Electroconvulsive therapy for agitation in schizophrenia: meta-analysis of randomized controlled trials
2017-11-29XiaojingGUWeiZHENGTongGUOGaborUNGVARIHelenCHIUXiaolanCAOCarlARCYXiangfeiMENGYupingNINGYutaoXIANG0
Xiaojing GU, Wei ZHENG, Tong GUO, Gabor S. UNGVARI, Helen F.K. CHIU, Xiaolan CAO,, Carl D’ARCY,Xiangfei MENG, Yuping NING*, Yutao XIANG0*
•Systematic review and meta-analysis•
Electroconvulsive therapy for agitation in schizophrenia: meta-analysis of randomized controlled trials
Xiaojing GU1#, Wei ZHENG2#, Tong GUO3, Gabor S. UNGVARI4,5, Helen F.K. CHIU6, Xiaolan CAO6,7, Carl D’ARCY8,Xiangfei MENG9, Yuping NING1*, Yutao XIANG10*
Electroconvulsive therapy; agitation; schizophrenia; headache, meta-analysis
1. Introduction
Agitation, excessive motor and/or verbal activity,characterized by excitement, restlessness, and psychic and motor tension, is common in patients with schizophrenia. Agitation can escalate into aggressive behavior leading to high risk of injury for patients,relatives or staff.[1-3]Furthermore, agitation increases the frequency of patient emergency department visits with further negative consequences.[4]
In order to minimize the risk posed to self or others, agitated patients should be managed, first and preferably by non-pharmacological interventions such as environmental and behavioral modification,and secondly by pharmacological agents.[3-5]However,in most cases the management of agitation largely depends on pharmacological agents,[6]mainly benzodiazepines and antipsychotics (APs) with their well-known adverse effects particularly if they are administered repeatedly.[1,3]
Electroconvulsive therapy (ECT) is a fast, effective and safe treatment for a variety of psychiatric disorders.[7]Use of ECT for acute or even prolonged agitation has received scant attention in contemporary literature and it appears that ECT is hardly ever used for this purpose in developed countries. However,ECT remains an option for agitation or aggression in China and developing countries.[8]There have been a number of studies published in China, including randomized controlled trials (RCTs)[9-15]to compare the efficacy of ECT alone or the ECT-AP combinations to AP monotherapy with conflicting results.
To the best of our knowledge, no systematic review or meta-analysis of ECT treatment for agitation in schizophrenia has been published. This was the impetus for this meta-analysis concerning the efficacy and safety of ECT treatment for agitation in schizophrenia.
2. Methods
2.1 Selection of studies
According to PICOS acronym, the inclusion criteria were: Participants (P): adult schizophrenia patients(≥18 years) with agitation. Intervention (I): ECT alone and ECT-AP combination. Comparison (C): AP monotherapy. Outcomes (O): primary outcomes were the improvement of agitation related outcomes at lastobservation-carried-forward (LOCF) study endpoint measured by the Positive and Negative Syndrome Scale(PANSS),[16]Brief Psychiatric Rating Scale (BPRS),[17]and any other scales or sub-scales or item for agitation: 1)total psychopathology scores, 2) the excitement subscores, and 3) the agitation sub-scores. Key secondary outcomes included early symptomatic improvement (at 1, 3, 7, and 14 days), rate of all-cause discontinuation and patient-reported adverse events. Study design (S):RCT with available data. The exclusion criteria were case series, non-randomized studies, and non-original research (reviews and meta-analyses).
2.2 Search strategy
English databases (PubMed, PsycINFO, and Cochrane Library) and Chinese databases (WanFang Database,Chinese Biomedical Database and China Journal Net) were searched, from their inception until Feb 3, 2017 using the following search terms: (1) English databases: (ECT OR Electric Convulsive Therap* OR Therap*, Electric Convulsive OR Electroshock Therap*OR Convulsive Therap*, Electric) OR Electroconvulsive Therapy OR Electroconvulsive Therapies OR Therap*,Electroconvulsive OR Electric Shock Therap* OR Shock Therap*, Electric OR Therap*, Electric Shock OR Therap*, Electroshock) AND (schizoaffective disorder OR schizophreniform OR Schizophrenic Disorder OR Disorder, Schizophrenic OR Schizophrenic Disorders OR Schizophrenia OR Dementia Praecox) AND (agitation OR exciting OR aggression); (2) Chinese databases: (电休克 OR 电抽搐 OR ECT OR MECT OR 电痉挛) AND (激越 OR 攻击 OR 兴奋)AND 随机 AND (精神分裂症OR 精神分裂). The search was supplemented by using the “related article” function. Hand-searched reference lists from relevant review articles for additional studies were hand-searched and authors contacted for unpublished data.
2.3 Data extraction
Two independent evaluators (GXJ and ZW) selected studies, extracted data, conducted quality assessment and data synthesis. Any inconsistencies were resolved by discussion to reach consensus or involvement of a third reviewer (XYT).
2.4 Data synthesis and statistical analyses
Clinical outcomes were based on intent-to-treat (ITT)analysis, if available. The meta-analysis was performed using Review Manager (version 5.3) according to the recommendations of the Cochrane Collaboration.[18]To combine studies, the random effects model[19]was used in all cases. For continuous data and dichotomous data, weighted mean differences (WMDs) associated with their 95% confidence intervals (CIs) and risk ratio (RR) ±95% CIs were calculated, respectively. We reported the number-needed-to-treat (NNT) or numberneeded-to-harm (NNH) calculated by dividing 1 by the risk difference as soon as RR was significant. One study[11]from the ‘ECT alone’ group had three study arms.According to the methodology of prior meta-analysis,[20]we should include each of the 2 ECT arms separately in one RCT[11]with 3 treatment arms. Furthermore,the APs monotherapy arm was included twice in the analysis, but half of all patients were randomized to each AP arm in order not to inflate the number of patients in the APs monotherapy arm.
In case of I2≥50% for the effect of primary outcome on the PANSS total score, a sensitive analysis was conducted by excluding one outlying study[15]with an outlying effect size (ES) of less than -1.24 (i.e.,more than 1.24 standard deviation superiority of ECTAP combination) in the ‘ECT-AP combination’ group.Furthermore, subgroup and meta-regression analyses were conducted to detect the sources of heterogeneity,if possible. Publication bias was assessed using funnel plots and Egger’s test.[21]All statistical differences were considered significant when p<0.05.
2.5 Assessment of study quality
The Cochrane risk of bias[18]was used to assess the quality of each study. Furthermore, the quality of each study was also assessed with the Jadad scale that assesses study quality on a 5-point scale along the following five domains: “randomization,” “double blinding,” “description withdrawals and dropouts,”“generation of random numbers,” and “allocation concealment”.[22]The criteria of high and low quality were defined as Jadad score ≥4 and <4, respectively.
2.6 Clinical evidence recommendation
The grading of recommendations assessment,development, and evaluation (GRADE) system[23]was used to judge the quality of clinical evidence recommendations of the meta-analytic results of ECT for agitation in schizophrenia.
3. Results
3.1 Results of the search
Altogether 133 potentially relevant articles from English(n=96) and Chinese databases (n=37) were identified;duplication excluded 14 studies. Of the remaining 119 entries, 112 were determined to be irrelevant after review of the titles and abstracts, a further 7 were removed on the basis of full text review. Finally, 7 RCTs with 8 treatment arms met the selection criteria for the meta-analysis (Figure 1).
3.2 The characteristics of included studies
The seven RCTs lasted an average of 4.3(3.1) weeks(range: 2-8 weeks; median: 2 weeks). The total number of participants in all the studies was 480 (range: 30-100, median: 60). All the RCTs that met our inclusion and exclusion criteria were thus included in the metaanalysis had been conducted in China. Aggregating data across all the reviewed trials: there were 240 patients in ECT monotherapy vs. AP monotherapy (n=135 vs.n=105) comparison and 240 patients in the ECT-AP vs.AP monotherapy (n=120 vs. n=120) comparison (Table 1); patients were on average 34.3(4.5) years old (range:31.9-43.5 years; median: 32.5 years) in 6 RCTs with available data; 57.6(14.2)% were males (range: 40.0%-80.0%; median: 56.7%); and the mean illness duration with available data (6 RCTs) was 2.7(2.7) years (range:0.02-6.1 years; median: 2.2 years).
3.3 Assessment of risk of bias and quality assessment
The Cochrane risk of bias was presented in Table 2.85.7% (6/7) RCTs only mentioned “random” assignment,lacking a detailed description of the method of randomizing and thus were rated as unclear. However,only one RCT[13]using random assignment according to the random number table was rated as low risk.Given that all included studies were open label, the allocation bias, performance bias, and detection bias were rated as high risk. None of the included RCTs presented the study registration materials, which limited us to determine whether or not there was selective reporting (i.e., reporting bias). Furthermore,it was impossible to judge the other types of biases(e.g., drug company sponsorship of the study) due to lack of available evidence. Overall, 7 included RCTs suffered from high risk of bias and were considered as relatively low-quality studies. The Jadad score was 2.0(0.6) (range=1-3, median=2) (Table 1). All RCTs were rated as low quality (Jadad score < 4). Due to pooling of data, less than 3 RCTs with 4 treatment arms were in all forest plots, thus funnel plot analysis to show the presence of risk of publication bias could not be conducted.
3.4 The improvement of agitation related outcomes
There were differences between the ECT alone vs AP (4 RCTs with 5 treatment arms) and ECT-AP vs AP (3 RCTs)groups. Moreover, the improvement of agitation related outcomes were measured using PANSS in all included RCTs.
ECT alone vs AP: ECT alone was superior to AP monotherapy with respect to PANSS total score (WMD=-7.13, (95%CI: -11.99, -2.27), I2=0%, p=0.004, Figure 2) and excitement sub-score (WMD=-1.97, (95%CI: -2.87, -1.08),I2=0%, p<0.0001, Figure 2), but not in the agitation subscore (WMD=-0.90, p=0.38); ECT alone was superior to AP monotherapy in PANSS total score at 14 days (WMD:-7.13 (95%CI:-11.99, -2.27), p=0.004; I2=0%, Supplemental Figure 1), but not at 1 and 7 days (WMD:-5.23 to -7.13(95%CI:-16.86, 4.25), p=0.06 to 0.24; I2=0% to 77%,Supplemental Figure 1). Furthermore, subgroup and meta-regression analyses could not be performed due to the limited number of RCTs.
Furthermore, ECT alone was superior to AP monotherapy in PANSS excitement sub-score at 7 and 14 days (WMD:-1.97 to -1.92 (95%CI:-3.14, -0.71),p=0.002 to 0.0001; I2=0%, Supplemental Figure 2), but not at 1 day after ECT treatment (WMD:-1.92 (95%CI:-4.00, 0.17), p=0.07; I2=35%, Supplemental Figure 2).Among the ECT alone studies one RCT[10]used Clinical Global Impression (CGI) and found an advantageous improvement of psychiatric symptoms in the ECT group at 7 and 14 days.
ECT plus AP vs AP: Regarding the PANSS total score, the ECT-AP combination was superior to AP monotherapy (WMD=-10.40, (95%CI: -19.67, -1.12),I2=93%, p=0.03, Figure 3), but not in the excitement and agitation sub-scores (WMD=-1.06 to -1.34, p=0.33 to 0.37). The significant difference between the two groups in the PANSS total score disappeared after one outlying study[15]was removed (WMD:-4.23 (95%CI:-8.89, 0.43), p=0.08; I2=76%). Furthermore, subgroup and meta-regression analyses could not be performed due to the limited number of RCTs.
Furthermore, adding ECT to AP was superior to AP monotherapy at 7 days for the PANSS total score(WMD=-5.01, (95%CI: -9.37, -0.66), I2=14%, p=0.02,Figure 4), but not to PANSS total score (p=0.15),excitement (p=0.35) and agitation sub-scores (p=0.44)at 14 days (Figures 4).
3.5 Side ef f ects and discontinuation rate
The Treatment Emergent Symptom Scale (TESS) was generally used to assess adverse drug reactions (ADRs)in these RCTs however such data were not available in 1 RCT (Table 1). None of the included RCTs reported the rate or cause of treatment discontinuation.
ECT alone vs APs: Headache (p=0.0001, NNH=3,95%CI=2-4) was the only ADRs more frequent in the ECT alone group compared to AP monotherapy(Supplemental Figure 3). There was significantly less akathisia (p=0.02, NNH=8, 95%CI=5-17) and electrocardiogram changes (p=0.05) with borderline significance in the ECT alone group compared to the AP group. Meta-analysis of uroclepsia, weight gain, upper respiratory infections, tremor, dry mouth, insomnia,and electroencephalography changes did not differ between the groups (Supplemental Figure 3).
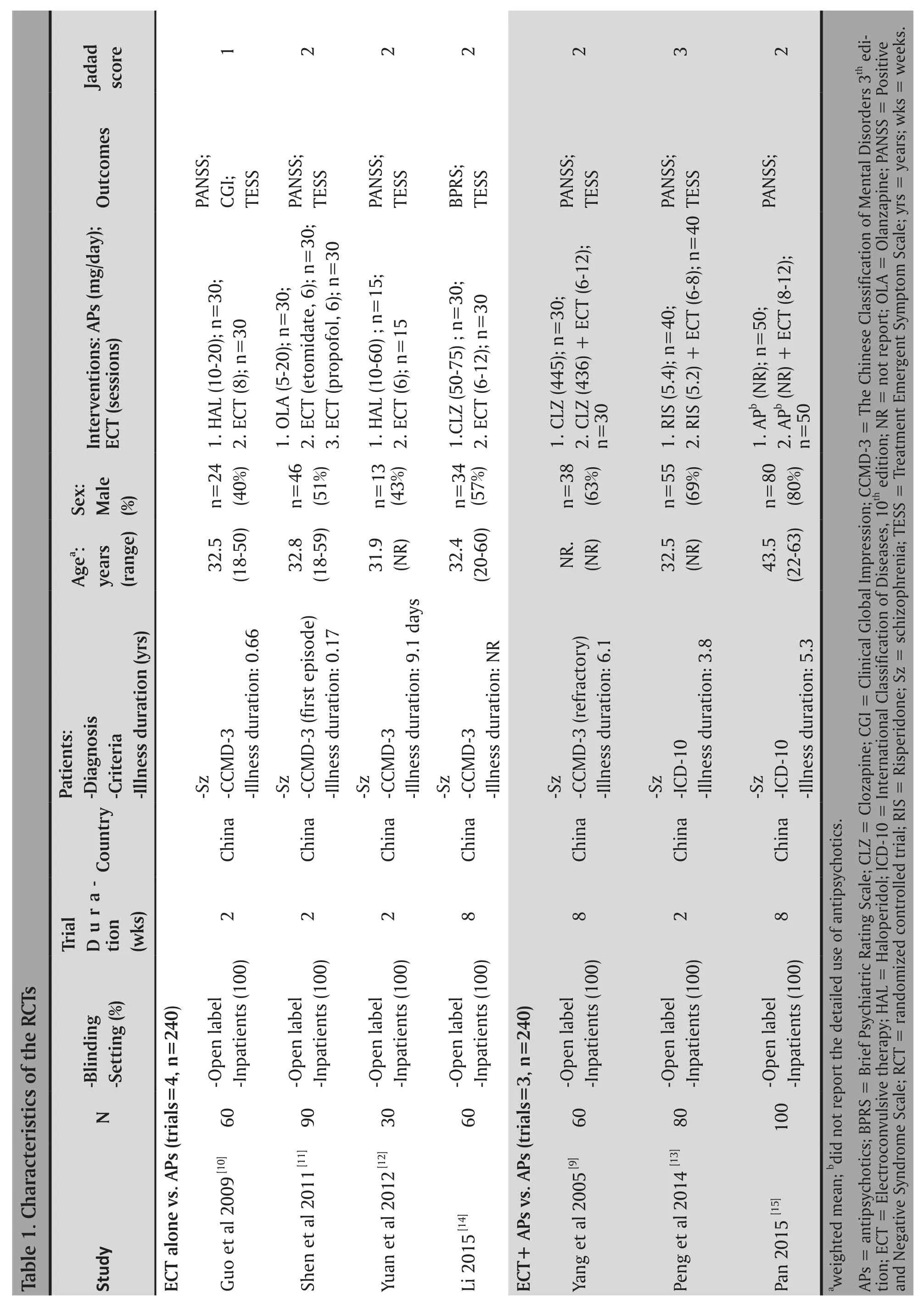
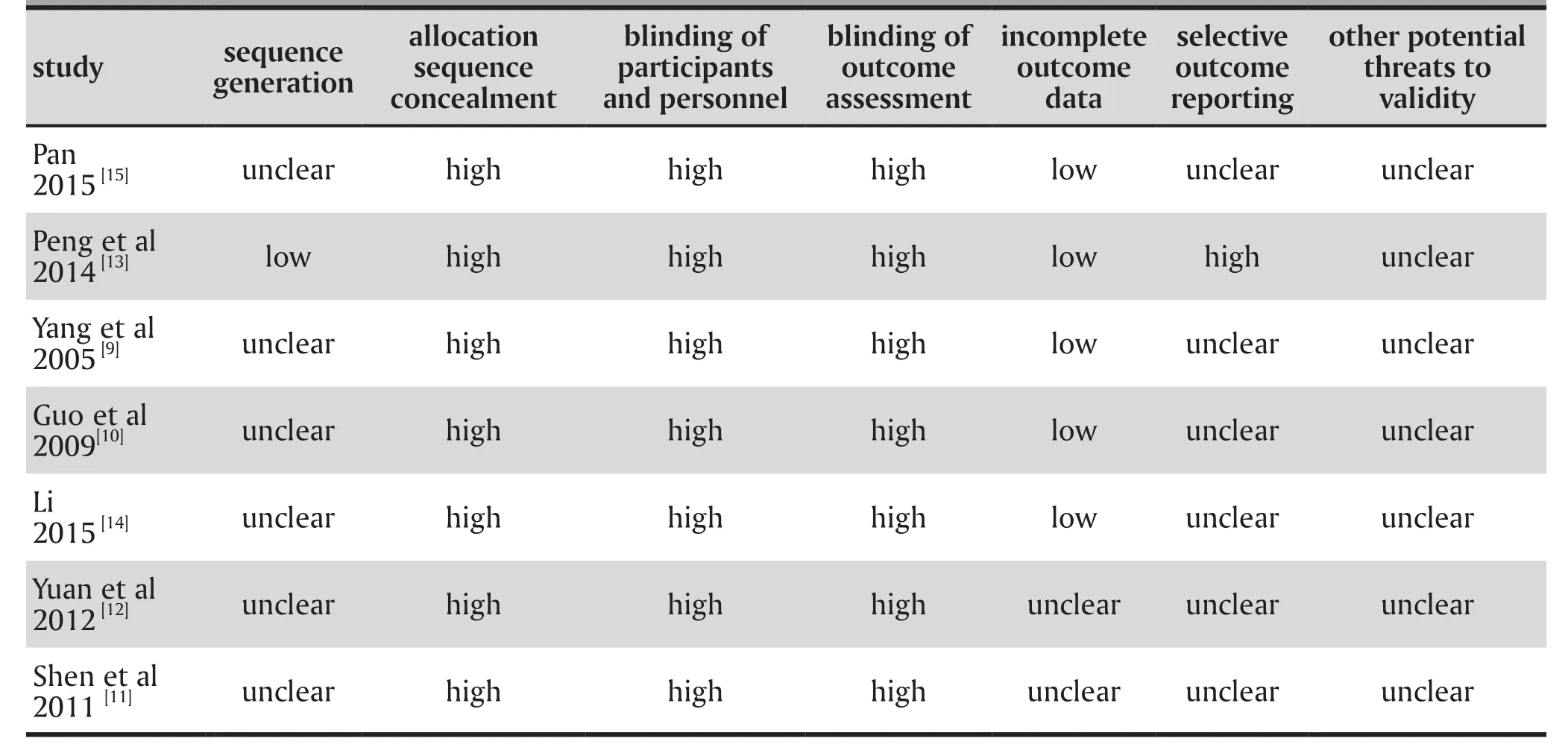
Table 2. Evaluation of risk of bias in the seven included studies
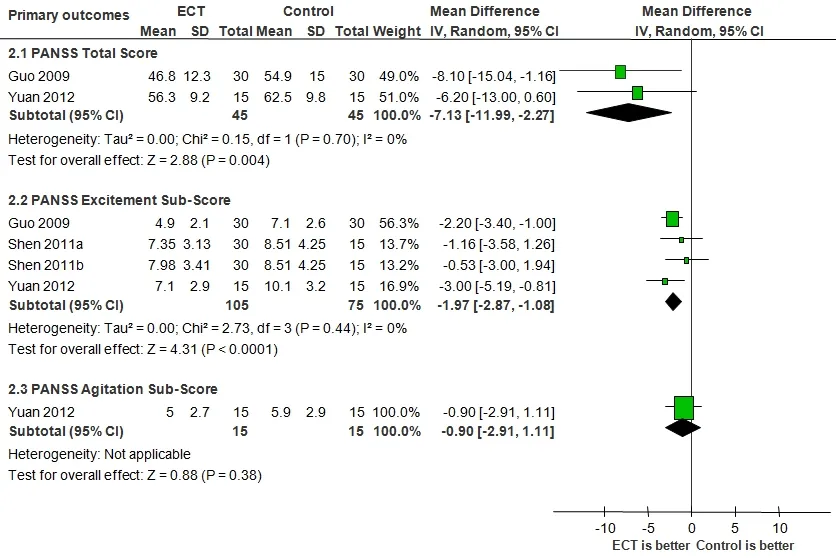
Figure 2. ECT alone for agitation in schizophrenia: forest plot for the Positive and Negative Syndrome Scale(PANSS) total score and its PANSS excitement and agitation sub-scores at endpoint
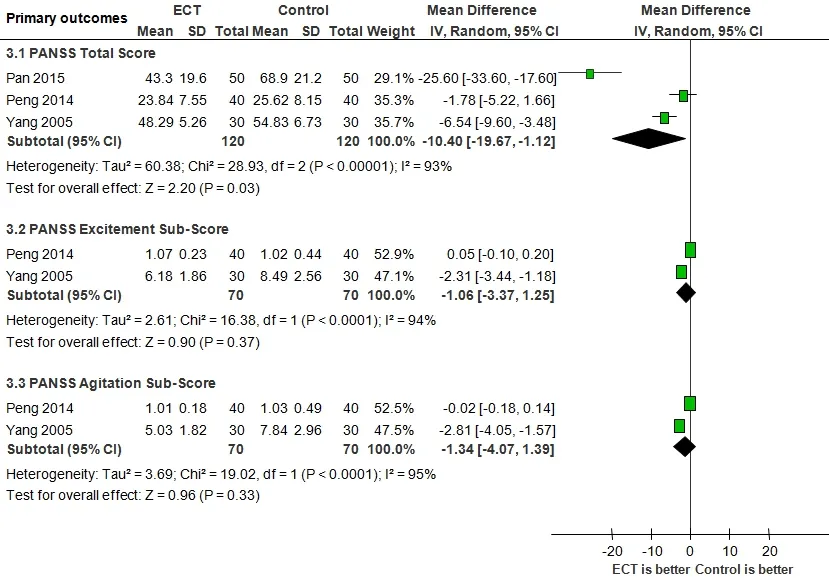
Figure 3. Add-on ECT to antipsychotics for agitation in schizophrenia: forest plot for the Positive and Negative Syndrome Scale (PANSS) total score and its excitement and agitation sub-scores at endpoint
ECT plus AP vs AP: Only two RCTs[9,13]reported the ADRs without meta-analyzable data.
3.6 Clinical evidence recommendation
Clinical evidence recommendation of the main metaanalytic outcomes based on the GRADE approach showed some limitations of risk of bias, inconsistency and publishing bias, and no obvious indirectness or imprecision. According to the above assessments, the quality of evidence of 8 outcomes presented in Table 3 and ranged from ‘very low’ (37.5%), “low” (50%), to‘high’ (12.5%).
4. Discussion
4.1 Main findings
Despite a systematic literature search in both English and Chinese-language databases, we only identified 7 RCTs with 8 treatment arms that examined the efficacy and safety of using ECT for the treatment of agitation in 480 patients with schizophrenia who are currently using APs. All included RCTs were open label and the assessment of outcomes was not blinded in all trials.Furthermore, the quality of all included RCTs was rated as ‘low quality’ based on Jadad scale. Overall, the results suggest that both ECT alone and the ECT-AP combination over 2 to 8 weeks had superior efficacy to AP monotherapy regarding the reduction in PANSS total score, but not in the agitation sub-score. ECT and ECT-AP combination were both safe and well tolerated.The reduction in the total PANSS score with ECT alone was superior to AP monotherapy as early as at 1 day with a moderate effect size of -0.52, which increased to a relatively larger effect size of -0.60 after 14 days.The ECT-AP combinations were significantly superior to AP monotherapy with respect to PANSS total score at 7 days with a small effect size of -0.36. However,35 patients reported headache (38.9% vs. 0% on APs monotherapy, NNH=3), which was significantly more common in the ECT alone group. These adverse effects were transient and mild.[10,11]
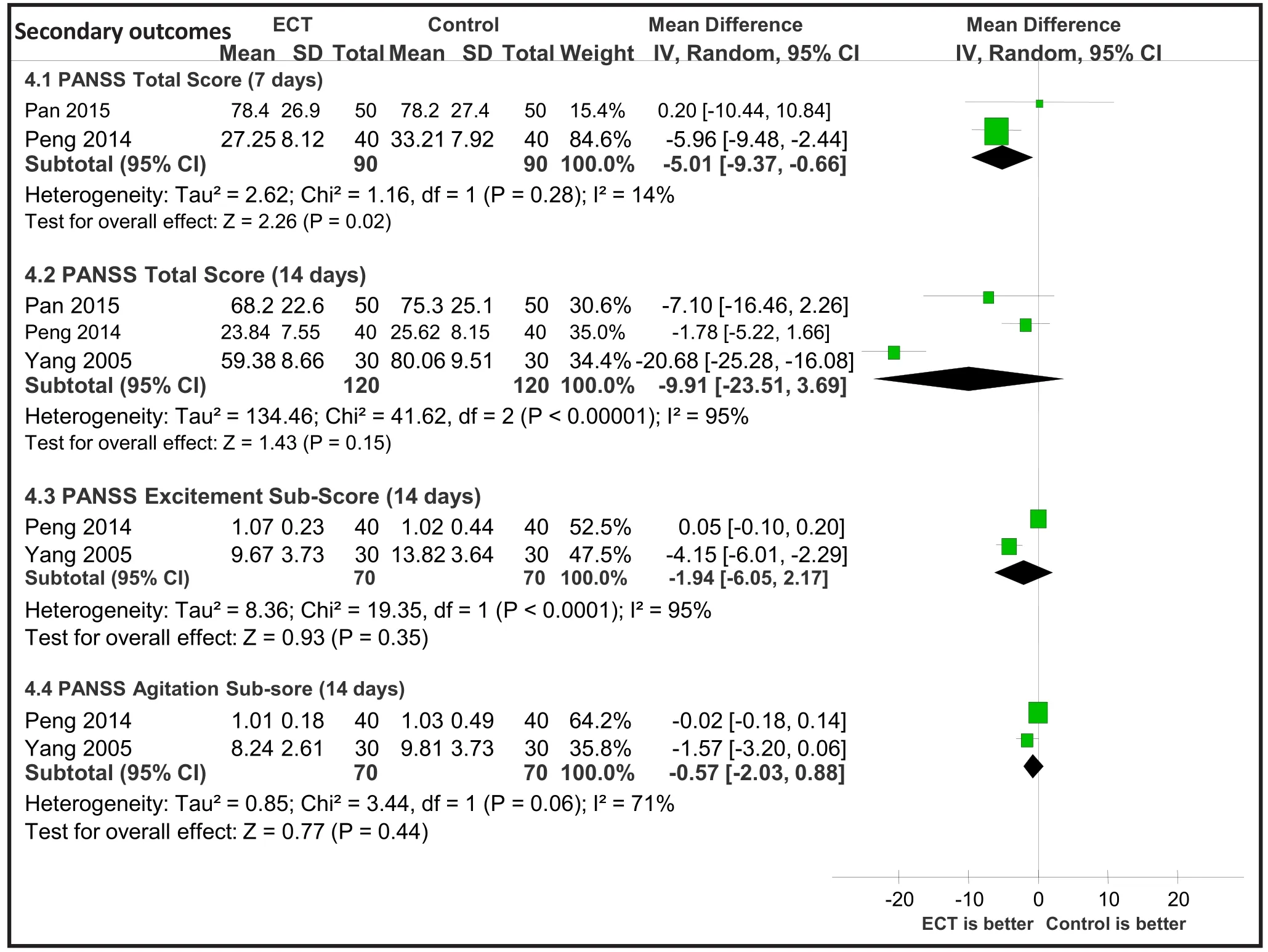
Figure 4. Add-on ECT to antipsychotics for agitation in schizophrenia: forest plot for the Positive and Negative Syndrome Scale (PANSS) total score at 7 and 14 days as well as PANSS agitation and excitement subscore at 14 days
4.2 Limitations
Several limitations need to be acknowledged. First, 7 RCTs (100%) reviewed were rated as low quality and the strength of the evidence for 87.5% outcomes was rated as“very low” or “low” according to the GRADE approach.However, strong recommendations does not necessarily imply high quality evidence and low quality evidence can still result in strong recommendations.[23]Further,the RCTs were inconsistent in their methodology with respect to sampling and the delivery of ECT and the type and dose of antipsychotic medications. Subgroup analyses and meta-regression cannot be employed to lessen the heterogeneity of primary outcomes. Second,data regarding the cognitive effects of ECT were not systematically assessed in the included studies. In addition, agitation, the target symptom in this study, was evaluated with a single item in the PANSS, rather than with a standardized rating scale. Furthermore, some more variables potentially associated with agitation, such as the quality of care and patients’ education, were not assessed in included studies. Third, treatment adherence was not routinely assessed or reported. In particular, the ECT dose-response effects on agitation when used as monotherapy or/and co-treatment in agitation patients with schizophrenia, definitely needs to be more fully evaluated. Finally, all studies were conducted in China thus the findings need to be replicated in other countries.
4.3 Implications
Although this paper included 7 low quality RCTs with small samples and the methodological limitations[23]identified, the thorough methodology of this meta-analysis included the assessment of quality using the Cochrane risk of bias,[18]Jadad scale[22],and GRADE system.[23]The heterogeneity of PANSS total score assessed by I2decreased from 93% to 76%after removing one outlying study;[15]in addition,the significance disappeared, which could be due to the decreased sample size thereby reducing thepower detecting significant results. The previous meta-analyses[24-25]supported our interpretation that adjunctive ECT can be an efficacious treatment for improving total psychopathology in schizophrenia patients. Agitation poses a significant challenge in the treatment of schizophrenia.[1]However, the current meta-analysis of 7 relatively low quality RCTs showed that both ECT alone and the ECT-AP combination are ineffective treatments for agitation in 480 Chinese schizophrenia patients. This meta-analysis indicates that other symptoms (e.g. hallucination, delusion, etc.)maybe respond better to ECT when compared with agitation related outcomes in schizophrenia patients.
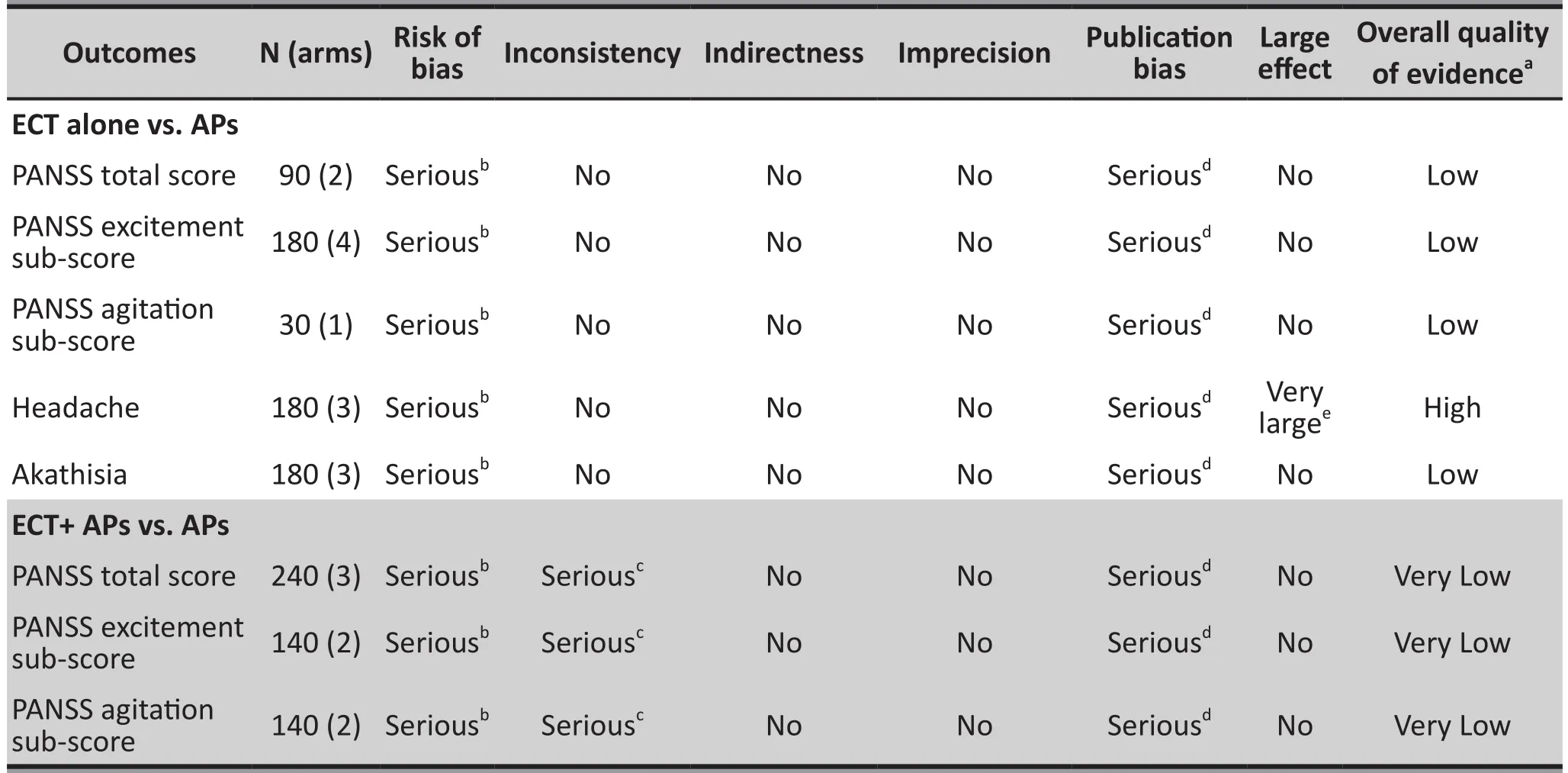
Table 3. GRADE Analyses for main primary and secondary outcomes: ECT for agitation in schizophrenia
Funding
The study was supported by the Start-Up Research Grant (SRG2014-00019-FHS) and the Multi-Year Research Grant (MYRG2015-00230-FHS) from the University of Macau. The University of Macau had no role in the study design, generating or interpreting the results and publication of the study.
Conflicts of interest statement
The authors declare that they have no conflicts of interest concerning this article.
Acknowledgements
GXJ designed the study and was assisted by ZW and GT in the search for papers, data extraction, and analysis.WZ and GXJ drafted the manuscript. GSU, HFKC, CDA,and MXF made critical revisions to the manuscript.All authors approved the final version for publication.The authors thank Cai Dong-Bin (Faculty of Traditional Chinese Medicine, the First Clinical Medical College,Guangzhou University of Chinese Medicine) for downloading relevant articles.
1. Siwek M. [Inhaled loxapine: A novel treatment for agitation in psychotic disorders]. Psychiatr Pol. 2014; 48(5): 917-930.Polish
2. Nordstrom K, Allen MH. Alternative delivery systems for agents to treat acute agitation: progress to date. Drugs.2013; 73(16): 1783-1792. doi: http://dx.doi.org/10.1007/s40265-013-0130-3
3. Hankin CS, Bronstone A, Koran LM. Agitation in the inpatient psychiatric setting: a review of clinical presentation, burden, and treatment. J Psychiatr Pract.2011; 17(3): 170-185. doi: http://dx.doi.org/10.1097/01.pra.0000398410.21374.7d
4. Citrome L. Addressing the need for rapid treatment of agitation in schizophrenia and bipolar disorder: focus on inhaled loxapine as an alternative to injectable agents.Ther Clin Risk Manag. 2013; 9: 235-245. doi: ht t p://dx.doi.org/10.2147/TCRM.S31484
5. Gonzalez D, Bienroth M, Curtis V, Debenham M, Jones S, Pitsi D, et al. Consensus statement on the use of intramuscular aripiprazole for the rapid control of agitation in bipolar mania and schizophrenia. Curr Med Res Opin.2013; 29(3): 241-250. doi: ht t p://dx.doi.org/10.1185/03007 995.2013.766591
6. Koster LS, Carbon M, Correll CU. Emerging drugs for schizophrenia: an update. Expert Opin Emerg Drugs. 2014; 19(4):511-531. doi: ht t p://dx.doi.org/10.1517/14728214.2014.958148
7. UK ECT Review Group. Efficacy and safety of electroconvulsive therapy in depressive disorders: a systematic review and meta-analysis. Lancet. 2003;361(9360): 799-808. doi: ht t p://dx.doi.org/10.1016/S0140-6736(03)12705-5
8. Zheng W, Tong G, Ungvari GS, Ng CH, Chiu HF, Xiang YQ, et al. Memory impairment following electroconvulsive therapy in chinese patients with schizophrenia: Meta-analysis of randomized controlled trials. Perspect Psychiatr Care. 2017;doi: http://dx.doi.org/10.1111/ppc.12206. Epub ahead of print
9. Yang KJ, Liu TB, Yang HC, Gao H, Wu DH, et al. [The effect of clozapine combined MECT for the resistant schizophrenics with agitation and aggressive behavior]. Zhongguo Ren Ming Jian Kang Yi Xue Za Zhi. 2005; 17: 485-486. Chinese
10. Guo HM. [A control study of MECT in the treatment of agitated behavior of schizophrenia]. Lin Chuang Xin Shen Ji Bing Za Zhi. 2009; 15(6): 488-489. Chinese.doi: http://dx.chinadoi.cn/10.3969/j.issn.1672-187X.2009.06.004.0488-02
11. Shen T, Wang B, Li C, Wang HF, Wang XL, Han HQ.[The effective study of olanzapine and MECT in acute schizophrenia patients]. Sichuan Jing Shen Wei Sheng. 2011;24: 89-91. Chinese. doi: http://dx.chinadoi.cn/10.3969/j.issn.1007-3256.2011.02.010
12. Yuan F, Chen GG, Zhang Q, Ding Y. [Effect of MECT combined with haloperidol injection in the acute phase of schizophrenia with irritability and agitation syndrome]. Yi Yao Qian Yan. 2012; 02: 227-228. Chinese
13. Peng CG, Wang GH, Zhang XF, Tu ZM, Cai DM, et al. [Effect of MECT combined with risperidone oral solution on irritability and agitation symptom during the acute phase of schizophrenia]. Jing Shen Yi Xue Za Zhi. 2014; 27: 427-429.Chinese
14. Li D. [A control study of clozapine combined with MECT for schizophrenia patients with irritability symptom]. Zhongguo Xian Dai Yao Wu Ying Yong. 2015; 9: 132-133. Chinese
15. Pan JZ. [Effect of MECT for agitation and irritability symptom in homelessness schizophrenia patients]. Yi Xue Li Lun Yu Shi Jian Za Zhi. 2015; 28: 2316-2317. Chinese
16. Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull.1987; 13: 261-276
17. Overall JE, Gorham DR. The Brief Psychiatric Rating-Scale.Psychological Reports. 1962; 10: 799-812
18. Higgins J, Higgins J. Cochrane Handbook for Systematic Reviews of Interventions. NY: John Wiley & Sons; 2008
19. DerSimonian R, Laird N. Meta-analysis in clinical trials.Control Clin Trials. 1986; 7: 177-188
20. Zheng W, Xiang YT, Xiang YQ, Li XB, Ungvari GS, Chiu HF, et al. Efficacy and safety of adjunctive topiramate for schizophrenia: a meta-analysis of randomized controlled trials. Acta Psychiatr Scand. 2016; 134(5): 385-398. doi:ht t p://dx.doi.org/10.1111/acps.12631
21. Egger M, Davey Smith G, Schneider M, Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315: 629-634.
22. Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ,Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996; 17(1): 1-12. doi: http://dx.doi.org/10.1016/0197-2456(95)00134-4
23. Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008; 336(7650): 924-926. doi:ht t p://dx.doi.org/10.1136/bmj.39489.470347.AD
24. Wang W, PU C, Jiang J, Cao X, Wang J, Zhao M, et al.Efficacy and safety of treating patients with refractory schizophrenia with antipsychotic medication and adjunctive electroconvulsive therapy: a systematic review and metaanalysis. Shanghai Arch Psychiatry. 2015; 27(4): 206-219.doi: ht t p://dx.doi.org/10.11919/j.issn.1002-0829.215093
25. Tharyan P, Adams CE. Electroconvulsive therapy for schizophrenia. Cochrane Database Syst Rev. 2005; 2:CD000076. doi: http://dx.doi.org/10.1002/14651858.CD000076
电休克治疗用于精神分裂症的激越症状:随机对照试验的meta分析
顾小静,郑伟,郭彤,Gabor S. Ungvari,Helen F.K. Chiu,操小兰,Carl D’Arcy,孟祥飞,宁玉萍,项玉涛
电休克治疗;躁动;精神分裂症;头痛,meta分析
Background: Agitation poses a significant challenge in the treatment of schizophrenia. Electroconvulsive therapy (ECT) is a fast, effective and safe treatment for a variety of psychiatric disorders, but no metaanalysis of ECT treatment for agitation in schizophrenia has yet been reported.
Aims: To systematically evaluate the efficacy and safety of ECT alone or ECT-antipsychotics (APs)combination for agitation in schizophrenia.
Methods:Systematic literature search of randomized controlled trials (RCTs) was performed. Two independent evaluators selected studies, extracted data about outcomes and safety with available data, conducted quality assessment and data synthesis. The Grades of Recommendation, Assessment,Development, and Evaluation (GRADE) was used to judge the level of the overall evidence of main outcomes.
Results: Seven RCTs from China, including ECT alone (4 RCTs with 5 treatment arms, n=240) and ECTAPs combination (3 RCTs, n=240), were identified. Participants in the studies were on average 34.3(4.5)years of age and lasted an average of 4.3(3.1) weeks of treatment duration. All 7 RCTs were non-blinded,and were rated as low quality based on Jadad scale. Meta-analysis of the pooled sample found no significant difference in the improvement of the agitation sub-score of the Positive and Negative Syndrome Scale (PANSS) when ECT alone (weighted mean difference=-0.90, (95% confidence interval (CI): -2.91,1.11), p=0.38) or ECT-APs combination (WMD=-1.34, (95%CI: -4.07, 1.39), p=0.33) compared with APs monotherapy. However, ECT alone was superior to APs monotherapy regarding PANSS total score (WMD=-7.13, I2=0%, p=0.004) and its excitement sub-score (WMD=-1.97, p<0.0001) as well as the PANSS total score at 14 days (WMD=-7.13, I2=0%, p=0.004) and its excitement sub-score at 7 and 14 days (WMD=-1.97 to -1.92, p=0.002 to 0.0001) after ECT. The ECT-APs combination was superior to APs monotherapy with respect to the PANSS total score at treatment endpoint (WMD=-10.40, p=0.03) and 7 days (WMD=-5.01, p=0.02). Headache ( number-needed-to-harm (NNH)=3, 95%CI=2-4) was more frequent in the ECT alone group compared to AP monotherapy. According to the GRADE approach, the evidence levels of main outcomes were rated as ‘very low’ (37.5%) and “low” (50%).
Conclusion:Pooling of the data based on 7 RCTs from China found no advantage of ECT alone or ECT-APs combination in the treatment of agitation related outcomes in schizophrenia patients. However, ECT alone or ECT-APs combination were associated with significant reduction in the PANSS total score. High-quality RCTs are needed to confirm the current interpretations.
Review registration number: CRD42014006689
http://dx.doi.org/111919/j.issn.1002-0829.217003]
1The Second Affiliated Hospital of Xinxiang Medical University, Henan Mental Hospital, Henan, China;
2Guangzhou Brain Hospital (Guangzhou Huiai Hospital), Affiliated Hospital of Guangzhou Medical University, Guangzhou China;
3The National Clinical Research Center for Mental Disorders & Beijing Anding Hospital, Capital Medical University, China;
4School of Psychiatry & Clinical Neurosciences, University of Western Australia, Perth, Australia;
5The University of Notre Dame Australia / Marian Centre, Perth, Australia;
6Department of Psychiatry, Chinese University of Hong Kong, Hong Kong SAR, China;
7Shenzhen Key Laboratory for Psychological Healthcare & Shenzhen Institute of Mental Health, Shenzhen Kangning Hospital & Shenzhen Mental Health Center, Shenzhen, China;
8Department of Psychiatry & School of Public Health, University of Saskatchewan, Saskatoon, Canada;
9Department of Psychiatry, McGill University and the Douglas Mental Health University Institute, Montreal, Canada;
10Unit of Psychiatry, Faculty of Health Sciences, University of Macau, Macao SAR, China;
#These authors equally contributed to the work.
*correspondence: Dr. Yu-Tao Xiang. Mailing address: 3/F, Building E12, Faculty of Health Sciences, University of Macau, Avenida da Universidade,Taipa, Macau SAR, China. E-mail: xyutly@gmail.com; Dr. Yu-Ping Ning. Mailing address: the Affiliated Brain Hospital of Guangzhou Medical University(Guangzhou Huiai Hospital), Guangzhou, China. E-mail: ningjeny@126.com
背景:躁动在精神分裂症治疗中是一个重大挑战。电休克疗法(ECT)对各种精神疾病是一种快速、有效、和安全的治疗,但ECT对精神分裂症的躁动治疗的相关meta分析还尚未报道。
目标:系统地评估单一使用ECT或ECT合并使用其他抗精神病药物(APs)的对精神分裂症的躁动治疗的有效性和安全性。
方法:进行随机对照试验(RCT)的系统文献搜索。两名独立评估者筛选研究、提取结果数据与现有数据的安全性、进行质量评估和数据合成。采用建议、评估、开发、和评价的工作组等级(GRADE)来判断主要成果的证据的总体水平。
结果:一共确定了中国有七个RCTs,包括ECT单一使用(4个RCTs有5个治疗组,n = 240)和ECT-APs合并使用(3个RCTs,n = 240)。研究对象平均年龄34.3(4.5)岁,平均治疗时间为4.3(3.1)周。所有7个RCTs非盲法,并且根据Jadad量表7项RCTs均被评为低质量。样本的Meta分析发现与APs单一治疗相比,单一使用ECT或ECT-APs合并使用阳性和阴性症状量表(PANSS)的躁动子因子评分改善均无显著性差异(ECT单一使用: weighted mean difference(WMD)=-0.90, 95% confidence interval (CI): (-2.91,1.11), p=0.38; ECT-APs合并使用:WMD=-1.34, (95%CI:-4.07, 1.39), p=0.33)。然而,PANSS总分(WMD=-7.13, I2=0%, p=0.004)和兴奋子因子评分(WMD=-1.97, p<0.0001)、ECT治疗14天后的PANSS总分(WMD=-7.13, I2=0%, p=0.004)和第7天和第14天的兴奋子因子评分(WMD=-1.97 to -1.92, p=0.002 to 0.0001)均显示单一使用ECT优于APs单一治疗。ECTAPs合并治疗结束时(WMD=-10.40, p=0.03)和治疗后7天(WMD=-5.01, p=0.02)的PANSS总分显示均优于APs单药治疗。头痛(p=0.0001, number-neededto-harm (NNH)=3, 95%CI=2-4)是唯一的ECT单一治疗后不良反应,并且ECT单一治疗组比APs单药治疗发生的更频繁。根据GRADE方法,主要结果的证据水平被评为“非常低”(37.5%)和“低”(50%)。
结论:基于中国7个RCTs合并的数据发现ECT单一治疗或ECT-APs合并治疗在精神分裂症患者的躁动治疗中并没有优势。然而,ECT单一治疗或ECT-APs合并治疗均与PANSS总分减低显著有关。需要高质量的RCTs验证目前的解释。

Xiao-jing Gu obtained a bachelor’s degree in 2009 and a master’s degree in psychiatry and mental health from the Capital Medical University in Beijing in 2012. Since then she has been working as a resident physician in the Second Affiliated Clinical College of Xinxiang Medical University, Henan Mental Hospital. Her research interests are depression and schizophrenia.

Wei Zheng obtained a bachelor’s degree from Hebei Medical University in 2012 and a master’s degree in psychiatry and mental health from the Capital Medical University in Beijing in 2015. Since then he has been working as a resident physician in the Department of Psychiatry in the Guangzhou Huiai Hospital. He is currently a PhD Candidate at the Affi liated Brain Hospital of Guangzhou Medical University (Guangzhou Huiai Hospital). His research interests are depression and schizophrenia.
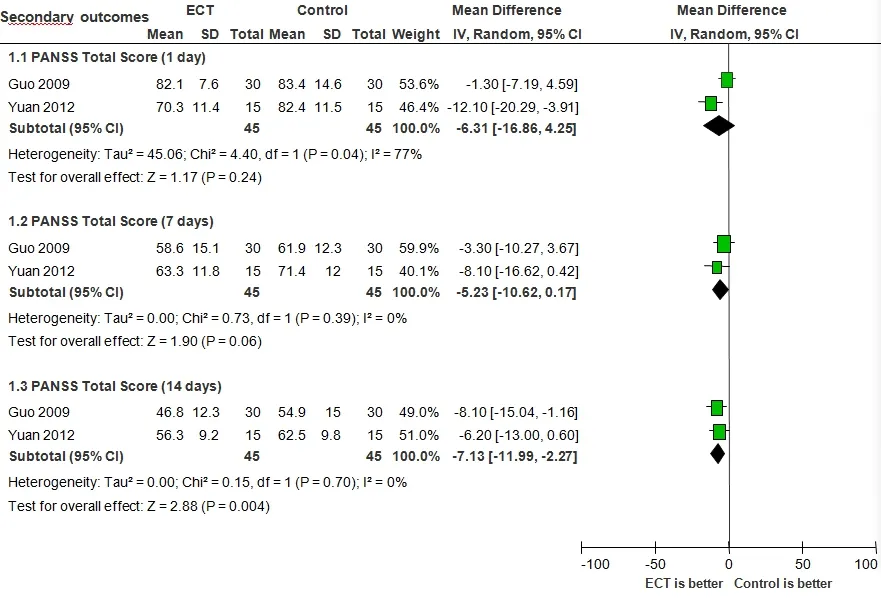
Supplemental Figure 1. ECT alone for agitation in schizophrenia: forest plot for the Positive and Negative Syndrome Scale (PANSS) total score at 1, 7, and 14 days
Notice for soliciting papers for the 14th academic conference of the Chinese Society of Neuroscience & Psychiatry (CSNP)
“The 14thannual academic conference of the Chinese Society of Neuroscience & Psychiatry”, which is hosted by CSNP, and undertaken by Mental Health Center of Shanghai Jiao Tong University’s medical school and Shandong Mental Health Center, will be held in the Luneng Hilton Hotel in Jinan, Shandong, from 29thJune to 1stJuly, 2017.
The present society welcomes paper submissions and conference participations. The conference affair group accepts abstracts (objectives, methods, results and conclusions) under 1000 words. The website used for paper submissions and registrations is http://61.147.124.137:8088/2017/default.aspx. The academic committee of this conference will review papers and select high quality reports for presentation at the conference. We look forward to your participation and support! The deadline for paper submission is 1stJune, 2017.
We welcome colleagues from all over China and abroad to participate in this conference held in scenic Jinan. We are looking forward to a lively discussion on developments in the field.
Dates: 29thJune to 1stJuly, 2017 (check in on 29thJune)
Address: Luneng Hilton Hotel in Jinan, Shandong, No.2888 South Erhuan Lu, Central District in Jinan
Cost arrangement: The registration fee, travel fee and accommodation fee are at your own expense. The registration fee is 1000 yuan (Shandong representatives and graduate students with student IDs can pay half of the registration fee). The accommodation fee from 30thJune to 1stJuly 2017 is 500 yuan per standard room.
Contact: Ruizhi Mao 18221768225
E-mail:csnpmeeting@163.com
Chinese Society of Neuroscience & Psychiatry 4thFebruary 2017
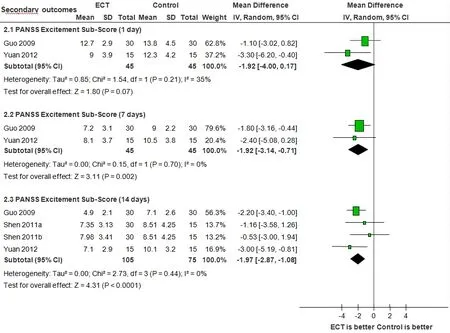
Supplemental Figure 2. ECT alone for agitation in schizophrenia: forest plot for the Positive and Negative Syndrome Scale (PANSS) excitement sub-score at 1, 7, and 14 days
Erratum
Li HB, Wang Y, Jiang J, Li W, Li CB. Effects of transcranial direct current stimulation (tDCS) for auditory hallucinations: A systematic review. Shanghai Arch Psychiatry. 2016; 28(6):301-308. doi: http://dx.doi.org/10.11919/j.issn.1002-0829.216121
In the Figure 1 (identification of included studies) of the paper, the number in the first box “304 potential articles published before 13 February 2016 were identified…” should be “432 potential articles published before 13 February 2016 were identified…”. This change was been made to the online version on the Shanghai Archives of Psychiatry website as of 10 Jan, 2017.
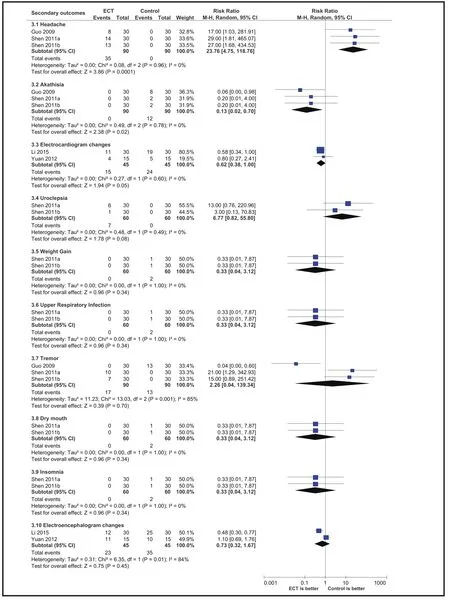
Supplemental Figure 3. ECT alone for agitation in schizophrenia: forest plot for adverse events
猜你喜欢
杂志排行
上海精神医学的其它文章
- The psychometric properties of the Quick Inventory of Depressive Symptomatology-Self-Report (QIDS-SR) in patients with HBV-related liver disease
- Relationship of mean platelet volume to MDD: a retrospective study
- Linking anger trait with somatization in low-grade college students: Moderating roles of family cohesion and adaptability
- Personality characteristics and neurocognitive functions in parents of children with Autism Spectrum Disorder
- The use of psychotropic drugs during pregnancy
- The Development of the Mind: A Three Month Old Infant
