Distribution and drug resistance of pathogenic bacteria in emergency patients
2019-04-18WeiHuaiQingBianMaJiaJiaZhengYangZhaoQiangRongZhai
Wei Huai,Qing-Bian Ma,Jia-Jia Zheng,Yang Zhao,Qiang-Rong Zhai
Wei Huai,Qing-Bian Ma,Qiang-Rong Zhai,Emergency Department,Third Clinical Medical College,Peking University,Beijing 100191,China
Jia-Jia Zheng,Yang Zhao,Laboratory Department,Third Clinical Medical College,Peking University,Beijing 100191,China
Abstract
Key words:Distribution;Drug resistance;Bacteria;Emergency department
INTRODUCTION
With the wide application of antibacterial drugs,the sensitivity of common bacteria to antibiotics is decreasing.Especially,the resistance to β-lactams,aminoglycosides,fluoroquinolones,and sulfonamides extremely plagues the effective anti-infective treatment and seriously threatens the lives of patients.At the same time,the emergence of new antibacterial drugs makes problem of drug abuse increasingly serious.It has become one of the most important medical problems worldwide.The recent discovery of superbacteria in India and other countries is a serious consequence of the abuse of antimicrobial drugs,but currently there is still no effective treatment that can replace the antibiotics to inhibit and exterminate the pathogens.Therefore,the rational use of antibiotics has become an important topic for clinical use[1].However,the premise of rational drug use is to understand the distribution of pathogens and the trends and characteristics of drug resistance.
Generally,patients in the emergency department have a relatively rapid disease progression.Without clear etiology and bacteriological basis,early and empirical use of antibiotics is required.In China,the emergency department of the central hospitals is an important department for the treatment and rescue of critically ill patients.It is difficult to avoid the body injury of patients caused by invasive treatment while rescuing patients,so it is also inevitable to be complicated with various hospital infectious diseases[2].Besides,most of the emergency departments are open management,with more patients’ family members,more hospital staff flow,and more severe ward environmental pollution,further increasing the probability of hospitalacquired infection in critically ill patients in the emergency department[3].For patients with severe infections,a combination of multiple antibiotics is often required,which may lead to bacterial resistance.Due to the great difference in the resistance of different pathogenic bacteria to antibacterial drugs,it brings great inconvenience to clinical medication,followed by poor therapeutic effect[4,5].In this study,we analyzed the distribution characteristics and drug resistance to different antibiotics of the bacteria isolated from the emergency department specimens in our hospital from 2013 to 2017.This study is of great significance for the selection of drugs for initialempirical treatment in the emergency department and the careful selection of antibiotics to reduce the generation of drug-resistant strains.
MATERIALS AND METHODS
Source of strain
This study was approved by the Ethics Committee of Peking University Third Hospital,China,and all patients provided written informed consent.
A total of 2048 critically ill patients hospitalized in the emergency department of Peking University Third Hospital from January 2013 to December 2017 were enrolled.The clinical examination specimens of these patients were collected,including deep sputum retained after adequate gargling(secretions from deep respiratory tract in patients with tracheotomy or intubation),urine,localized secretions,and blood from the apical segment of the catheter in patients with central venous catheterization1.Finally,the respiratory specimens accounted for 51.6% of all samples,blood specimens accounted for 23.3%,urine specimens accounted for 18.7%,sterile body fluid specimens accounted for 4.0 % and other specimens accounted for 2.4%.The bacteria were then isolated from these specimens.Only the first isolated strains were used for patients with replicate strains isolated.Staphylococcus aureusATCC25923,Enterococcus faecalisATCC29212,Escherichia coliATCC25922,andPseudomonas aeruginosaATCC27853 were used as control strains.
Methods
Bacterial identification and drug susceptibility testing were carried out according to the routine methods of the National Clinical Laboratory Procedures for bacteria culture,isolation,and identification.
The isolation media including China-blue plate and blood agar plate were purchased from Oxoid,United Kingdom.The bacterial identification was then performed using VITEK 2 Compact automatic microorganism analysis system(bioMerieux,France)and BD-Bruker MALDI Biotyper microorganism mass spectrometry rapid identification system(BD,United Kingdom).
Machine-based and paper-based susceptibility tests were used for evaluating drug sensitivity.Among them,the machine-based susceptibility test applied VITEK 2 Compact automatic microbiological analysis system to determine the minimum inhibitory concentration(MIC)of commonly used antibacterial drugs;the paperbased susceptibility test used Mueller Hinton Agar plates(Oxoid,United Kingdom).Cefoperazone-sulbactam,imipenem,tigecycline,amikacin,ciprofloxacin,and minocycline were purchased from Oxoid,United Kingdom.According to the Clinical and Laboratory Standards Institute(CLSI)M100-S27 document,2017 edition,the sensitivity of both tests was determined as sensitive(S),intermediate resistant(I),and resistant(R).The determination of susceptibility to cefoperazone-sulbactam referred to cefoperazone.The susceptibility to tigecycline ofEnterobacteriaceaeandAcinetobacterwas determined based on the United States Food and Drug Administration standard:S(MIC ≤ 2 μg/mL),I(MIC ≤ 4 μg/mL),and R(MIC ≥ 8 μg/mL).
Statistical analysis
Data were analyzed using the R 3.5.1 software.The rate was expressed as a percentage.The Cochran-Armitage trend test(CATT)was used to analyze the change trend of drug resistance rates with time.P <0.05 was considered to be statistically significant.
RESULTS
Bacterial distribution
A total of 3387 pathogens were isolated from various clinical specimens of 2048 critically ill patients,including 1805 strains of Gram-negative bacteria(53.29%),1141 Gram-positive bacteria(33.69%),and 441 fungi(13.02%).The Gram-negative bacteria were mainlyAcinetobacter baumannii(660 strains),Klebsiella pneumoniae(347 strains),Pseudomonas aeruginosa(338 strains),andEscherichia coli(237 strains).The Grampositive bacteria mainly includedStaphylococcus aureus(436 strains),Staphylococcus epidermidis(181 strains),Staphylococcus haemolyticus(161 strains),andEnterococcus faecalis(140 strains).Besides,the fungi were mainlyCandida albicans(207 strains),followed byCandida tropicalis(95 strains).As a result,the top six bacteria isolated from emergency patients wereAcinetobacter baumannii,Staphylococcus aureus,Klebsiella pneumoniae,Pseudomonas aeruginosa,Escherichia coli,andCandida albicans.
From 2013 to 2017,the isolation rates of common pathogens in the emergency department decreased,includingAcinetobacter baumannii(25.5% to 17.4%),Staphylococcus aureus(21.0% to 7.1%),Pseudomonas aeruginosa(12.3% to 10.3%),andEscherichia coli(7.6% to 6.5%).However,the isolation rate ofKlebsiella pneumoniaeincreased from 7.1% to 12.1%(Figure 1).
Drug resistance of Gram-negative bacteria
Although the isolation rate ofAcinetobacter baumanniihas been decreasing these year,it was still ranked first for many years and was a widely-resistant strain,whose resistance rates to imipenem and ciprofloxacin were above 90%.The drug with the lowest resistance rate ofAcinetobacter baumanniito common clinical antibiotics was tigecycline,followed by minocycline,but the sensitivity to the two drugs has been also decreasing each year(P< 0.01).
The resistance rates ofPseudomonas aeruginosato cefoperazone/sulbactam and imipenem were higher,with the resistance to cefoperazone/sulbactam increasing year over year(P< 0.01).But its resistance rate to amikacin was below 10%.
Klebsiella pneumoniaehad higher resistance rates to imipenem,cefoperazone/sulbactam,amikacin,and ciprofloxacin,with the lowest resistance rate to tigecycline.The resistance rate to minocycline was also high but it decreased year over year(P< 0.01).
ForEscherichia coli,the resistance to ciprofloxacin was high,and the resistance rate to cefoperazone/sulbactam showed an upward trend year after year(P <0.01).Besides,the resistance rates to imipenem,amikacin,and tigecycline were low,with the resistance rate to tigecycline being zero for the last three years(Table 1).
Drug resistance of Gram-positive bacteria
Staphylococcus aureusis the top one of the Gram-positive bacteria isolated from clinical examination specimens of emergency department patients.As shown in Table 2,the resistance rates ofStaphylococcus aureusto levofloxacin,penicillin G,and tetracycline were high,but the resistance rates to penicillin G and tetracycline showed a downward trend(P <0.01).Moreover,the resistance rates to vancomycin and tigecycline were always zero.
Analysis of patients infected with Klebsiella pneumoniae
As mentioned above,the isolation rates of common pathogens decreased year after year exceptKlebsiella pneumoniae.We then further analyzed the clinical data of all patients infected withKlebsiella pneumoniae(Table 3).There were 347 patients withKlebsiella pneumoniaeinfection aged between 18 and 96 years,with an average age of 73.35 ± 14.60 years.Notably,we found that the percentage of patients with deep venous catheterization or retention catheterization was much higher than that of patients without both operations.
DISCUSSION
This study showed that the top six pathogens isolated from emergency patients in our hospital from 2013 to 2017 wereAcinetobacter baumannii,Staphylococcus aureus,Klebsiella pneumoniae,Pseudomonas aeruginosa,Escherichia coli,andCandida albicans,consistent with other reports in the emergency department of the top three hospitals in the same area.Besides,the detection rates of drug-resistant bacteria were high,showing the severe situation of antibiotic resistance.Therefore,these findings provided a good basis for the early delivery of empirical medication for critically ill patients.
With the emergence of antibacterial drugs,the rate of bacterial resistance remains high[6].In this study,we found thatStaphylococcus aureushad high resistance rates to levofloxacin,penicillin G,and tetracycline,but the resistance rates to vancomycin and tigecycline were always zero.Besides,five linezolid-insensitive strains ofStaphylococcus aureuswere discovered,consistent with the previous report[7].Therefore,vancomycin should be given priority in the clinical treatment of severe patients withStaphylococcus aureusinfection.However,in case of adverse reactions,such as hyperpyrexia and hypersensitivity after vancomycin administration,tigecycline may be selected and targeted drugs may be given after drug sensitivity testing[8,9].Husseinet alindicated that a high MRSA prevalence was found amongst healthcare workers(HCWs)in Kurdistan Region,Iraq.Twenty-two point five percent of HCWs wereStaphylococcus aureuscarriers compared with 18.7% of non-HCWs.61.0% of S.aureus strains isolated from HCWs were MRSA compared with 21.6%from non-HCWs.The mean working years of MRSA carriers was significantly higher than that of MRSA non-carriers.Basic infection control measures,a screeningprogramme,and treatment of MRSA-positive HCWs can help as an effective measure to control MRSA infections[10].In addition,it was shown that among 13 patients infected with vancomycin-resistantEnterococcus,most patients had lower limb wound infection[11].Therefore,for patients with lower limb infection of vancomycin-resistant enterococcus,strict observation and active treatment are required to prevent multiple infections.
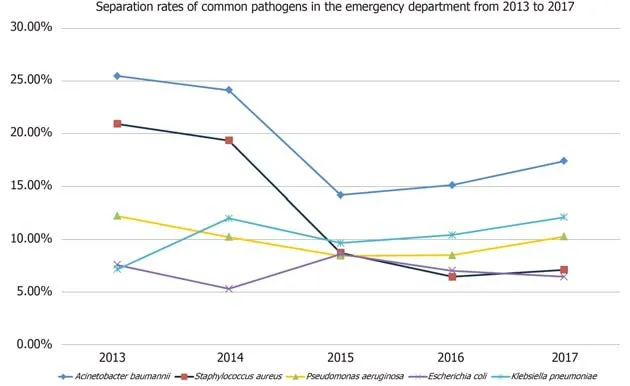
Figure 1 Separation rates of common pathogens in the emergency department from 2013 to 2017.
Acinetobacter baumanniiis a common colonized pathogen in hospital,and it is also a relatively common pathogen of nosocomial acquired pneumonia[12].In this study,its isolation rate ranked first for many years,and it was an extensively drug-resistant strain.Acinetobacter baumanniiin the emergency department is mostly due to nosocomial infection during hospitalization[13,14],and there are few reports thatAcinetobacter baumanniicauses community infection.
Klebsiella pneumoniaeranked second in the number of Gram-negative strains isolated in the emergency department.Recently,it has been reported that the drug resistance rate ofcarbapenems resistant enterobacteriaceae(CRE)shows a steady increasing trend,among whichKlebsiellabacteria account for the largest proportion[15].In this study,Klebsiella pneumoniaeshowed higher resistance to imipenem,cefoperazone/sulbactam,amikacin,and ciprofloxacin.The resistance ofKlebsiella pneumoniaeto carbapenem is mainly due to the production of carbapenemases,and few antibacterial drugs are available for the strains resistant to carbapenem,making clinical treatment difficult.A study in southern Europe showed a higher incidence of inappropriate empirical treatment for the multidrug-resistantKlebsiella pneumoniaebloodstream infection,resulting in a more than two-fold increase in patient mortality[16].However,it has also been demonstrated that patients who received carbapenem monotherapy or combination therapy within the first five days after blood culture positive for β-lactamase-producingKlebsiella pneumoniaeinfection had a significantly lower mortality than those who received non-carbapenem antibiotics[17].Therefore,carbapenems are still recommended as the treatment of choice for patients with severe infections,and compound agents containing β-lactamase inhibitors can be considered for patients with mild to moderate infections.Besides,due to the increasing reports of carbapenem-resistantKlebsiella pneumoniaein recent years,high doses of carbapenem can be given for treatment[18],and tigecycline can also be selected,owing to its goodin vitroantibacterial activity[19].
The positive rate of β-lactamase-producingEscherichia colifrom emergency sources should be low,but our study revealed thatEscherichia colihad high resistance to ciprofloxacin and cefoperazone/sulbactam,indicating that its resistance to quinolones and cephalosporins is still very prominent.In addition,the resistance rate ofEscherichia colito imipenem was low,which was consistent with the previous study[20].
As mentioned above,Klebsiella pneumoniaehas been the only bacteria with the increasing detection rate among the most common bacteria at the emergency department for the past five years,and the resistance to antibiotics such as meropenem and imipenem was also gradually increasing.These findings were in agreement with previous study[21],bringing great difficulties for clinical anti-infectivetreatment.Therefore,we further analyzed the clinical data of all patients infected withKlebsiella pneumoniaeand found that the proportion of patients with deep venous catheterization or retention catheterization was much higher than that of patients without both operations,indicating that indwelling deep venous catheter or urinary catheter is an independent risk factor for bloodstream infection withKlebsiella pneumoniae[22].Long-term indwelling urethral catheter causes bloodstream infection likely due to the colonization ofKlebsiella pneumoniaein damaged urethral mucosa during intubation and its regular release into the blood[23].Whereas the central venous catheter provides a direct way for bacteria to invade into the bloodstream,inducing the catheter-related bloodstream infection.Further,because the catheter is left in the blood vessel,the pathogenic bacteria in the blood can easily attach the front end of the catheter to gradually form a biofilm that is difficult to remove,which becomes a secondary infection source and aggravates the severity of infection.Therefore,in patients with clinically diagnosed bloodstream infections,when anti-infective drug therapy fails,the possibility of catheter-associated bacteremia should be considered.The ureter or central venous catheter should be removed timely.Other reports show that the use of antibiotics,especially cephalosporins and quinolones,is a risk factor forKlebsiella pneumoniaebloodstream infection[23,24].Besides,the total amount and days of antibiotic use were also found to be significantly associated with the development ofKlebsiella pneumoniaeinfection[25].Hence,short-course antibiotics may be useful in reducing drug-resistant bacteria[26].
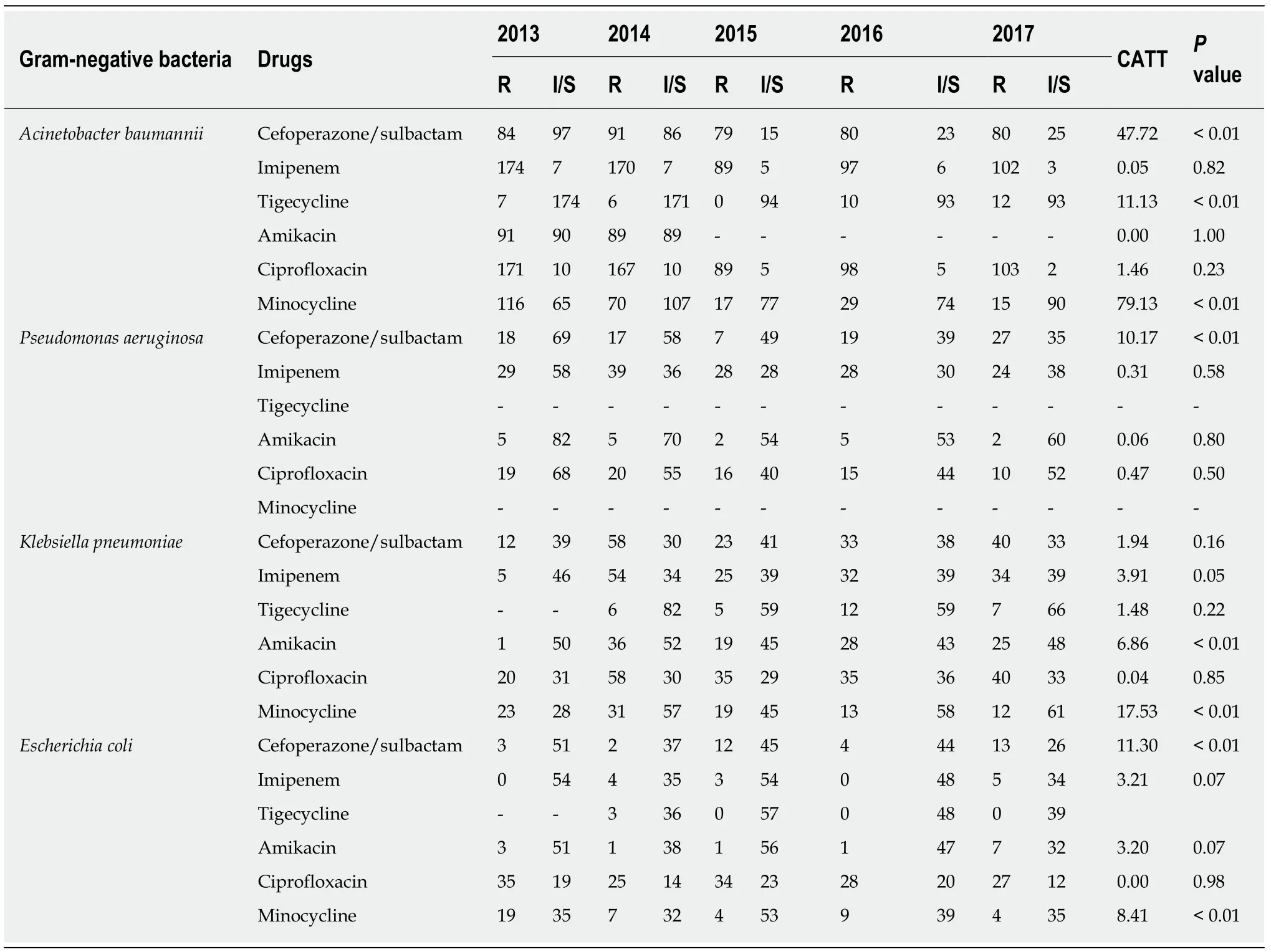
Table 1 Analysis of resistance rates of Gram-negative bacteria
There is a certain course of treatment with antibiotics,which should be administered on time once adopted to maintain sufficient concentration of drugs in patients to reduce the generation of drug-resistant strains[27,28].Some recent studies offer some hope for tackling bacterial resistance[29].Bacteriophages have many advantages over antibiotics in their use to treat and prevent infection by drugresistant bacteria.Their therapeutic effects are significantly different from those of antibiotics,making them still sensitive to multidrug-resistant bacteria[30].Therefore,phages are currently seen as a potential effective treatment for many multidrug-resistant bacteria[31].However,at the present stage,it is still of great significance to strengthen the pathogenic examination and monitoring in the emergency department and understand the distribution and drug resistance trends of the prevalent strains,so as to guide the rational use of drugs,reduce the production of multidrug-resistant bacteria,reduce the hospital infection rate and improve the success rate of patient treatment.
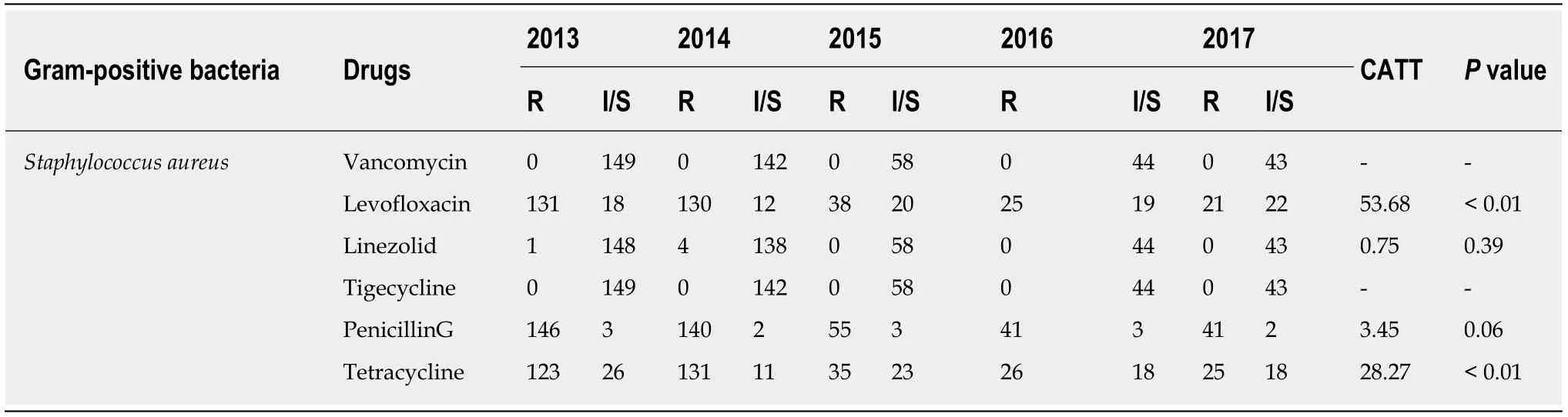
Table 2 Analysis of resistance rates of Gram-positive bacteria
In summary,the pathogenic bacteria isolated from the emergency department were mainlyAcinetobacter baumannii,Staphylococcus aureus,Klebsiella pneumoniae,Pseudomonas aeruginosa,Escherichia coli,andCandida albicans,with high detection rates of drug-resistant bacteria.When critically ill patients are admitted to the emergency department,initial antibiotic treatment should be selected empirically according to the distribution characteristics of bacteria in this area while bacteriological examination should be conducted on the clinical samples as soon as possible,and the later drug regimen should be adjusted timely according to the results of pathogen culture and drug sensitivity.For patients with extremely serious infections and life risk at any time,multi-drug regimens can be considered to achieve early control of the disease.
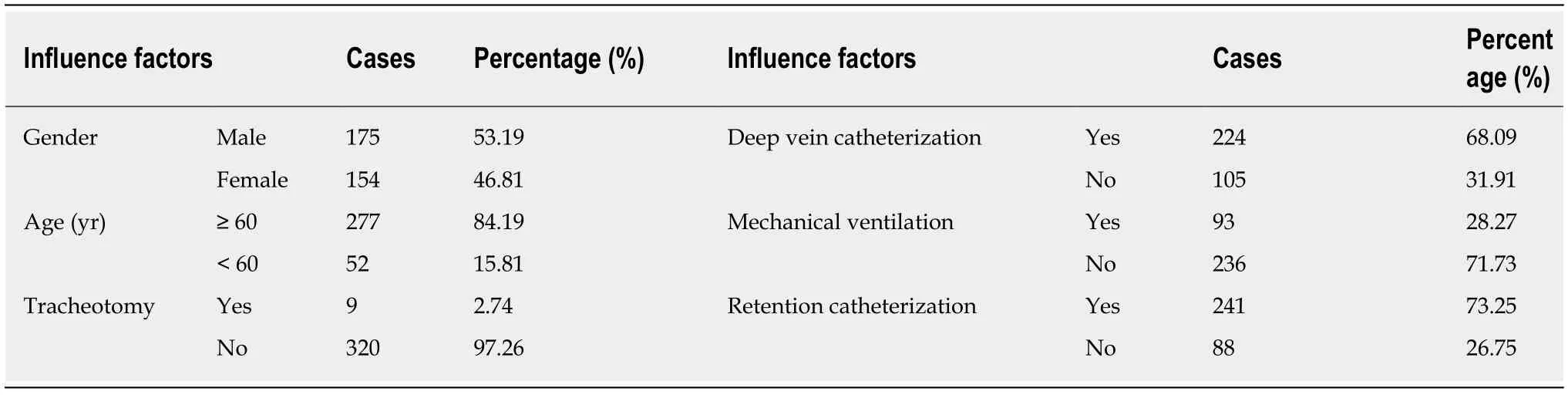
Table 3 Analysis of clinical data of patients with Klebsiella pneumoniae infection(n = 347)
ARTICLE HIGHLIGHTS
Research background
Antibiotic resistance has become a global threat for human health,calling for rational use of antibiotics.
Research motivation
The premise of rational drug use is to understand the distribution of pathogens and the trends and characteristics of drug resistance.
Research objectives
In this study,we analyzed the distribution characteristics and drug resistance to different antibiotics of the bacteria isolated from the emergency department specimens in our hospital from 2013 to 2017.This study is of great significance for the selection of drugs for initial empirical treatment in the emergency department and the careful selection of antibiotics to reduce the generation of drug-resistant strains.
Research methods
The isolation media including China-blue plate and blood agar plate were purchased from Oxoid,United Kingdom.The bacterial identification was then performed using VITEK 2 Compact automatic microorganism analysis system(bioMerieux,France)and BD-Bruker MALDI Biotyper microorganism mass spectrometry rapid identification system(BD,United Kingdom).Data were analyzed using the R 3.5.1 software.The rate was expressed as a percentage.The Cochran-Armitage trend test was used to analyze the change trend of drug resistance rates with time.P <0.05 was considered to be statistically significant.
Research results
The top six bacteria isolated from emergency patients wereAcinetobacter baumannii,Staphylococcus aureus,Klebsiella pneumoniae,Pseudomonas aeruginosa,Escherichia coli,andCandida albicans.From 2013 to 2017,the isolation rates of common pathogens in the emergency department decreased,includingAcinetobacter baumannii(25.5% to 17.4%),Staphylococcus aureus(21.0% to 7.1%),Pseudomonas aeruginosa(12.3% to 10.3.%),andEscherichia coli(7.6% to 6.5%).However,the isolation rate ofKlebsiella pneumoniaeincreased from 7.1% to 12.1%.The drug with the lowest resistance rate ofAcinetobacter baumanniito common clinical antibiotics was tigecycline,followed by minocycline,but the sensitivity to the two drugs has been also decreasing each year(P< 0.01).The resistance rates ofPseudomonas aeruginosato cefoperazone/sulbactam and imipenem were higher,with the resistance to cefoperazone/sulbactam increasing year over year(P< 0.01).But its resistance rate to amikacin was below 10%.Klebsiella pneumoniaehad higher resistance rates to imipenem,cefoperazone/sulbactam,amikacin,and ciprofloxacin,with the lowest resistance rate to tigecycline.The resistance rate to minocycline was also high but it decreased year over year(P<0.01).ForEscherichia coli,the resistance to ciprofloxacin was high,and the resistance rate to cefoperazone/sulbactam showed an upward trend year after year(P <0.01).the resistance rates ofStaphylococcus aureusto levofloxacin,penicillin G,and tetracycline were high,but the resistance rates to penicillin G and tetracycline showed a downward trend(P <0.01).
Research conclusions
The pathogenic bacteria isolated from the emergency department were mainlyAcinetobacter baumannii,Staphylococcus aureus,Klebsiella pneumoniae,Pseudomonas aeruginosa,Escherichia coli,andCandida albicans,with high detection rates of drug-resistant bacteria.When critically ill patients are admitted to the emergency department,initial antibiotic treatment should be selected empirically according to the distribution characteristics of bacteria in this area while bacteriological examination should be conducted on the clinical samples as soon as possible,and the later drug regimen should be adjusted timely according to the results of pathogen culture and drug sensitivity.For patients with extremely serious infections and life risk at any time,multi-drug regimens can be considered to achieve early control of the disease.These findings provided a good basis for the early delivery of empirical medication for critically ill patients.There is a certain course of treatment with antibiotics,which should be administered on time once adopted to maintain sufficient concentration of drugs in patients to reduce the generation of drug-resistant strains.Some recent studies offer some hope for tackling bacterial resistance.Bacteriophages have many advantages over antibiotics in their use to treat and prevent infection by drug-resistant bacteria.Their therapeutic effects are significantly different from those of antibiotics,making them still sensitive to multidrug-resistant bacteria.A total of 2048 critically ill patients were enrolled.The clinical examination specimens of these patients were collected,including deep sputum retained after adequate gargling(secretions from deep respiratory tract in patients with tracheotomy or intubation),urine,localized secretions,and blood from the apical segment of the catheter in patients with central venous catheterization.As mentioned above,Klebsiella pneumoniaehas been the only bacteria with the increasing detection rate among the most common bacteria at the emergency department for the past five years,and the resistance to antibiotics such as meropenem and imipenem was also gradually increasing.The pathogenic bacteria isolated from the emergency department were mainlyAcinetobacter baumannii,Staphylococcus aureus,Klebsiella pneumoniae,Pseudomonas aeruginosa,Escherichia coli,andCandida albicans,with high detection rates of drug-resistant bacteria.Phages are currently seen as a potential effective treatment for many multidrug-resistant bacteria.However,at the present stage,it is still of great significance to strengthen the pathogenic examination and monitoring in the emergency department and understand the distribution and drug resistance trends of the prevalent strains,so as to guide the rational use of drugs,reduce the production of multidrug-resistant bacteria,reduce the hospital infection rate and improve the success rate of patient treatment.
Research perspectives
There may be bias in data collection of retrospective studies.The future research direction is the rational use of antibiotics.
杂志排行
World Journal of Clinical Cases的其它文章
- Clinical use of low-dose aspirin for elders and sensitive subjects
- Comparative analysis of robotic vs laparoscopic radical hysterectomy for cervical cancer
- Feasibility of laparoscopic isolated caudate lobe resection for rare hepatic mesenchymal neoplasms
- Soft tissue release combined with joint-sparing osteotomy for treatment of cavovarus foot deformity in older children:Analysis of 21 cases
- Clinical characteristics of sentinel polyps and their correlation with proximal colon cancer:A retrospective observational study
- Longitudinal observation of intraocular pressure variations with acute altitude changes
