Extra-corporeal membrane oxygenation in aortic surgery and dissection: A systematic review
2019-02-27MassimoCapocciaMarcMaybauer
Massimo Capoccia,Marc O Maybauer
Massimo Capoccia,Department of Aortic and Cardiac Surgery,Royal Brompton Hospital,Royal Brompton and Harefield NHS Foundation Trust,London SW3 6NP,United Kingdom
Marc O Maybauer,Department of Anaesthesia,Manchester Royal Infirmary,Manchester University NHS Foundation Trust,Manchester M13 9WL,United Kingdom
Marc O Maybauer,Department of Anaesthesiology and Intensive Care Medicine,Phillips University,Marburg 35037,Germany
Marc O Maybauer,Critical Care Research Group,The Prince Charles Hospital and The University of Queensland,Brisbane QLD 4032,Queensland,Australia
Marc O Maybauer,Advanced Critical Care and Transplant Institute,Integris Baptist Medical Centre,Oklahoma City,OK 73112,United States
Abstract
Key words: Aortic dissection;Aortic surgery;Extra-corporeal life support;Extracorporeal membrane oxygenation;Extracorporeal life support;Mechanical circulatory support
INTRODUCTION
Veno-arterial extracorporeal membrane oxygenation (VA-ECMO) has become an established and widely used technique to provide circulatory support for critically ill patients with refractory cardiogenic shock and cardiac arrest[1-3]although an increased left ventricular (LV) afterload may affect the intended beneficial effects[4].The impact of VA-ECMO on LV function can be explained in terms of pressure-volume (PV)loops and Starling curves[5]following simulations based on a previously developed model[6,7].VA-ECMO does not affect LV function directly.When LV afterload is maintained constant at a specific systemic pressure,the Starling curve generated before VA-ECMO support predicts the filling pressure related to any target stroke volume (SV) at that systemic pressure.The mechanism by which that specific pressure is achieved does not change the relationship between filling pressure and native LV SV.A maintained Starling relationship during VA-ECMO support may help predict ventricular distension and optimise the balance between LV unloading and systemic perfusion[5].Despite the outcome of the SHOCK II trial which remains against the use of the intra-aortic balloon pump (IABP) in cardiogenic shock[8-10],a combined use of VA-ECMO and IABP has shown reduced in-hospital mortality[11,12].In addition,the combination of VA-ECMO and the Impella device has been shown to be a useful method to offload the left ventricle[13,14].Quantitative evaluation based on a simulation approach has confirmed the beneficial effect of adding IABP or Impella during VAECMO support[15].
A recent retrospective multi-centre cohort study on post-cardiotomy VA-ECMO has identified age,previous cardiac surgery,preoperative acute neurological events,aortic arch surgery and increased arterial lactate as factors associated with increased risk of early mortality following the procedure although the experience of the centre may contribute to improved results[16].Nevertheless,there is no real focus on critical patients experiencing post-cardiotomy failure after major aortic surgery for aneurysmal disease or dissection.
《修订稿》要求固定资产按类、按月计提折旧,高校实行固定资产折旧制度以后,每年资产的列支数为折旧金额,将来就是一项刚性支出,而新增资产不再全额列支。这必将对高校的收支、年底的决算平衡产生直接的影响,至于影响程度的大小,需要高校在计算出每年应计的折旧额后,再做评估。哪些固定资产应提折旧、应如何提取折旧、应提多少折旧等固定资产的信息要求,必将对原有的高校固定资产管理信息系统产生直接影响,对财务和资产管理人员提出了更高的要求。
Diseases of the thoracic aorta carry a high mortality with an increasing prevalence worldwide at present in the context of long-standing controversy regarding its treatment[17-19].Current evidence suggests that acute aortic syndromes are best treated in dedicated,high-volume aortic centres[20].Preoperative malperfusion plays a major role on early and late outcome[21-23].
Therefore,we sought to review current attitude on the use of mechanical circulatory support (MCS) following major aortic surgery with a view that it may be an option for these critical patients.The analysis has considered adult patients only.
MATERIALS AND METHODS
This review has been undertaken according to a web-based literature search on PubMed and EMBASE using appropriately combined key words [extra-corporeal life support (ECLS) and aortic surgery;ECLS and aortic dissection;ECMO and aortic surgery;ECMO and aortic dissection].The Participants,Intervention,Comparison,Outcome and Study Design (PICOS) approach for the selection of clinical studies following our systematic search has been used (Table 1).The PRISMA approach has also been considered whose main purpose is to help ensure the clarity and transparency of systematic reviews;it was developed using an evidence-based approach and is not intended as a quality assessment tool[24].An extension of the PRISMA statement has been developed to specifically address the reporting of systematic reviews incorporating network meta-analyses[25].PRISMA-P is intended to help the preparation and reporting of a robust protocol for a systematic review[26].
We selected all the articles including major aortic surgery involving the ascending aorta,arch,descending thoracic and abdominal aorta.
The aim of this systematic review was to determine current knowledge and experience with ECLS/ECMO support for aortic disease and whether it is appropriate for postcardiotomy failure following major aortic surgery with particular reference to aortic dissection.
RESULTS
The search gave the following results (Figure 1): ECMO and aortic surgery retrieved 906 publications in PubMed and 13 publications in EMBASE;ECMO and aortic dissection retrieved 61 publications in PubMed and 49 in EMBASE;ECLS and aortic surgery retrieved 67 publications in PubMed and no publications in EMBASE;ECLS and aortic dissection retrieved 5 publications in PubMed and 2 publications in EMBASE.The overall analysis revealed 29 publications related to the subject of investigation as follows (Table 2): 1 brief communication[27],1 surgical technique report[28],1 invited commentary[29],1 retrospective case review[30],1 observational study[31],4 retrospective studies[32-35],13 case reports[36-48]and 7 conference abstracts[49-55].The articles had been published between 1994 and 2019.Four publications reported key data for this review[31-34].A total number of 194 patients had been treated with ECMO support leading to 77 surviving patients.Three publications[31,35,54]did not specify how many patients survived following ECMO support;therefore,the number of surviving patients remains incomplete.Further analysis gives a breakdown of aetiology,procedures performed and cannulation site when available (Table 3).
DISCUSSION
ECMO has become increasingly available for the treatment of a diverse population of critically ill patients and recent reviews have highlighted its indications and the evidence basis to justify its use[1,56].VA-ECMO is a suitable approach in the context of cardiac failure.Veno-venous (VV) ECMO is appropriate in the context of acute respiratory disease syndrome.More recently,ECMO has been considered in the setting of extracorporeal cardiopulmonary resuscitation.Despite increased application of the technique,overall survival rates have remained unchanged with a 50%-70% range for respiratory support and 40%-60% range for cardiac support[57,58].Traditional configurations for ECMO support include the VV through the right internal jugular vein (Avalon cannula) and the veno-arterial (VA) either through the ascending aorta and the right atrium (central cannulation) or through the femoral vessels (peripheral cannulation)[3,59].Hybrid ECMO configurations have been increasingly considered recently as an attempt to improve outcome.Triple cannulation such as veno-venous-arterial (VVA) or venous-arterial-venous (VAV)configurations may help with concomitant cardiac and respiratory failure.VVA ECMO consists of double venous cannulation through the right internal jugular vein and the right femoral vein for drainage with right femoral artery cannulation for perfusion.VAV ECMO consists of single venous drainage through the right femoral vein with right femoral artery and right internal jugular vein for perfusion.The VPa configuration through the insertion of a long venous cannula in the pulmonary artery,usually via the right internal jugular vein,may be a suitable option for patients with right heart failure[3].
Our literature search revealed a limited number of relevant articles as expected.ECMO support following major aortic surgery has not been usually recommendedbecause of its potential to further exacerbate lesions of the aortic wall and increased bleeding with delayed thrombosis of the false lumen due to the use of anticoagulation[60-62].Nevertheless,3 retrospective studies[32-34]and 1 observational study[31](Table 2) have shown the feasibility of ECMO support in patients undergoing major aortic surgery for aneurysmal disease and dissection in contrast to current scepticism[29].In many countries the argument is to make for a balance between the costs involved in running ECMO support and select those patients who would benefit the most from a period of circulatory support following repair for acute aortic dissection.Monitoring the outcome of those patients who required ECMO support postoperatively and develop a specific database may be the way forward to shed further lights on the role of ECMO support in patients undergoing major aortic surgery.Although 1 retrospective study[34]has reported 88% mortality rate in 35 patients who underwent ECMO support following surgical treatment for type A aortic dissection,there is no mention about indications for ECMO support;profile and co-morbidities of these patients;cannulation site (peripheral or central);cause of death.Twenty-seven patients received ECMO support on the day of surgery and 8 patients required ECMO support on postoperative day 1 or later.Most unusual,4 additional patients with type A aortic dissection underwent ECMO support without surgical intervention but none of them survived.The other two retrospective studies[32,33]are more detailed with more favourable outcome in line with the extra corporeal life support organization registry[57,58].One study[33]included 36 patients who required VA-ECMO for post-cardiotomy failure following major aortic surgery.In-hospital mortality was 50% with multi-organ failure being the main cause of death.Preoperative levels of CK-MB >100 IU/L and peak lactate levels >20 mmol/L were considered relevant factors for in-hospital mortality.Retrograde flow cannulation was identified as another key factor for reduced survival compared to antegrade cannulation although the risk for early mortality is related to the preoperative clinical and haemodynamic status rather than the cannulation technique[62].The other study[32]compared short- and long-term outcomes between patients who required ECMO support and those who did not.In-hospital mortality was higher in the ECMO group(65%) compared to the non-ECMO group (8.5%).Preoperative haemodynamic instability,aortic cross-clamp time and postoperative peak CK-MB were identified as predicting factors for postoperative ECMO support.ECMO survivors had younger age and less postoperative blood transfusion.Interestingly,those patients who survived after ECMO support following repair for acute type A aortic dissection showed a long-term survival rate comparable to patients who did not require ECMO support postoperatively.These findings were confirmed by a very detailed observational study[31]comparing patients with and without LV systolic dysfunction who underwent surgical intervention for acute type A aortic dissection.A total of 510 patients were considered: 86 with LV systolic dysfunction (group I) and 424 patients with preserved LV systolic function (group II).ECMO support was required in 7 patients from group I and in 10 patients from group II.The overall mortality was 79 patients out of 510: 20 from group I and 59 from group II.Multivariate analysis confirmed that a preoperative serum creatinine greater than 1.5 mg/dL and the requirement for ECMO support intra-operatively were significant independent predictors of in-hospital mortality but survival following ECMO support was not specified.Although patients with preoperative LV systolic dysfunction showed higher surgical risk for in-hospital mortality,their 3-year cumulative survival rate(77.8%) was comparable with those with preserved LV systolic function (82.1%).Serial echocardiographic assessment did not show further deterioration of LV systolic function during the 3-year follow-up.
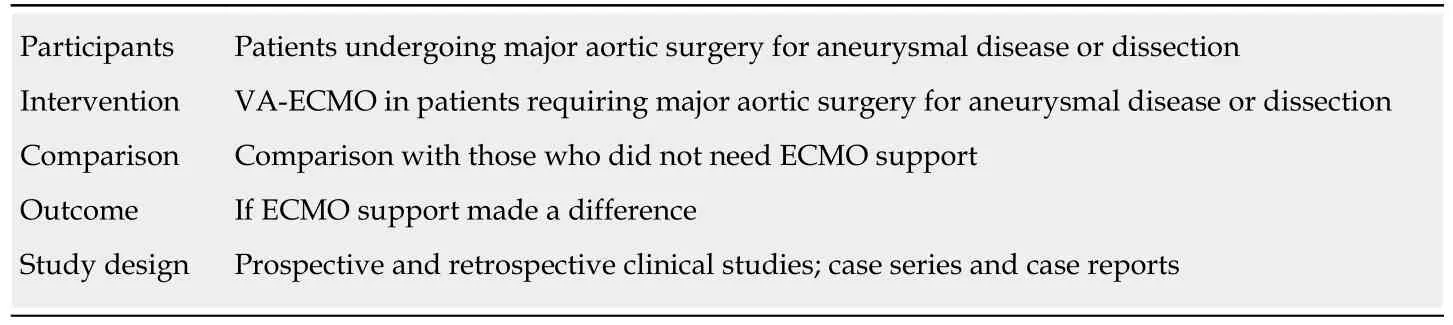
Table1 “Participants,Intervention,Comparison,Outcome and Study Design” approach for the selection of clinical studies following systematic search

Figure1 Summary of the steps followed during the literature search.
Factors predicting the need for postoperative ECMO support[31,32,34]: Preoperative haemodynamic instability;Myocardial infarction;Aortic cross-clamp time;Cardiopulmonary bypass time;Biventricular systolic dysfunction;Inadequate myocardial protection;Postoperative peak CK-MB;Propagation of the dissection into the coronary arteries.
Factors related with survival following ECMO support[32,33]: Younger age;Reduced postoperative blood transfusion;Lower level of preoperative CK-MB;Higher rate of antegrade cannulation;Lower lactate levels at 12 h;Lower rate of continuous renal replacement therapy;Longer intensive care stay.
Factors related with adverse outcome[31,33]: Retrograde flow cannulation;Peak lactate levels >20 mmol/L;Preoperative CK-MB >100 IU/L;Combined aortic arch replacement;Postoperative need of continuous renal replacement therapy;Prolonged inotropic support;Visceral ischaemia;Limb ischaemia.
In conclusion,although there is no compelling evidence in favour or against the use of ECMO support following major aortic surgery for aneurysmal disease or acute aortic dissection,it is enough to justify its use in those patients who develop haemodynamic instability refractory to inotropic support.

Table2 Grading of manuscripts with key information and outcome

?
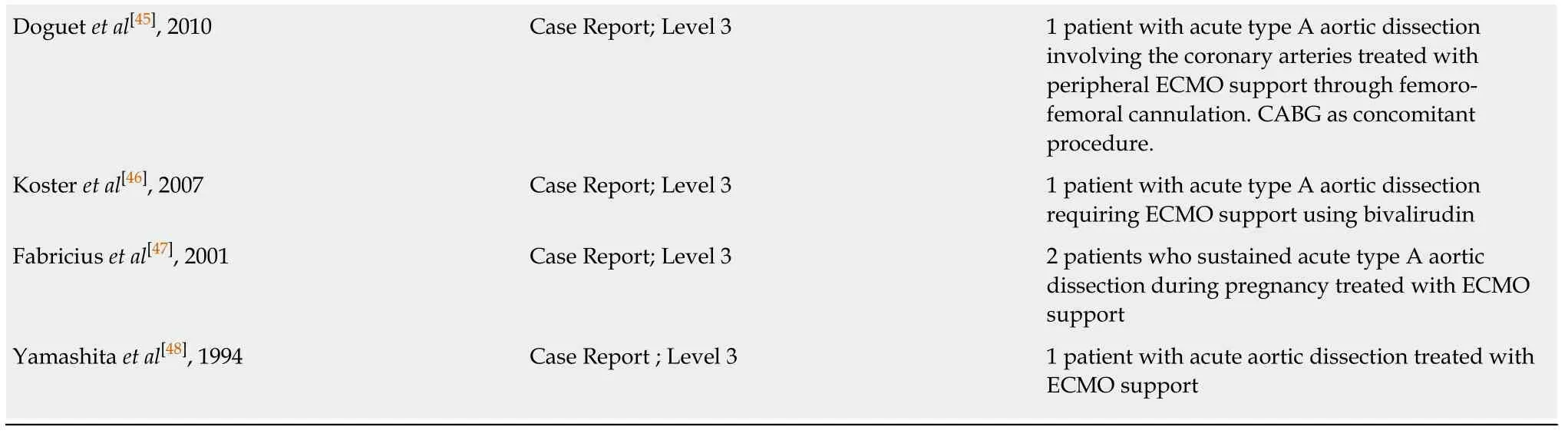
ATAAD: Acute type A aortic dissection;ECMO: Extra-corporeal membrane oxygenation;TEVAR: Thoracic endo-vascular aortic repair;AAA: Abdominal aortic aneurysm;EVAR: Endo-vascular aortic repair.
ARTICLE HIGHLIGHTS
Research background
Extra-corporeal membrane oxygenation (ECMO) support following major aortic surgery with particular reference to aortic dissection remains controversial without clear direction.We aim to shed some lights on the subject in order to make an impact and give a clear view that may well lead to further studies.
Research motivation
We believe that a clear direction based on evidence may change current attitude.
Research objectives
Although ECMO support is not perfect,it does work when appropriately considered and performed.We believe it may become an additional option in aortic surgery.
Research methods
The methods have been already described in the article.
Research results
The results are promising and may lead to further studies to improve outcomes.
Research conclusions
There is enough evidence to support our statement although we would like to think that further studies can be pursued to confirm our initial findings.
Research perspectives
There is potential to support further studies in the future.
