直肠癌进展期应用3D腹腔镜行根治性手术的临床观察
2017-06-08区颖豪粱丽婷陈晓黄灿东
区颖豪 粱丽婷 陈晓 黄灿东
【摘要】 目的:探讨三维成像系统(3D)在腹腔镜下进展期直肠癌根治术中的应用价值和临床效果。方法:选取2015年2月-2016年10月本院收治的进展期直肠癌患者53例,按照随机数字表法分为对照组(n=26)与观察组(n=27)。对照组接受传统2D系统下腹腔镜直肠癌根治术,观察组则在3D成像系统下接受同样术式治疗。记录并对比两组术中情况(手术时间、术中出血量、淋巴结清扫数)、术后情况(排气时间、并发症发生率)和住院情况(住院时间、住院费用)。结果:观察组手术时间更短,术中出血量更少,淋巴结清扫数目更多(P<0.05)。在术后排气时间、并发症发生率、住院时间、住院费用等方面,两组比较差异均无统计学意义(P>0.05)。结论:对进展期直肠癌患者应用3D腹腔镜进行根治性手术治疗,能够缩短手术时间,减少术中出血量,并增加淋巴结清扫数目,与传统2D腹腔镜手术相比,有一定优势。
【关键词】 三维成像系统; 腹腔鏡; 直肠癌根治术; 进展期
Clinical Observation of Laparoscopic 3D Radical Operation for Advanced Rectal Cancer/OU Ying-hao,LIANG Li-ting,CHEN Xiao,et al.//Medical Innovation of China,2017,14(14):032-035
【Abstract】 Objective:To evaluate the clinical value of three-dimensional imaging system (3D) in laparoscopic radical resection of rectal cancer.Method:A total of 53 cases of advanced rectal cancer in our hospital from February 2015 to October 2016 were enrolled in the study and were divided into the control group(n=26) and the observation group(n=27).The control group was taken with laparoscopic radical resection of rectal cancer under traditional 2D system,while the observation group was taken with the same surgical treatment under the 3D imaging system.Intraoperation situation(operation time,intraoperative bleeding,lymph nodes),postoperative condition(exhaust time,complication rate) and hospitalization (hospitalization time,hospitalization expenses) of two groups were recorded and compared.Result:The observation group had shorter operation time,less blood loss and more lymph node dissection(P<0.05).However,there were no statistical significance in postoperative exhaust time,complication rate,hospital stay or hospitalization cost of the two groups(P>0.05).Conclusion:The application of 3D laparoscopic radical operation for patients with advanced rectal cancer can shorten the operation time,reduce the amount of intraoperative blood loss,increase the number of lymph node dissection,compared with traditional 2D laparoscopic surgery,there are certain advantages.
【Key words】 Three dimensional imaging system; Laparoscopy; Radical resection of rectal cancer; Advanced
First-authors address:The First Peoples Hospital of Zhaoqing,Zhaoqing 526040,China
doi:10.3969/j.issn.1674-4985.2017.14.009
腹腔镜技术在直肠癌根治术中已被广泛应用,其良好疗效和较高的安全性,得到专家学者的广泛认可[1-2]。但由于传统2D成像技术腹腔镜在操作过程中缺乏立体感,对于术中操作的纵深需根据术者丰富的临床经验判断,对术者要求较高[3]。新兴的3D腹腔镜技术可显著提升术野的空间分辨率和精确度,但目前国内鲜有将其应用于直肠癌根治术治疗的相关报道[4]。本研究选取2015年2月-2016年10月本院收治的进展期直肠癌患者53例,探讨3D成像技术在腹腔镜下进展期直肠癌根治术中的应用价值和临床效果结果满意,现报道如下。
1 资料与方法
1.1 一般资料 选取2015年2月-2016年10月本院收治的进展期直肠癌患者53例,其中男35例,女18例,年龄39~72岁,平均56.7岁。肿瘤直径>3 cm 37例,≤3 cm 16例,分化程度:低分化32例,中分化21例,无高分化患者。纳入标准:(1)术前经腹部影像学检查或结肠镜检查确诊为原发性进展期中低位直肠癌,术后病理学检查与之相符;(2)均接受2D或3D腹腔镜下直肠癌根治术(Dixon)治疗;(3)年龄范围20~80岁;(4)肿瘤未发生远处转移。排除标准:(1)既往有盆腔或腹腔手术史者;(2)合并其他脏器严重器质性病变者;(3)术中联合脏器切除或中转开腹者。所有患者按照随机数字表法分为对照组26例与观察组27例,两组患者一般资料比较差异均无统计学意义(P>0.05),具有可比性。该研究已经伦理学委员会批准,患者知情同意。
1.2 方法 对照组在传统2D系统下操作,观察组在3D系统下操作,所有患者手術操作均由本科同一组临床经验丰富的医师完成。具体手术过程为:患者取臀高头低截石位,依据无瘤原则和全肠系膜切除原则,使用五孔法将肠系膜下血管在根部离断,对周围脂肪和淋巴结进行清扫,使直肠充分游离[5]。使用腹腔镜下切开缝合器将直肠闭合,并在耻骨联合上方2 cm处做一横行切口,将肠管在肿瘤上缘10~15 cm处切断后,将购于美国强生公司的29#圆形吻合器钉座置入近端结肠,同时将断端切缘冰冻切片送病理检查,确认无癌细胞残留或缝合腹壁切口并重新建立气腹,整块切除侧方与上方淋巴结,并在腹腔镜直视下对结肠-肛管或结肠-直肠进行吻合,将肠管重新排列,术毕。
1.3 观察指标 记录并对比两组术中情况(手术时间、术中出血量、淋巴结清扫数)、术后情况(排气时间、并发症发生率)和住院情况(住院时间、住院费用)。其中,术后并发症主要包括吻合口瘘、吻合口出血、切口感染、切口疝、粘连性肠梗阻或输尿管损伤。
1.4 统计学处理 采用SPSS 16.0软件对所得数据进行统计分析,计量资料用(x±s)表示,比较采用t检验;计数资料以率(%)表示,比较采用 字2检验,以P<0.05为差异有统计学意义。
2 结果
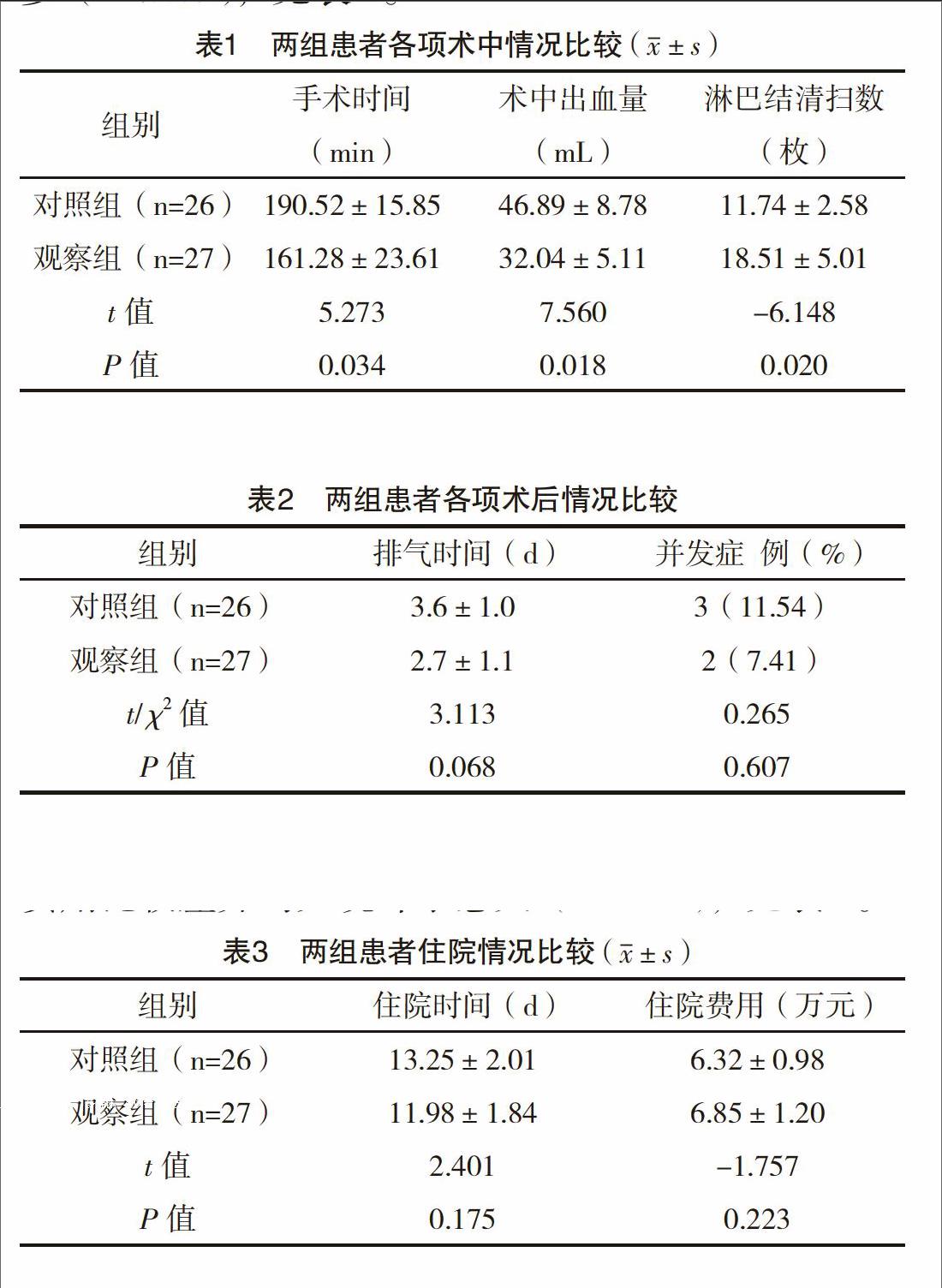
2.1 两组患者术中情况比较 两组患者接受不同成像系统下腹腔镜直肠癌根治术治疗期间,观察组手术时间更短,术中出血量更少,淋巴结清扫数目更多(P<0.05),见表1。
2.2 两组患者术后情况比较 接受不同成像系统下腹腔镜直肠癌根治术治疗后,两组排气时间比较差异无统计学意义(P>0.05)。此外,对照组发生吻合口出血1例,粘连性肠梗阻1例,切口感染1例,并发症发生率为11.54%,观察组发生切口感染2例,并发症发生率为7.41%,两组比较差异无统计学意义(P>0.05),见表2。
2.3 两组患者住院情况比较 两组住院时间和住院费用比较差异均无统计学意义(P>0.05),见表3。
3 讨论
微创外科时代的重要标志之一是腹腔镜的普及应用[3]。伴随腹腔镜技术的持续发展以及外科医生对腹腔镜技术的熟练掌握,其在直肠癌手术治疗中的安全性及疗效已被国内外专家学者广泛认可[6]。但传统的2D成像系统腹腔镜手术,由于无法帮助术者直观感受操作中的深度感和空间定位,立体感较差,需要外科医生进行大量、反复练习才可适应,对术者要求高,同时还增加了手术操作造成副损伤的风险,这也是传统腹腔镜手术术中出血甚至中转开腹的重要因素之一[7-9]。近年来新兴的3D成像技术,对腹腔镜手术术野的空间分辨率和精确度有极大改善,尤其在复杂手术操作中,能够显著提高精确解剖的操作水平,使解剖结构立体化、层次化,神经、血管走行更加清晰。有学者研究认为,3D腹腔镜技术术野较2D更接近双眼直视下所见,真实感更强,能使术者更快掌握腹腔镜的操作技术[10-11]。
本研究对观察组患者应用3D腹腔镜技术进行直肠癌根治术治疗,结果显示观察组手术操作时间和术中出血量均优于使用传统2D成像技术的对照组患者,这与国外学者的研究结果一致[12],提示3D腹腔镜操作体验更接近传统开腹手术,帮助术者获取较好的纵深感和立体感,而不只依靠经验对深度进行判断。这与3D腹腔镜下腹腔内各脏器解剖层次鲜明、术中定位精确有关[13-14]。3D腹腔镜操作过程中,术者与手术可在各自的操作领域进行更为默契的配合,大大减少手术操作时间和副损伤,降低术中出血量[15]。对于无法避免的术中出血,3D腹腔镜操作者也可凭借良好的术野对出血点进行迅速定位,并完成止血。同时,淋巴结的清扫也更直观,易于操作[16-17]。
在术后情况和住院情况方面,观察组与对照组比较差异均无统计学意义(P>0.05),提示3D腹腔镜技术在改善术中操作体验的同时,并未增加患者的住院时间和费用。还有学者研究认为,3D腹腔镜技术可通过缩短手术时间降低术中麻醉相关费用,减轻患者经济负担[18]。此外,还有报道称3D腹腔镜技术可降低术中周围脏器、血管、神经的损伤,使术后并发症发生率下降[19],但本研究中两组术中并发症发生率差异无统计学意义(P>0.05),这可能与本研究中手术操作医生熟练掌握腹腔镜的相关操作技术有关,也可能由于本研究样本量不多导致,有待于进一步研究。对于本研究中出现术后并发症的患者,并发症发现及时,症状较轻,均给予对症治疗后痊愈。
综上所述,对进展期直肠癌患者应用3D腹腔镜进行根治性手术治疗,能够缩短手术时间,减少术中出血量,增加淋巴结清扫数目,与传统2D腹腔镜手术相比,有一定优势。
参考文献
[1] Arezzo A,Passera R,Scozzari G,et al.Laparoscopy for rectal cancer reduces short-term mortality and morbidity:results of a systematic review and meta-analysis[J].International Journal of Colorectal Disease,2015,30(11):1457-1472.
[2] Xiong B,Ma L,Huang W,et al.Robotic versus laparoscopic total mesorectal excision for rectal cancer:a meta-analysis of eight studies[J].Journal of Gastrointestinal Surgery,2015,19(3):516-526.
[3] Arezzo A,Passera R,Salvai A,et al.Laparoscopy for rectal cancer is oncologically adequate:a systematic review and meta-analysis of the literature[J].Surgical Endoscopy,2015,29(2):334-348.
[4] Arbea L,Ramos L I,Moreno M,et al.Intensity-modulated radiation therapy (IMRT) vs. 3D conformal radiotherapy (3DCRT) in locally advanced rectal cancer (LARC):dosimetric comparison and clinical implications[J].Radiation Oncology,2010,5(1):17.
[5] Alberda W J,Verhoef C,Schipper M E,et al.The Importance of a Minimal Tumor-Free Resection Margin in Locally Recurrent Rectal Cancer[J].Annals of Oncology,2015,58(7):677-685.
[6] Morino M,Risio M,Bach S,et al.Early rectal cancer:the European Association for Endoscopic Surgery (EAES) clinical consensus conference[J].Surgical Endoscopy,2015,29(4):755-773.
[7] ?zsoy M,Kallidonis P,Kyriazis I,et al.Novice surgeons:do they benefit from 3D laparoscopy[J].Lasers in Medical Science,2015,30(4):1-9.
[8] Feng X,Morandi A,Boehne M,et al.3-Dimensional (3D) laparoscopy improves operating time in small spaces without impact on hemodynamics and psychomental stress parameters of the surgeon[J].Surgical Endoscopy,2015,29(5):1231-1239.
[9] Dongliang X U,Tan M,Yi H E,et al.Three-port laparoscopic radical prostatectomy:comparison of three dimensional (3D) versus two-dimensional (2D) laparoscopy[J].Chinese Journal of Surgical Oncology,2016,4(5):54-56.
[10] Schoenthaler M,Schnell D,Wilhelm K,et al.Stereoscopic (3D) versus monoscopic (2D) laparoscopy:comparative study of performance using advanced HD optical systems in a surgical simulator model[J].World Journal of Urology,2016,34(4):471-477.
[11] Shakir F,Jan H,Kent A.3D straight-stick laparoscopy versus 3D robotics for task performance in novice surgeons:a randomised crossover trial[J].Surgical Endoscopy,2016,30(12):5380-5387.
[12] Baum S,Sillem M,Ney J,et al.What Are the Advantages of 3D Cameras in Gynaecological Laparoscopy[J].Geburtshilfe Frauenheilkd,2017,77(1):45-51.
[13] Abouhaidar H,Alqaoud T,Jednak R,et al.Laparoscopic pyeloplasty:Initial experience with 3D vision laparoscopy and articulating shears[J].Journal of Pediatric Urology,2016,12(6):121-126.
[14] Sinha R,Battina S.3D Laparoscopy:An Analysis of 1,475 Cases[J].Journal of Minimally Invasive Gynecology,2016,23(7):S55.
[15] Wei-Min L I,Wang F,Yan-Qin Y U.Application of 3D laparoscopy in gynecological operation for uterine fibroid[J].Journal of Laparoscopic Surgery,2016,4(12):94-101.
[16] Huang Z,Ding Y,Chaohui G U,et al.Comparison of efficacy between 3D laparoscopy and conventional laparoscopy in nephron-sparing surgery for renal cell carcinoma[J].Journal of Clinical Urology,2016,3(7):3-9.
[17] Fang C,Fang Z,Fan Y,et al.Application of 3D visualization,3D printing and 3D laparoscopy in the diagnosis and surgical treatment of hepatic tumors[J].Journal of Southern Medical University,2015,35(5):639.
[18] Gingu C,Dick A,Baston C,et al.The advantages of 3D HD laparoscopy over the standard 2D vision[J].European Urology Supplements,2016,15(11):e1414.
[19] Raspagliesi F,Bogani G,Martinelli F,et al.Incorporating 3D laparoscopy for the management of locally advanced cervical cancer:a comparison with open surgery[J].Tumori,2016,102(4):393-397.
(收稿日期:2017-03-14) (本文編辑:周亚杰)
