Effect of warm joint needling plus rehabilitation on the balance function and quality of life of patients with spastic hemiplegia after ischemic cerebral stroke
2018-06-28HanZhenxiang韩振翔QiLili祁丽丽ZhouYixin周一心ZhangHong张宏ChuLixi褚立希XuWenjie许文杰WangHonglin王宏林LingJun凌隽
Han Zhen-xiang (韩振翔), Qi Li-li (祁丽丽), Zhou Yi-xin (周一心), Zhang Hong (张宏), Chu Li-xi (褚立希),Xu Wen-jie (许文杰), Wang Hong-lin (王宏林), Ling Jun (凌隽)
1 Shanghai No.7 People’s Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai 200137, China
2 Yueyang Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai University of Traditional Chinese Medicine,Shanghai 200437, China
3 Shanghai University of Traditional Chinese Medicine, Shanghai 201203, China
More and more people have been affected by cerebral stroke during the recent years[1]. Spastic hemiplegia is a major post-stroke manifestation of neurological injury, especially upper motor neurons,featured by involuntary contraction and speeddependent stretch hyperreflexia. It is significant to promptly and effectively manage spasticity in restoring the motor function of the patients. Otherwise, the affected limbs may suffer permanent hypermyotonia,stiffness and limited motion of joint[2]. Studies have proved that 20%-40% of cerebral stroke patients may develop limb spasticity[3-4]. In clinical practice,kinesiotherapy is the first choice among all the rehabilitation therapies for spastic hemiplegia[5]. As one of the five classic needling methods, joint needling is often used to treat diseases affecting the meridian sinews. This study was to focus on the effect of warm joint needling plus rehabilitation on the spasticity and balance function of patients after ischemic cerebral stroke.
1 Clinical Materials
1.1 Diagnostic criteria
Conforming to the diagnostic criteria of atherosclerotic thrombotic cerebral infarction from theKey Diagnostic Points for Cerebrovascular Diseases[6].
1.2 Inclusion criteria
Conforming to the above diagnostic criteria; first onset of stroke or the second onset but only after complete recovery of the first one, and disease duration from 3 months to 1 year; graded I-III by the modified Ashworth scale (MAS); in stage II-V estimated by Brunnstrom approach; aged 30-80 years old; with clear consciousness, and scored >24 points by the minimental state examination (MMSE), suggesting no dementia, and capable of cooperating in completing the whole observation; informed consent form obtained.
1.3 Exclusion criteria
Unstable vital signs or significant dysfunction of heart,liver or kidney, or progressively exacerbated condition;severe cognitive impairment or aphasia; coupled with other diseases that can cause hypermyotonia; those with mental disorders so that unable to complete the observation or those having a poor compliance; brain tumor or intracranial space-occupying lesions; brain trauma, parasitic encephalopathy, metabolic disturbance, rheumatic heart disease, coronary heart disease or other heart diseases accompanied by atrial fibrillation leading to cerebral thrombosis; coupled with severe primary diseases involving liver, kidney,hematopoietic system or endocrine system.
1.4 Statistical method
The SAS 9.1.3 statistical software was adopted for data analyses. The measurement daxta were expressedby mean ± standard deviation (±s). The overall comparisons were performed by using a generalized estimation model; inter-group comparisons were analyzed by Kruskal-Wallis test; Friedman test was adopted to compare data at different time points.P<0.05 was taken to indicate a statistical significance.
1.5 General data
A total of 90 patients with hemiplegia after ischemic cerebral stroke were enrolled from the Neurological Rehabilitation Department of Shanghai No.7 People’s Hospital Affiliated to Shanghai University of Traditional Chinese Medicine between April 2014 and September 2016. A full allocation concealment design was adopted by using opaque envelops to seal the assigned numbers.The subjects were divided into a rehabilitation group, a warm joint needling group and an observation group by using the random number table, with 30 cases in each group. The enrolled patients all agreed to participate in the trial and signed the informed consent form. There were no dropouts during the observation. The inter-group differences in the general data were statistically insignificant (P>0.05), (Table 1).

Table 1. Comparison of the general data
2 Treatment Methods
The three groups all received treatments for general medical conditions such as hypertension, coronary disease and diabetes and symptomatic treatments for complications including respiratory infection, urinary infection and enteritis.
2.1 Rehabilitation group
Patients in the rehabilitation group were intervened by Bobath therapy. They had to change their position once every 2 h, alternately between a lateral position and a supine position. Meanwhile, they always had to keep the limbs in a functional position to prevent convulsion. This therapy also included active and passive in-bed movements for hemiplegic limbs;bedside moving training, sitting-standing training in the rehabilitation room and between-chairs transfer training; balance training in standing or sitting position;gait training, climbing stairs, and lower-limb weightbearing exercise; use of braces and walking frames;training for activities of daily living (ADL), such as dressing, feeding themselves, grooming and bathing.
2.2 Warm joint needling group
Based on the theory of meridian sinews, points on shoulder, elbow, wrist and palm nearby the endings of upper-limb flexors were selected; for the lower limb,points on hip, knee and ankle nearby the endings of extensors were selected.
Points: Upper-limb points including Jianyu (LI 15),Chize (LU 5), Quze (PC 3), Daling (PC 7), Tongli (HT 5)and Yuji (LU 10); lower-limb points including Juliao(GB 29), Biguan (ST 31), Xuehai (SP 10), Yanglingquan(GB 34), Xuanzhong (GB 39), Shenmai (BL 62) and Kunlun (BL 60)[7].
Operation: After sterilization of the acupoints, filiform needles of 0.30 mm in diameter and 40-115 mm in length (Hwato brand) were used for acupuncture. The needles were retained for about 20 min after needling qi was obtained. During the retaining, warm needling was applied to each every point by fixing a piece of moxa stick (1 cm in length) onto the needle tail to ignite.The needles were removed when the moxa sticks were burnt out.
2.3 Observation group
Patients in the observation group received the same warm joint needling treatment as those in the warm joint needling group, followed by the same rehabilitation training as those in the rehabilitation group.
The three groups were all intervened once every other day for 1 month as a course of treatment, for 6 months in total.
3 Observation of Therapeutic efficacy
3.1 Observation items
3.1.1 Lower-limb spasticity intensity
The MAS was adopted to measure the hemiplegic spasticity according to the change in muscle tension.Muscle tension was measured in 0-4 levels, the higher the level, the severer the spasticity. Level 0: muscle tone does not increase and the affected limb can be passively moved in the whole range of motion (ROM) without resistance; level 1: muscle tone increases slightly and resistance presents in the passive movement of the affected limb at the end of the ROM; level 1+: muscle tone increases slightly and the passive movement of the affected limb is slightly stuck during the first half of the ROM and slightly resisted during the rest half; level 2:muscle tone increases mildly and resistance presents in the passive movement of the affected limb most of the time, though the passive movement is still available;level 3: muscle tone increases moderately and the passive movement of the affected limb is resisted in the whole ROM and the movement is rather difficult; level 4:muscle tone highly increases and the affected limb is stiff so that it is very difficult to conduct the passive movement.
3.1.2 Balance function evaluation
The balance function was evaluated by Berg balance scale (BBS). The tester observed the patients when they were asked to do the following 14 movements: standing to sitting, standing unsupported, sitting unsupported,sitting to standing, transfers, standing with eyes closed,standing with feet together, reaching forward while standing, retrieving objects from floor, turing head to look behind, turning 360°, stool stepping, tandem standing and standing on one leg. The highest score is 56 points. The lower the score, the worse the balance function, and the higher the possibility of falls[8].
3.1.3 Evaluation of the quality of life (QOL)
The stroke-specific quality of life scale (SS-QOL) was used to estimate the patients’ QOL[9-10]. The scale consists of 49 items which are covered by 12 domains.Each item is scored 1-5. The higher the score, the better the QOL. This scale is suitable to evaluate the outcome of mild-moderate cerebral stroke because of its overall contents and brief questions. It takes less time to finish the scale so that the estimation will not be influenced by fatigue or impaired concentration.
3.2 Time of evaluation
The evaluations were performed at the recruitment,and respectively 2 weeks, 1 month, 3 months and 6 months after the recruitment, 5 times altogether.
3.3 Results
3.3.1 Comparison of the lower-limb spasticity
The repeatedly-measured ranked data were compared by adopting a generalized estimation model.The refined comparison was used to study the factor of grouping and factor of time respectively due to their interaction. The results showed that the lower-limb MAS scores showed significant changes after the intervention in each group (P<0.05), and a time effect was discovered (Table 2).
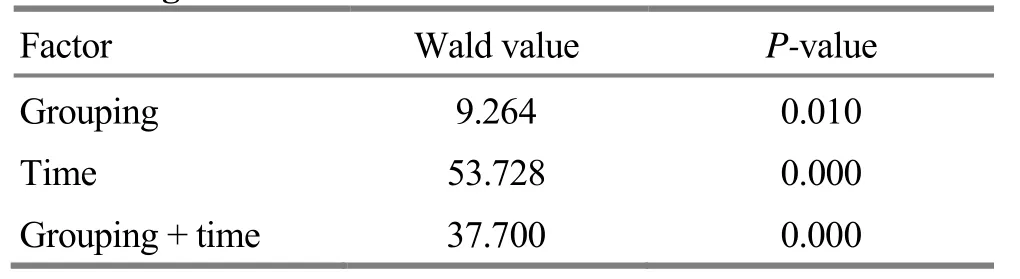
Table 2. Difference in the grouping and time effects in evaluating MAS
Intra-group comparison: the time effect was significant in the warm joint needling group and observation group, and the MAS scores in the two groups were significantly improved after the treatment(P<0.05). Inter-group comparison: the lower-limb MAS scores in the observation group were significantly better than those in the rehabilitation group and warm joint needling group respectively after 3-month and 6-month treatment (P<0.05), (Table 3).
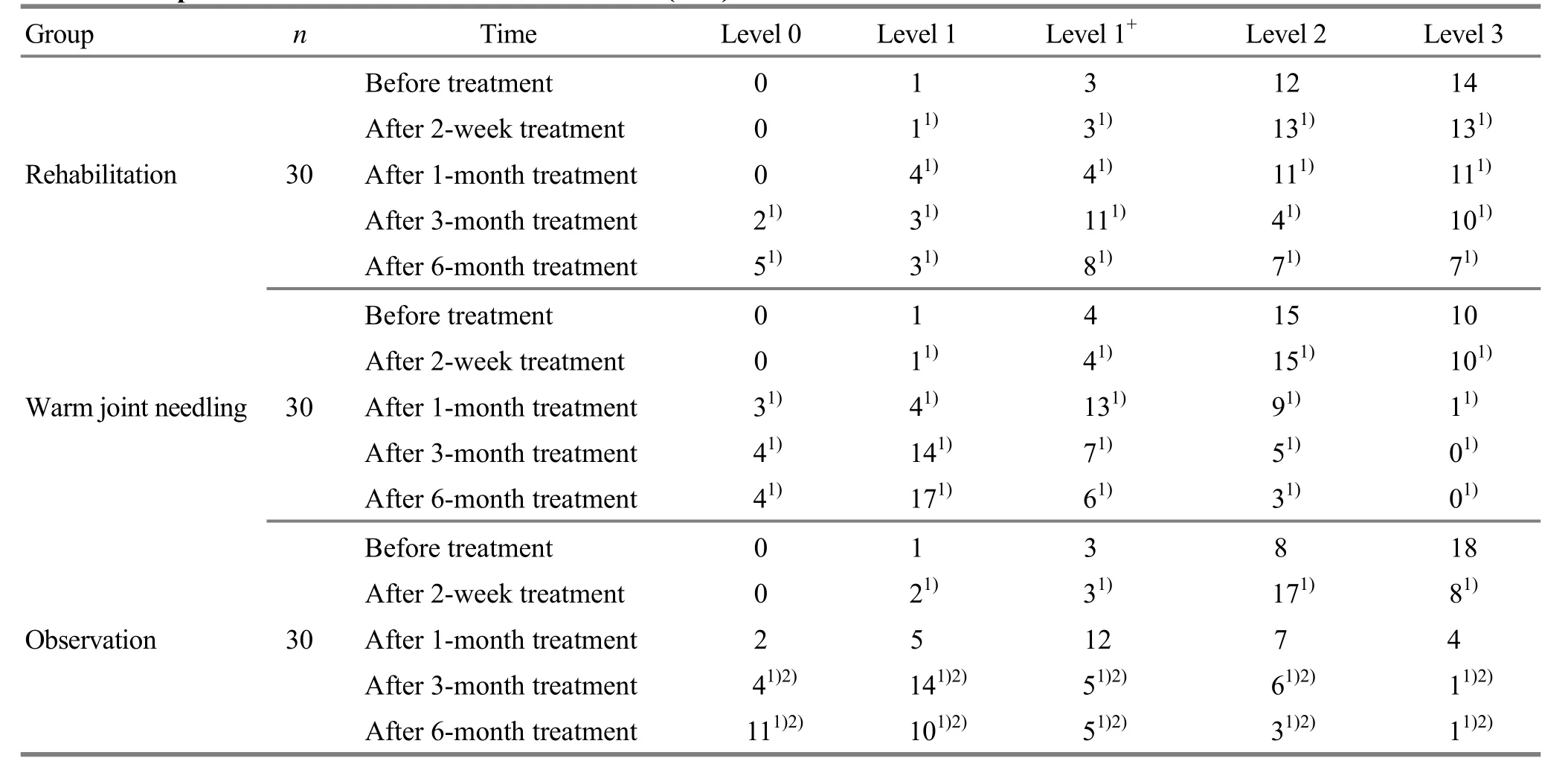
Table 3. Comparison of the lower-limb MAS evaluation (case)
3.3.2 Comparison of the balance function
The repeatedly-measured ranked data were compared by adopting a generalized estimation model.The refined comparison was used to study the factor of grouping and factor of time separately due to their interaction. The results showed that the changes in BBS score were statistically significant after the treatment in the three groups (P<0.05), and a time effect was showed (Table 4).
Intra-group comparison: after 1-month treatment,the three groups all showed a significant time effect,and the BBS scores were significantly improved compared with the corresponding baseline value(P<0.05). Inter-group comparison: respectively after 1-month, 3-month and 6-month treatment, the BBS scores in the observation group were significantly better than those in the rehabilitation group and warm joint needling group (P<0.05), (Table 5).

Table 4. Difference in grouping and time effects in evaluating BBS

Table 5. Comparison of the BBS score (x±s, point)
3.3.3 Comparison of QOL
The repeatedly-measured ranked data were compared by adopting a generalized estimation model.The refined comparison was used to study the factor of grouping and factor of time separately due to their interaction. The results showed that the changes in the SS-QOL score were statistically significant after the treatment in the three groups (P<0.05), and a time effect was found (Table 6).
Intra-group comparison: after 1-month treatment,the warm joint needling group and observation group both showed a significant time effect, and the SS-QOL scores were significantly improved (P<0.05). Inter-group comparison: respectively after 2-week, 1-month,3-month and 6-month treatment, the SS-QOL score in the observation group was significantly superior to that in the rehabilitation group and warm joint needling group (P<0.05), (Table 7).
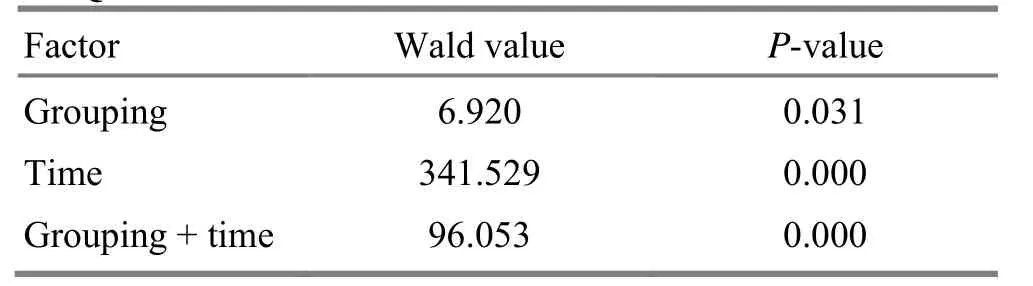
Table 6. Difference in grouping and time effects in evaluating SS-QOL
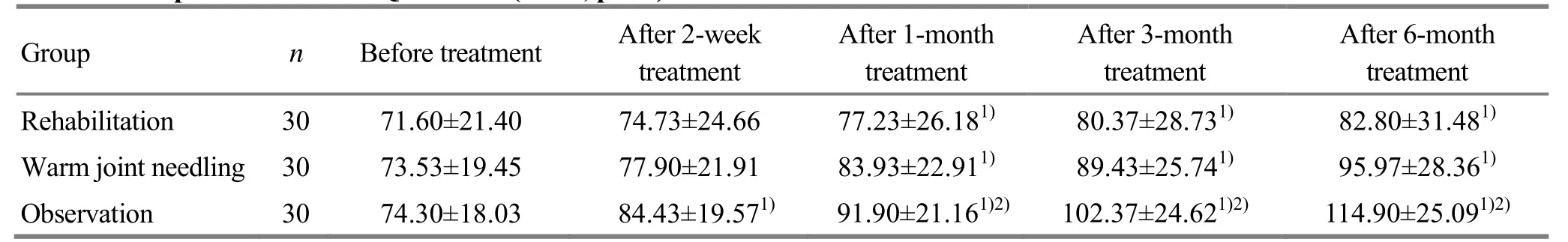
Table 7. Comparison of the SS-QOL score (x±s, point)
4 Discussion
Motor dysfunction after cerebral stroke seriously affects the patients’ daily living and work. In spastic hemiplegia, the affected upper limb and lower limb present diametrically different symptoms. The flexors of the upper limb are spastic while the extensors are flaccid, so that the upper-limb joints are flexed inward.On contrary, the extensors of the lower limb are spastic while the flexors are flaccid, so that the lower-limb joints are over-extended. This special spasticity causes a lifted pelvis while the patient is walking, along with external rotation of lower limb, extended hip and knee joints, strephenopodia, flexed toes, and circumduction gait[11]. Spastic hemiplegia belongs to the scope of Jin Bi(tendon impediment) and should be treated through regulating tendons[12]. Multiple studies have suggested that acupuncture can improve dystonia in cerebral stroke patients[13-14]. Joint needling is an acupuncture method used to treat Jin Bi (tendon impediment) by directly puncturing tendons. It can produce an intensive stimulation and strong needling sensation[15], acting to relax tendons and unblock collaterals, regulate qi-blood flow, and nourish meridian sinews, so as to release spasm[16]. Modern research has shown that fire acupuncture can effectively mitigate spastic hemiplegia in stroke patients and improve the motor function[17],but it is not well accepted by patients. Meanwhile,warm needling has also been found effective in releasing limb spasticity[18-19]and more easily accepted by patients. As the most commonly used rehabilitation therapy, Bobath adopts a reflex-inhibiting pattern to improve the posture, inhibit synkinesis and spasticity,restore a normal muscle tone, and thus help recover motor function. It has been proved by a clinical study that Bobath therapy plus acupuncture-moxibustion can ameliorate the limb function in spastic paralysis after stroke[20]. That is why we used warm joint needling method plus Bobath therapy to treat spastic hemiplegia after cerebral stroke in this study.
Study showed that joint needling produced more significant effects in improving balance function, joint movement, muscle tone and lower-limb spasticity than ordinary needling method in treating spastic hemiplegia,and it also helped correct strephenopodia and gait abnormality[21]. The current study found that warm joint needling plus rehabilitation produced more significant efficacies in improving BBS and MAS evaluations than either warm joint needling or rehabilitation used alone.It is suggested that warm joint needling plus rehabilitation can ameliorate the balance function of spastic hemiplegia patients via easing the lower-limb spasticity state.
The Chinese-version SS-QOL provides an overall evaluation and measure of speech, cognition and vision which are closely associated with cerebral stroke patients from various domains including mental,physiological and social functions[9-10,22]. With high reliability, validity and sensitivity, this scale can comprehensively and objectively reflect the QOL of cerebral stroke patients. Therefore, it can be taken as an efficacy evaluation index in clinical trials. The current study also found that warm joint needling plus rehabilitation can enhance the QOL via improving the lower-limb spasticity and balance function.
To conclude, warm joint needling plus rehabilitation can significantly release the limb spasticity, improve the balance function and QOL of spastic hemiplegia patients after cerebral stroke, and it can produce a satisfactory long-term efficacy.
Conflict of Interest
The authors declared that there was no potential conflict of interest in this article.
Acknowledgments
This work was supported by Program of Health Commission of Pudong New Area, Shanghai (上海市浦东新区卫计委项目No. PW2014B-15); Shanghai New Star in Medical Field (上海市杏林新星, No. ZY3-RCPY-2-2077); Shanghai Academic Community of Leading Talents in Chinese Medicine (上海市中医药领军人才建设项目学术共同体, No. ZY3-RCPY-1-1001); Program of Chinese Medicine Development Office of Shanghai Health Commission (上海市卫计委中发办项目, No.2014LQ030A); Program of Distinguished Young Scholars in Rehabilitation System of Shanghai Disabled Person’s Federation (上海市残联康复系统优青人才项目); Key Discipline (Stroke) Construction Program of Shanghai Pudong New Area [上海市浦东新区重点专科(中风专科)建设项目, No. PDZYXK-1-2014001]; Highland Discipline Construction Program of Shanghai University of Traditional Chinese Medicine (上海中医药大学高原学科建设项目); Chinese Medicine Inheritor Program of No.7 People’s Hospital Affiliated to Shanghai University of Traditional Chinese Medicine (上海中医药大学附属第七人民医院中医继承人项目).
Statement of Informed Consent
Informed consent was obtained from the patients in this study.
Received: 2 September 2017/Accepted: 8 October 2017
[1] Feigin VL, Forouzanfar MH, Krishnamurthi R, Mensah GA, Connor M, Bennett DA, Moran AE, Sacco RL,Anderson L, Truelsen T, O'Donnell M,Venketasubramanian N, Barker-Collo S, Lawes CMM,Wang W, Shinohara Y, Witt E, Ezzati M, Naghavi M,Murray C. Global and regional burden of stroke during 1990-2010: findings from the Global Burden of Disease Study 2010. Lancet, 2014, 383(9913): 245-254.
[2] Deng SY, Hu N, Lu X, Xi SY, Liu C, Bi S. Research on the effects of ankle stretch training on spasticity in patients with stroke: a randomized clinical trial. Zhongguo Kangfu Yixue Zazhi, 2015, 30(12): 1228-1233.
[3] Zorowitz RD, Gillard PJ, Brainin M. Poststroke spasticity:sequelae and burden on stroke survivors and caregivers.Neurology, 2013, 80(Suppl 3): S45-S52.
[4] Sommerfeld DK, Eek EU, Svensson AK, Holmqvist LW,von Arbin MH. Spasticity after stroke: its occurrence and association with motor impairments and activity limitations.Stroke, 2004, 35(1): 134-139.
[5] Li S. Spasticity, motor recovery, and neural plasticity after stroke. Front Neurol, 2017, 8: 120.
[6] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases.Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[7] General Administration of Quality Supervision, Inspection and Quarantine of the People’s Republic of China,Standardization Administration of the People’s Republic of China. Nomenclature and Location of Acupuncture Points(GB/T 12346-2006). Beijing: Standards Press of China,2006.
[8] Zhou JG, Fan JZ. Analysis of the effectiveness of Morse fall scale and Berg balance scale applied in the fall risk prediction for senile patients. Zhongguo Kangfu Yixue Zazhi, 2012, 27(2): 130-133.
[9] Hui JR, Pei J, Song Y, Fu QH, Hui JP. Overview of research and application of patient-reported outcomes in stroke. Shanghai Zhongyiyao Daxue Xuebao, 2009, 23(4):85-88.
[10] Hui JR, Pei J, Wang YC, Hui JP, Fu QH, Song Y, Li HY,Liu ZD. Research analysis on stroke-specific quality of life(SS-QOL) scale of acupuncture intervention on stroke.Zhongguo Zhen Jiu, 2013, 33(4): 363-366.
[11] Liu J, Chen LF, Zhou J, Wang CY, Fang JQ. Efficacy on the range of motion of the lower limbs in patients of poststroke spasmodic paralysis regulated with multi-directional stimulation technique. Zhongguo Zhen Jiu, 2016, 36(10):1013-1017.
[12] Liu ZM, Wei D. Research progress of acupuncturemoxibustion in treating spastic hemiplegia. Guangxi Zhongyiyao, 2015, 38(4): 12-14.
[13] Burke D, Wissel J, Donnan GA. Pathophysiology of spasticity in stroke. Neurology, 2013, 80(Suppl 2): S20-S26.[14] Ellis MD, Schut I, Dewald JP. Flexion synergy overshadows flexor spasticity during reaching in chronic moderate to severe hemiparetic stroke. Clin Neurophysiol,2017, 128(7): 1308-1314.
[15] Zhang Y, Guo CQ. Study on joint needling. Shanghai Zhenjiu Zazhi, 2013, 32(7): 580.
[16] He XH, Hu YH, Ke SH, Yang LF. Effect of Hui and Guan puncture and routine acupuncture method on cases with upper limb spasticity after stroke. Ningxia Yike Daxue Xuebao, 2013, 35(11): 1247-1249.
[17] Wang N, Li ZF. Life quality improvement of spastic hemiplegia of stroke treated with fire needle: a randomized controlled trial. Zhongguo Zhen Jiu, 2015, 35(11): 1105-1109.
[18] Fang XH, Zhou WH, Chen LH, Zhou P. Effect of warming needle on the excitability of spinal motor neuron of patients with spastic hemiplegia due to stroke. Shanxi Zhongyi,2014, 30(7): 34-35.
[19] Fang XH, Zhou P, Zhou WH, Chen LH. Warm acupuncture in the treatment of spastic hemiplegia after stroke. Zhenjiu Linchuang Zazhi, 2011, 27(4): 50-51.
[20] Yang AG, Yan XH, Zhao Y. Clinical observation of acupuncture plus Bobath therapy for motor dysfunction of core muscles in patients with post-stroke hemiplegia.Shanghai Zhenjiu Zazhi, 2015, 34(2): 105-108.
[21] Yan RJ, Cheng B, Chen LS, Shen XY, Zong L. Clinical observation of relaxing needling plus joint needling from the Internal Medicine for post-stroke spastic hemiplegia.Shanghai Zhenjiu Zazhi, 2016, 35(8): 930-934.
[22] Cai YF, Jia Z, He CX, You JS, Bai XX, Guo JW, Ou AH,Liang WX, Pei J, Huang Y, Huang PX. Multi-centered study of SS-QOL of Chinese version. Zhongguo Zhongyi Jichu Yixue Zazhi, 2007, 13(7): 551-553.
猜你喜欢
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Clinical observation on electroacupuncture plus hydro-acupuncture for low back pain caused by compression fractures
- Effect of acupoint sticking at Shenque (CV 8) for preventing spleen-stomach disharmony caused by venous analgesia pump
- Observation on clinical effects of acupuncture plus external medicine application forcervical radiculopathy
- Observation on clinical efficacy of warm needling therapy for chronic lumbar strain
- Observation on lower-reinforcing and upperreducing acupuncture method for hyperplasia of mammary gland and its influence on estradiol and progesterone
- Influence of acupuncture on pulmonary function of patients with asthma: a review
