Observation on mind-refreshing and orifice-opening needling method plus swallowing disorder therapeutic apparatus for deglutition disorder of stroke patients in the convalescent stage
2018-06-28XuZhenjie徐贞杰XiangLian向连LiuXia刘霞
Xu Zhen-jie (徐贞杰), Xiang Lian (向连), Liu Xia (刘霞)
Rehabilitation Department, Bai’an Branch of Chongqing Three Gorges Central Hospital, Chongqing 404100, China
Stroke is the most common cause of deglutition disorder. In China diagnostic and treatment guidelines for acute ischemic stroke, it occurs to nearly 50% of stroke patients on admission[1]. It’s also one of the risk factors for respiratory aspiration and a serious complication which happens in nearly 43%-54% of stroke patients[2]. Aspiration can lead to aspiration pneumonia or even life-threatening apnea, and thus cause grave impact on stroke patients’ quality of life(QOL) and safety. We have used mind- refreshing and orifice-opening needling method plus swallowing disorder therapeutic apparatus to treat deglutition disorder of stroke patients, and the report is now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
Conforming to the diagnostic criteria of stroke formulated in the Fourth National Academic Conference on Vascular Disease[3], and certified by cranial CT or MRI examinations; with the symptoms of deglutition disorder including choking, prolonged catering and drinking time, difficulty chewing and muscular atrophy,retarded or disappeared pharyngeal reflex.
1.2 Inclusion criteria
Conforming to the diagnosis criteria above; clear consciousness, without mental retardation, capable of understanding and following simple instructions of researchers; stable vital signs, without fever or pulmonary infection; grade 2 or higher grade evaluated by water-swallowing test (WST); aged between 20-65 years; signed an informed consent form.
1.3 Exclusion criteria
Stroke patients with severe visceral failure or in critical condition; other reasons led to deglutition disorder.
1.4 Statistical method
All data were analyzed with SPSS version 17.0 software. Enumeration data were compared using Chi-square test. Measurement data conforming to normal distributionxwere expressed with mean ±standard deviation (±s), and compared usingt-test;non-parametric test was used for data not conforming to normal distribution. APlevel less than 0.05 indicated a statistical significance.
1.5 General data
A total of 136 patients who met the inclusion criteria were included in this study. They were randomized by the random number table into three groups, including group A (treated with swallowing disorder therapeutic apparatus), group B (treated with mind-refreshing and orifice-opening needling method) and group C (treated with mind-refreshing and orifice-opening needling method plus swallowing disorder therapeutic apparatus). The differences in gender, age, duration and types of stroke showed no statistical significance (allP>0.05), indicating that the three groups were comparable (Table 1).

Table 1. Baseline comparison of the three groups
2 Treatment Methods
Patients in all three groups received same routine medicine treatment and rehabilitation training.Symptomatic medicine treatment was chosen according to patients’ condition, including neurotrophic drugs,anti- platelet agent and medicine to regulate blood pressure, lipid and glucose, and also cold stimulation therapy, breath-holding and pronouncing training,throat elevating exercise, physical and occupational therapy.
2.1 Group A
Patients in group A received the treatment of swallowing disorder therapeutic apparatus (YS1001,Changzhou Siya Medical Apparatus Instrument Co., Ltd.,China) combining conventional methods. After sterilization of skin around the neck, 2 electrode plates named channel 1 and channel 2 were pasted on patients’ laryngeal prominence on one side, and the location superior to laryngeal prominence on the other side separately. Then fixed the electrode plates with bandages, and increased the electric intensity to achieve the expected sensation or muscle movement.Every treatment lasted for 30 min. During treatment,instructed patients to do the swallow movement.
2.2 Group B
Patients in group B received mind-refreshing and orifice-opening needling plus routine treatments.
Acupoints: Shuigou (GV 26), bilateral Neiguan (PC 6),Sanyinjiao (SP 6), Fengchi (GB 20), Wangu (GB 12) and Yifeng (TE 17).
Methods:After routine sterilization, filiform needles of 0.35 mm in diameter and 50 mm in length were punctured perpendicularly at bilateral Neiguan (PC 6)for 0.5-1.0 cun. Upon qi arrival, performed twirling and lifting-thrusting reducing manipulations for 1 min. Then punctured Shuigou (GV 26) towards the direction of nasal septum for 0.3-0.5 cun, performed heavy pecking sparrow method until patients felt moist in eyes or shed tears. Punctured Sanyinjiao (SP 6) along the medial border of tibia for 1.0-1.5 cun, keeping a 45° angle between shaft of the needle and skin. Upon qi arrival,performed lifting-thrusting reinforcing manipulation until patients felt 3 twitching movements on lower limbs. When punctured Fengchi (GB 20), Wangu (GB 12)and Yifeng (TE 17), kept the needle tip toward laryngeal prominence and inserted 2.0-2.5 cun. Upon qi arrival,performed twirling reinforcing method of little amplitude and high frequency. Every manipulation was done for 1 min at each acupoint. The needles were retained for 30 min every time[4].
2.3 Group C
Patients in group C received conventional treatment combining swallowing disorder therapeutic apparatus and mind-refreshing and orifice-opening needling method which were the same as that in group A and group B.
Treatment above was done once a day, and 10 d constituted a course. The whole treatment lasted for 4 courses. There was a 1-day interval between every two courses.
3 Results
3.1 Observation items
Items below were measured before, after and follow-up visit period (2 months after treatment).
3.1.1 WST[5]
Deglutition capability is classified into 5 degrees. I:swallowing water in one time smoothly without bucking;II: swallowing water in two servings without bucking; III:swallowing water in one time with bucking; IV:swallowing water in two servings with bucking; V:frequent bucking, cannot finish drinking water.
Normal: for cases rated as grade I, those finish drinking in 5 s; suspicious: for cases rated as grade I,those finish drinking in more than 5 s and who was rated as grade II; abnormal: grade III, IV and V.
Scoring criteria: cases rated as grade I was scored as 5 points, grade II as 4 points, grade III as 3 points, grade IV as 2 points, grade V as 1 point. The minimum score was 1 point, the maximum score was 5 points. A higher score indicated a better deglutition capability.
3.1.2 Standardized swallowing assessment (SSA)[6]
The SSA evaluation is comprised of three sections.The first section is clinical examination, items including consciousness, head and trunk control, breathe, closure of lips, soft palate movement, larynx function,pharyngeal reflex and voluntary cough are measured,the total score ranges from 8 to 23 points. The second section is deglutition test. Patients are asked to swallow 5 mL water for three times, and the presence of larynx movement, repeated deglutition and wheezes, and larynx functions following deglutition are measured,and the total score ranges from 5 to 11 points. The third section is that the patients are asked to swallow 60 mL water in normal circumstance, then the time needed for deglutition and occurrences of cough are measured. The total score ranges from 5 to 12 points. Therefore, the minimum score of SSA is 18 points, and the maximum score is 46. A higher score indicates a worse deglutition function.
3.1.3 Activities of daily living (ADL)[7]
ADL was evaluated using modified Barthel index(MBI), including feeding, bathing, grooming, dressing,bowels, bladder, toilet use, transfers (bed to chair and back), mobility (on level surfaces) and stairs. Each item is classified into 5 grades with corresponding scores. The total score of MBI is 100 points. A higher score indicates a better ADL circumstance.
3.2 Clinical efficacy evaluation[8]
Cured: Flexible tongue motion, normal deglutition movement, grade I evaluated by WST.
Marked effect: Obvious improvement of deglutition disorder, grade II evaluated by WST.
Effective: Improvement of deglutition disorder, grade III evaluated by WST.
Invalid: No improvement of deglutition disorder,grade IV or V evaluated by WST.
3.3 Results
3.3.1 Clinical effect
After treatment and during follow-up visit period, the total effective rates in group A showed no statistical significance in comparing with those in group B (allP>0.05), the total effective rates in group C were superior than those in group A and group B (allP<0.05),(Table 2).
3.3.2 Comparisons of WST, SSA and MBI scores
Intra-group comparison: after treatment and during follow-up visit period, scores of the WST and MBI test increased significantly in comparing with those before treatment (allP<0.05); the SSA scores in all groups were lower than those before treatment (allP<0.05); during follow-up visit period, the changes of WST, SSA and MBI scores showed no statistical significance in comparing with those before treatment (allP<0.05). Inter-group comparison: after treatment and during follow-up visit period, the WST scores in group C were substantially higher than those in group A and group B (allP<0.05),while the differences showed no statistical significance between group A and group B (bothP>0.05); the SSA scores in group C were substantially lower than those in group A and group B (allP<0.05), while the differences showed no statistical significance between group A and group B (bothP>0.05); the MBI scores in group B and group C were substantially higher than those in group A(allP<0.05), while the differences showed no statistical significance between group B and group C (bothP>0.05),(Table 3-Table 5).
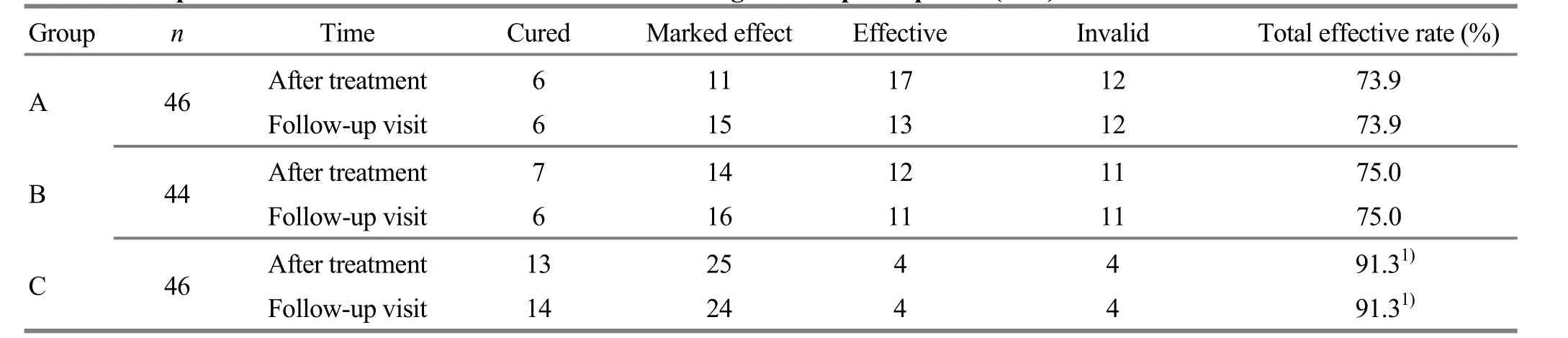
Table 2. Comparison of clinical effect after treatment and during follow-up visit period (case)

Table 3. Comparison of WST score (x±s, point)

Table 4. Comparison of SSA score (x±s, point)

Table 5. Comparison of MBI score (x±s, point)
4 Discussion
In traditional Chinese medicine, stroke occurs as a result of stagnant blood, liver wind or turbid phlegm misting the brain. Mind-refreshing and orifice-opening needling method was created by academician Shi Xue-min based on the mechanism of this disease. In this technique, acupoints on yin meridians and the Governor Vessel are mainly selected, and acupuncture manipulation and stimulation intensity are standardized.It is also an innovation based on traditional acupointsselection and manipulation. Liu T,et al[9]held that the functioning mechanism of mind-refreshing and orificeopening needling method might be explained as follows.The lower motor neuron in spinal cord layer is stimulated in the first place. Then, the active movement order is given to patients to stimulate central nerve system to send impulses. At that time, damaged upper motor neuron will send minor impulses and further induce sensitized cells in anterior horns of spinal cord to generate action potentials, realizing the recanalization of neural pathways. Many clinical researches proved that mind-refreshing and orifice-opening needling method would effectively reverse neural function damage, and improve hemodynamic items[9-12]. Our study showed that mind-refreshing and orifice-opening needling method would effectively improve deglutition functions and ADL in stroke patients.
Swallowing disorder therapeutic apparatus is a low frequency, electrical stimulation equipment rooted on neuron facilitation technology and remodeling theory[13].The mechanism may be summarized as follows. On one hand, it directly stimulates pharyngeal muscles and therefore increases local muscle contraction to improve the balance of deglutition; on the other hand, it stimulates the afferent fibers of sensory nerves, by which causing further stimulation to swallow center in brain and increase its excitability, so it helps the recovery and reestablishment process of the reflex arc to improve deglutition. In this study, swallowing disorder therapeutic apparatus and mind-refreshing and orifice-opening needling method all have obvious therapeutic effect for deglutition disorder. During follow-up visit period, the changes in all evaluation items showed no statistical significance when compared with that before treatment (allP>0.05), indicating that the two methods have identical and steady long-term effect. The combination of two methods has a better effect than single therapy, indicating that the unity of the treatment has a synergistic effect. Therefore, the combination of the two methods has the merit of improving clinical efficacy, lowering the risk of aspiration and arising QOL.
In our study, we used WST and SSA to evaluate patients’ deglutition. WST can judge the presence of deglutition disorder by observing patients’ drinking condition, and further determine the degree of this disorder, while it cannot observe the presence of aspiration[14-15]. SSA shows good sensitiveness and specificity for evaluating deglutition disorder, and has a relatively high predictability for aspiration[16-19], which is a good remedy for WST. So the combination of the two items can give an overall view for evaluating deglutition.Due to restrictions, cases in our study were all stroke patients in convalescence stage. In the future, we can cooperate with neurology department to conduct clinical observation on stroke patients in acute stage to further explore the adaptability of such methods.
Conflict of Interest
There was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Wanzhou District Scientific and Technological Research Program of Chongqing City (重庆市万州区科学技术项目, No. 201403025).
Statement of Informed Consent
Informed consent was obtained from all individual participants included in this study.
Received: 28 August 2017/Accepted: 24 September 2017
[1] Chinese Society of Neurology. China diagnostic and treatment guidelines for acute ischemic stroke (2010).Zhonghua Shenjingke Zazhi, 2010, 43(2): 146-153.
[2] Rao ML. China Guideline for Cerebrovascular Disease Prevention and Treatment. Beijing: People’s Medical Publishing House, 2007: 64.
[3] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases.Zhonghua Shenjing Waike Zazhi, 1997, 13(1): 3-4.
[4] Shi XM. Xingnao Kaiqiao acupuncture therapy for 7stoke.Zhongguo Linchuang Kangfu, 2003, 7(7): 1057-1058.
[5] Oonishi S, Sun QL. Practical Technique for Rehabilitation of Feeding and Swallowing Disorders. Beijing: Chinese Medical Science Press, 2000: 43-44.
[6] Wu SL, Ma C, Huang FY, Yan TB. Clinical application of the standardized swallowing assessment. Zhonghua Wuli Yixue Yu Kangfu Zazhi, 2008, 30(6): 396-399.
[7] Yan TB, Dou ZL, Ran CF. Practice of Paralysis Rehabilitation. Beijing: People’s Medical Publishing House,2010: 264.
[8] Xiang L, Liu X, Xu ZJ. Therapeutic observation of low-frequency electrical stimulation plus acupuncture for deglutition disorder after cerebral stroke. Shanghai Zhenjiu Zazhi, 2016, 35(12): 1417-1419.
[9] Liu T, Zheng JG. Discussion on Neurophysiology Mechanism of Related Acupoints in Mind-refreshing and Orifice-opening Needling Method. Tianjin: Collected Papers in Seminar on Acupuncture Clinical Service Mode and the Eleventh China Youth Acupuncture and Tuina Academic Meeting of China Institute of Acupuncture and Moxibustion, 2014: 208-209.
[10] Zeng YY. Clinical observation on mind-refreshing and orifice-opening needling method combining conventional acupuncture method on pseudobulbar palsy. Jiangxi Zhongyiyao, 2012, 43(11): 60-61.
[11] Li QP, Wang W, Han YS, Wang WM, Mao YQ, Guo T, Han FQ. Effect of experimental study of Xingnao Kaiqiao acupuncture therapy on the recovery of motor functuion and the expression of SYN on cerebral ischemia reprerfusion rat model at early stage. Zhongguo Zhongyi Jizheng, 2015, 24(1): 19-23.
[12] Zhang LL, Du YZ, Chu Q. Combined the Chinese and Western, made the past serve the present: the four decades development history of consciousness-restoring resuscitation acupuncture treatment on stroke. Liaoning Zhongyi Zazhi, 2011, 38(6): 1240-1243.
[13] Peng WJ, Cui HJ, Liao X, Xing ZH, Luo JK. Effect of Xingnao Kaiqiao Acupuncture on hemorheology of patients with severe craniocerebral injury. Zhongguo Zhongyi Jizheng, 2011, 20(4): 517-518, 530.
[14] Liu JY, Chen YH. Influence of acupoint-injection on TXB2and 6-keto-PGF1ain patients with pseudobulbar palsy: a randomized controlled trial. J Acupunct Tuina Sci, 2017,15(1): 22-26.
[15] Wu WJ, Bi X, Song L, Liu ZH, Zhang JM, Huang Q. Value of applying water swallowing test for patients with dysphagia after acute stroke. Shanghai Jiao Tong Daxue Xuebao (Yixue Ban), 2016, 36(7): 1049-1053.
[16] Guo F, Hao YC. Application of water-swallowing drinking test on stroke patients. Qilu Huli Zazhi, 2016, 22(17): 65-67.
[17] Sun WP, Huang YN, Wang Z, Liu R, Sun W, Chen J. Value of standardized swallowing assessment in screening for aspiration after stroke. Zhongguo Kangfu Lilun Yu Shijian,2009, 15(4): 345-347.
[18] Ma YL, Zhang LM, Zhu QY, Ji XW, Yang JY. Research on the reliability and validity of standardized swallowing assessment (SSA) for the evaluation of deglutition function in aged patients. Huli Xuebao, 2012, 19(3A): 65-67.
[19] Hao GH, Yu BX, Sun YB, Dai MY, Wan W. Application of standardized swallowing assessment in screening postextubation aspiration. Qingdao Daxue Yixueyuan Xuebao,2012, 48(6): 473-475.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation on electroacupuncture plus hydro-acupuncture for low back pain caused by compression fractures
- Effect of acupoint sticking at Shenque (CV 8) for preventing spleen-stomach disharmony caused by venous analgesia pump
- Observation on clinical effects of acupuncture plus external medicine application forcervical radiculopathy
- Observation on clinical efficacy of warm needling therapy for chronic lumbar strain
- Observation on lower-reinforcing and upperreducing acupuncture method for hyperplasia of mammary gland and its influence on estradiol and progesterone
- Influence of acupuncture on pulmonary function of patients with asthma: a review
