (Dako);CD10 (56C6,Shenda Biotechnologies);epithelial membrane antigen (EMA),WT-1 (WT49),CK5/6 (D5/16B4)(MXB Biotechnologies);P53 (DO-7;Long Island Antibody).
FISH studies were conducted on 4 mm sections with probe 3,7,17 (Gpmedical,China) in a humidified chamber.
Medical examination resultsIn thepathologic examination of first time,we found the kidney measured 14 cm×9 cm×5 cm,and in the cortex of lateral border of kidney located 4 cm×3.5 cm×3 cm,well circumscribed mass with yellow-brownish necrotic areas.On top of this,in the location 1.3 cm far to the mass,a well-defined brown nodule was discovered in the cortex.Microscopically,the bigger tumor demonstrated a classic image of clear cell RCC and was immunoreactive for CK,Vimentin,CD10 and showed negative for CD117,CK7.The smaller nodule is characterized by papillary structures lined with round to oval nuclei,among which,several foam cells can be observed.The lesion stained positive for CK,CK7,vimentin,EMA,and negative for WT-1,CD10,P53 or CK5/6.Given the diameter of 1 cm in maximum,the diagnosis of PA was firstly proposed.After that,the resected kidney was reviewed and carefully checked again,by which we found another 3 tiny nodules measuring 1-3 mm in diameter.All these tiny nodules were proved to be PA by pathological images,which in turn supported the initial diagnosis.Finally,fluorescence in situ hybridization was performed and the tumor showed no amplification or deletion in chromosomes 3,7 and 17 (Fig 1).
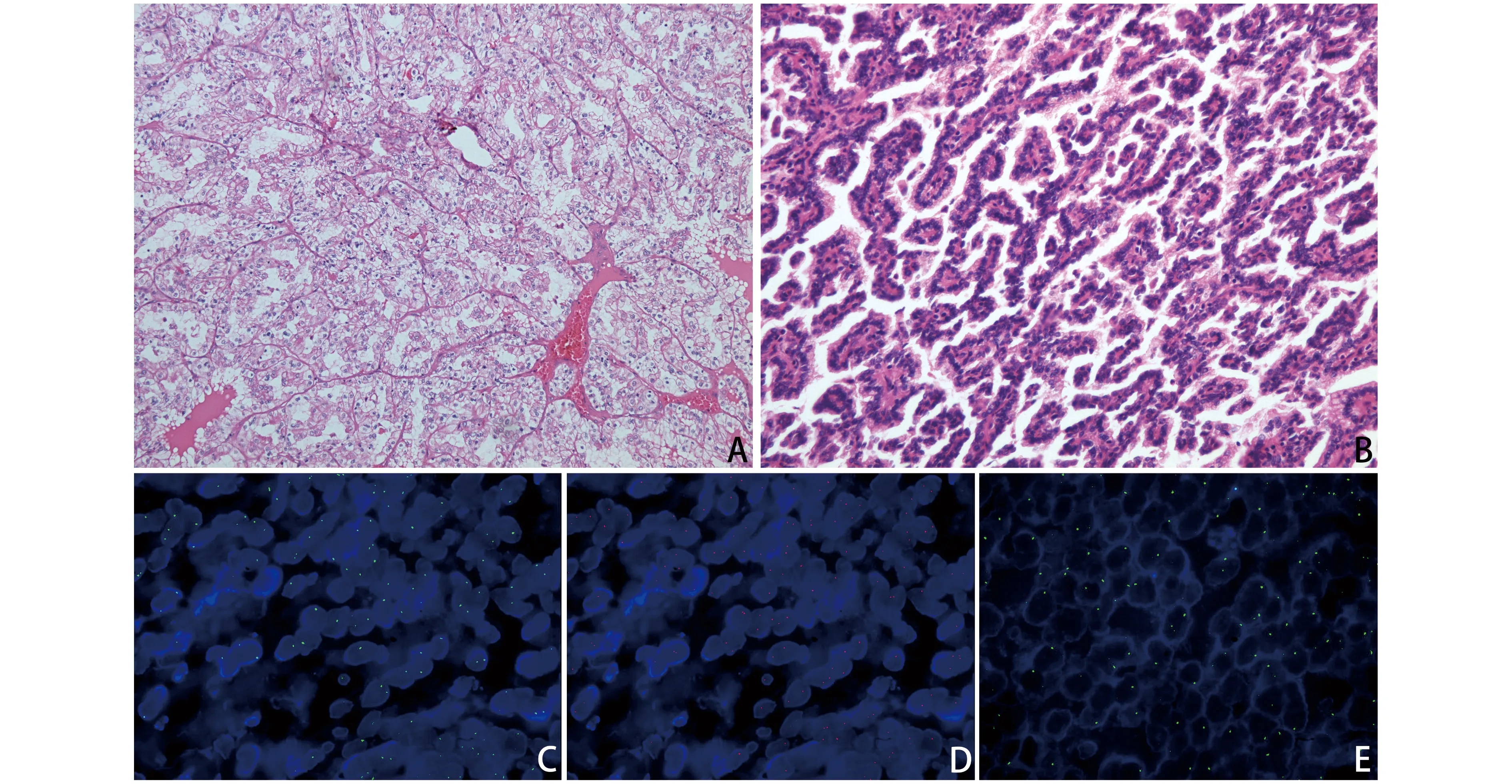
A:CCRCC (×200);B:One of the PAs (×200).The PA showed no amplification or deletion in chromosomes 3(C),7(D) and 17(E).
Fig 1 HE-staining sections of CCRCC and PA
DiscussionCCRCCs are solitary cortical tumors that accounts for the most part of malignant tumors in kidney,as a result,it is often easily noticed and diagnosed.However,according to the new WHO classification of renal tumors,there still some tumors such as Xp11 translocation renal cell neoplasms and clear cell papillary carcinoma need to be excluded before making the final diagnosis.Some immunohistochemistry markers such as TFE3,TFEB and molecular analysis will do help to identify the Xp11 translocation renal cell neoplasms[4].To exclude the clear cell papillary renal cell carcinoma,features including labeling for CD10 and AMACR,higher nuclear grade and tumor stage,tumor necrosis and abnormalities of chromosome 3p by FISH may be significant[5].Many nephrectomies were performed for the discovery of CCRCC and this is why most urologists and pathologists put too much enhance on this tumor to find other tiny lesions in the specimen,which could have been happen in our case but for the twice careful examination.
Making an accurate diagnosis of renalPA can be challenging because not only the imaging doctors and urologists,but also the pathologists in charge of dissection can easily overlook this kind of tumor.On top of this,the PA need to be distinguished from metanephric adenoma and papillary renal cell carcinoma.Metanephric adenomas are usually well circumscribed and demonstrate a similar image to PA in HE staining sections,immunohistochemistry can do much help for differential diagnosis because the former stains positively to WT-1 and negative to EMA.Another useful key to differential diagnose is that multifocal metanephric adenoma is extremely rare.Papillary renal cell carcinoma often exhibits a mass with pseudocapsule and microscopically,papillae with foamy macrophages along with psammoma bodies can be often observed.This malignant tumor often show positive immunohistochemical reactions for high-molecular weight cytokeratin,vimentin and CD10.
Almost all of the PAs are incidental findings and so is our case.Before operation,none of medical examinations including CT revealed the existence of multiple PA.Even in our pathological examination,it was until the second time did we find other 3 tiny lesions in the cortex.The small size and silence of clinic may be the main reason of the ignorance,also accounting for the different data of PA incidence.PAs have been reported in resected kidney for various reasons from polycystic renal disease to transplantation for end-stage renal failure.PA in kidney with clear-cell RCC is only found in 6 patients in literature[3].Up to now,our case is the first report of multiple PAs coexisting with CCRCC.However,we believe that more cases can be found if all the cores are carefully checked.Identifying this tiny lesion is of much importance for that it is strongly associated with papillary renal cell carcinoma and probably be a precursor of the latter[3].On top of this,pathologists also should take responsibility to identify this lesion in donor kidney during judging whether a donor kidney is qualified[8].
Both of PA and papillary renal cell carcinoma shows frequent gains of chromosomes 7 and 17 and loss of the Y chromosome,also,statistical analysis showed no difference between adenomas and carcinomas.Gains of chromosomes 7,17,16,12,and 20 and loss of the Y chromosome occur early in the evolution of papillary renal cell neoplasia in tumors that are only a few millimeters in diameter.Progressive gains of these chromosomes do not appear to correlate with the transition from adenoma to carcinoma[6-7].In our presented case,the tumor showed no change in chromosomes 3,7 and 17,whether it is related to the CCRCC remains to be judged.
In conclusion,clear cell carcinoma coexisting with multifocal PA is extremely rare.We present this special case to raise both surgeons and pathologists’ awareness of recognizing the tiny lesion of kidney such as PA owning probability to grow into papillary carcinoma.To pathologists,it is of significance to put emphasis on the dissection,which is the first step and basis of accurate pathological diagnosis,while to surgeon,they should aware that a PA bearing donor kidney may not be qualified and the question whether a kidney with multifocal PA need to be totally resected need careful consideration and more discussion.
