血清基质细胞衍生因子—1水平对阿卡波糖治疗初发2型糖尿病效果的影响
2017-05-11甘美舍周凤燕郑程何明杰
甘美舍+周凤燕+郑程+何明杰

[摘要] 目的 探討血清基质细胞衍生因子-1(SDF-1)水平对阿卡波糖治疗初发2型糖尿病效果的影响。 方法 选取2013年6月~2015年12月广西壮族自治区百色市人民医院内分泌科收治的初发2型糖尿病患者64例为研究对象。所有患者均予以口服阿卡波糖50 mg,每日3次,疗程持续6个月。采用酶联免疫吸附试验测定患者治疗前SDF-1水平,并以中位数155.86 pg/mL为分界值,将患者分为高SDF-1组(21例)和低SDF-1组(43例),比较不同SDF-1水平对阿卡波糖治疗初发2型糖尿病临床效果的影响。 结果 低SDF-1组的总有效率为97.67%,显著高于高SDF-1组的80.95%,差异有统计学意义(P < 0.05)。低SDF-1组空腹血糖和餐后2 h血糖均明显低于高SDF-1组,差异有统计学意义(P < 0.05)。两组肌酐、尿素氮比较,差异无统计学意义(P > 0.05)。 结论 低水平SDF-1的初发2型糖尿病患者予以阿卡波糖治疗的临床效果更为良好。
[关键词] 基质细胞衍生因子-1;阿卡波糖;初发2型糖尿病;临床疗效
[中图分类号] R587.1 [文献标识码] A [文章编号] 1673-7210(2017)03(c)-0059-03
Effect of serum stromal cell derived factor -1 level on the clinical efficacy of Acarbose in the treatment of newly diagnosed type 2 diabetes
GAN Meishe1 ZHOU Fengyan1 ZHENG Cheng2 HE Mingjie3
1.Department of Endocrinology, People's Hospital of Baise City, Guangxi Zhuang Autonomous Region, Baise 533000, China; 2.Department of Andriatry, the First Affiliated Hospital of Guangxi Medical University, Guangxi Zhuang Autonomous Region, Nanning 530021, China; 3.Department of Endocrinology, Affiliated Hospital of Youjiang Medical Universtiy for Nationalities, Guangxi Zhuang Autonomous Region, Baise 533000, China
[Abstract] Objective To explore the effect of serum stromal cell derived factor-1 (SDF-1) level on the clinical efficacy of acarbose in the treatment of newly diagnosed type 2 diabetes. Methods 64 cases of newly diagnosed type 2 diabetes from June 2013 to December 2015 in Department of Endocrinology, People's Hospital of Baise City, Guangxi Zhuang Autonomous Region were selected as study subjects. All patients were given 50 mg Acarbose, 3 times a day and lasted for 6 months. Enzyme linked immunosorbent assay was used to measure the level of SDF-1 before treatment, and the median 155.86 pg/mL was used as the cut-off value. The patients were further divided into high SDF-1 group (21 cases) and low SDF-1 group (43 cases). The effects of SDF-1 levels on clinical efficacy of Acarbose in the treatment of type 2 diabetes were compared. Results Total effective rate in low SDF-1 group was 97.67%, significantly higher than that in high SDF-1 group (80.95%) (P < 0.05). Fasting blood glucose and 2 h postprandial blood glucose in lower SDF-1 group were significantly lower than those in high SDF-1 group (P < 0.05). There was no significant difference in serum creatinine and urea nitrogen between two groups (P > 0.05). Conclusion Clinical efficacy of Acarbose is much better in the newly diagnosed type 2 diabetic patients with low level of SDF-1.
[Key words] Stromal cell derived factor-1; Acarbose; Newly diagnosed type 2 diabetes; Clinical efficacy
全球2型糖尿病患者总数已超过1.77亿例,其中我国的发病数高居第三位[1-2]。阿卡波糖是一种新型口服降糖药,具有显著抑制餐后血糖的作用[3-5]。基质细胞衍生因子-1(SDF-1)是一种新发现的趋化因子,被发现与糖尿病的多种并发症紧密相关[6]。然而,SDF-1水平是否影响阿卡波糖对初发2型糖尿病的治疗效果目前尚不清楚。故本研究拟以初发2型糖尿病患者为研究对象,探讨SDF-1水平对初发2型糖尿病临床疗效的影响。
1 资料与方法
1.1 一般资料
选取2013年6月~2015年12月于广西壮族自治区百色市人民医院内分泌科诊治的64例初发2型糖尿病患者为研究对象。其中男38例,女26例,年龄41~70岁,平均(53.61±5.83)岁。纳入标准:①所有患者均符合1999年世界卫生组织制订的糖尿病诊断标准[7],且初次诊断2型糖尿病;②心、肺、肝、肾功能均无明显异常,糖化血红蛋白(HbA1c)基线值为7.5%~9.0%;体质指数在20~24 kg/m2;③依从性好,愿意按时服药及复诊;④近8周内血压控制平稳,饮食、运动较规律,且无影响精神或情绪的重大生活事件发生。排除标准:①1型糖尿病患者或合并糖尿病急性并发症;②伴有严重感染,罹患呼吸、消化、循环系统基础疾病或有精神障碍、神经疾病者;③妊娠或哺乳期女性;④治疗过程中不参照规定服药,自行服用其他降糖药物或调整用药剂量;⑤治疗过程中失访者;⑥对阿卡波糖使用有禁忌证者。研究方案经医院伦理委员会批准,所有患者及其家属均签署知情同意书。
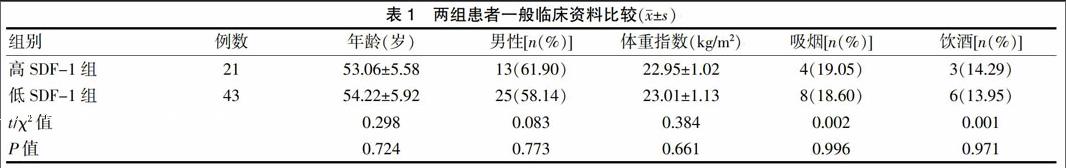
所有患者血清SDF-1水平范围114.19~324.52 pg/mL,平均(194.54±62.81)pg/mL。以SDF-1测定中位数155.86 pg/mL为分界值,将患者分为高SDF-1组(21例)和低SDF-1组(43例)。两组患者一般临床资料比较,差异无统计学意义(P > 0.05),具有可比性。见表1。
1.2 治疗方法
所有患者均予以口服阿卡波糖(华东医药股份有限公司制造分公司,生产批号132402)50 mg,每日3次;服药期间每2周检测一次空腹血糖值和餐后血糖;每8周测定1次HbA1c的变化量,疗程持续6个月。
1.3 疗效评估
所有患者临床总体疗效依据HbA1c水平[8]判定,①显效:HbA1c下降≥1%;②有效:HbA1c下降0.3%~1%;③无效:HbA1c下降<0.3%。总有效=显效+有效。观察患者血糖(空腹血糖、餐后2 h血糖)、肌酐、尿素氮水平。
1.4 SDF-1水平检测
治疗前采集患者清晨空腹静脉血液,采用酶联免疫吸附试验测定血清SDF-1的变化水平,试剂盒购自于上海研卉生物科技有限公司,产品编号P90122 Hu01,检测过程由专业检验人员严格按照说明书操作完成。
1.5 统计学方法
采用SPSS 18.0统计软件对数据进行分析和处理,计量资料以均数±标准差(x±s)表示,采用独立样本Student-t检验,计数资料采用χ2检验,以P < 0.05为差异有统计学意义。
2 结果
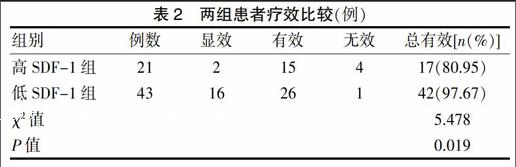
2.1 两组患者疗效比较
低SDF-1组总有效率高于高SDF-1组,差异有统计学意义(P < 0.05)。见表2。
2.2 两组患者血糖、肌酐和尿素氮水平比较
低SDF-1组空腹血糖和餐后2 h血糖均明显低于高SDF-1组(P < 0.05);两组肌酐、尿素氮比较,差异无统计学意义(P > 0.05)。见表3。
表3 两组患者血糖、肌酐和尿素氮水平比较(x±s)
3 讨论
2型糖尿病在我国是仅次于恶性肿瘤和心血管疾病后的第三大死因[9-10]。当前,多数2型糖尿病患者主要采用双胍类、α糖苷酶抑制剂、磺酰脲类、胰岛素增敏剂等药物进行治疗[11-13]。其中,阿卡波糖就是一种新型的α糖苷酶抑制剂,能够降低空腹血糖、餐后血糖和HbA1c水平[14-15]。本研究结果显示,经阿卡波糖治疗后,两组患者仅5例無效,治疗总体有效率达92.18%,与既往报道结论基本一致[16]。同时,在治疗过程中,患者均未出现明显的药物不良反应症状,充分提示阿卡波糖对2型糖尿病具有良好的临床疗效且安全性良好。
SDF-1是一种由骨髓基质细胞释放的新型细胞趋化因子[17]。目前已有众多研究显示,SDF-1可广泛参与新生血管形成、慢性炎症和氧化应激等多种病理生理过程[18-19]。而且,研究发现,SDF-1水平还与糖尿病的发生、发展以及并发症紧密相关[20-21],提示SDF-1可能参与调节糖尿病的形成和预后。本研究以血清SDF-1的中位数为临界值,将患者分为高、低SDF-1组,结果显示,低SDF-1组患者的总体有效率为97.67%,显著高于高SDF-1组的80.95%,表明SDF-1水平越低,阿卡波糖对2型糖尿病患者的疗效越佳。研究结果还发现,阿卡波糖良好的临床效果并不受年龄、性别、体重指数、是否吸烟和饮酒等因素的影响,提示SDF-1具有指示阿卡波糖治疗2型糖尿病临床疗效的潜在作用。本研究还进一步观察了不同SDF-1水平对空腹血糖、餐后2 h血糖、肌酐和尿素氮水平的影响,结果显示,低SDF-1组患者的空腹血糖和餐后2 h血糖值均明显低于高SDF-1组,充分证实了阿卡波糖的疗效。但研究结果却发现,SDF-1水平对肌酐和尿素氮的水平无显著影响,这可能与SDF-1主要作用靶点在肠道而对肾脏功能并无明显干预效应有关[22]。
綜上所述,低水平SDF-1的初发2型糖尿病患者予以阿卡波糖治疗的效果更为良好。但由于研究纳入的样本量有限,观察周期较短,且未考虑其他使用药物对阿卡波糖疗效的影响,故研究结论仍有一定的局限性,亟待后续多中心临床试验或基础研究加以论证。
[参考文献]
[1] Group IDFGD. Global guideline for type 2 diabetes-diabetes research and clinical practice [J]. Diabetes Res Clin Pr,2014,104(1):1-52.
[2] Association AD. The prevention or delay of type 2 diabetes [J]. Diabetes Care,2015,38(Suppl 1):742-749.
[3] Yang W,Liu J,Shan Z,et al. Acarbose compared with metformin as initial therapy in patients with newly diagnosed type 2 diabetes:an open-label,non-inferiority randomised trial [J]. Lancet Diabetes Endo,2014,2(1):46-55.
[4] 牟敏.阿卡波糖、二甲双胍联合胰岛素类似物治疗肥胖2型糖尿病的短期效果分析[J].中国当代医药,2015,22(22):112-114.
[5] 高红彦.阿卡波糖干预治疗糖耐量异常的临床效果[J].中国当代医药,2016,23(4):120-122.
[6] Derakhshan R,Arababadi MK,Ahmadi Z,et al. Increased circulating levels of SDF-1(CXCL12)in type 2 diabetic patients are correlated to disease state but are unrelated to polymorphism of the SDF-1β gene in the Iranian population [J]. Inflammation,2012,35(3):900-904.
[7] Gabir MM,Hanson RL,Dabelea D,et al. The 1997 American Diabetes Association and 1999 World Health Organization criteria for hyperglycemia in the diagnosis and prediction of diabetes [J]. Diabetes Care,2000,23(8):1108-1112.
[8] D′Emden MC,Shaw JE,Jones GR,et al. Use of glycated haemoglobin(HbA1c)in the diagnosis of diabetes mellitus [J]. Med J Australi,2015,203(2):89-90.
[9] Xu Y,Wang L,He J,et al. Prevalence and control of diabetes in Chinese adults [J]. JAMA,2013,310(9):948-959.
[10] Li MZ,Su L,Liang BY,et al. Trends in prevalence,awareness,treatment,and control of diabetes mellitus in mainland china from 1979 to 2012 [J]. Int J Endo,2013,2013(4):753150.
[11] Asche C,Lafleur J,Conner C. A review of diabetes treatment adherence and the association with clinical and economic outcomes [J]. Clin Ther,2011,33(1):74-109.
[12] Ratner RE,Sathasivam A. Treatment recommendations for prediabetes [J]. Med Clin N Am,2011,95(2):385-395.
[13] Pratley RE. The early treatment of type 2 diabetes [J]. Am J Med,2013,126(9):2-9.
[14] Wang JS,Huang CN,Hung YJ,et al. Acarbose plus metformin fixed-dose combination outperforms acarbose monotherapy for type 2 diabetes [J]. Diabetes Res Clin Pr,2013,102(1):16-24.
[15] Hanefeld M,Schaper F. Acarbose:oral antidiabetes drug with additional cardiovascular benefits [J]. Exp Rev Cardiovasc Ther,2014,6(2):153-163.
[16] Hu R,Li Y,Lv Q,et al. Acarbose monotherapy and type 2 diabetes prevention in eastern and western prediabetes:an ethnicity-specific Meta-analysis [J]. Clin Ther,2015,37(8):1798-1812.
[17] Yousry S,Shahin G,Demerdash DE,et al. SDF-1(CXCL12)polymorphisms in Egyptian patients with systemic lupus erythematosus(SLE):a pilot study [J]. Comp Clin Pathol,2015,24(6):1535-1540.
[18] Cai Y,Li X,Wang YS,et al. Hyperglycemia promotes vasculogenesis in choroidal neovascularization in diabetic mice by stimulating VEGF and SDF-1 expression in retinal pigment epithelial cells [J]. Exp Eye Res,2014, 123(4):87-96.
[19] Olekson MA,Faulknor R,Bandekar A,et al. SDF-1 liposomes promote sustained cell proliferation in mouse diabetic wounds [J]. Wound Repair Regen,2015,23(5):711-723.
[20] Fadini GP,Albiero M,Seeger F,et al. Stem cell compartmentalization in diabetes and high cardiovascular risk reveals the role of DPP-4 in diabetic stem cell mobilopathy [J]. Basic Res Cardiol,2013,108(1):1164.
[21] Zhao Y,Tan Y,Xi S,et al. A novel mechanism by which SDF-1β protects cardiac cells from palmitate-induced endoplasmic reticulum stress and apoptosis via CXCR7 and AMPK/p38 MAPK-mediated interleukin-6 generation [J]. Diabetes,2013,62(7):2545.
[22] Connelly KA,Advani A,Zhang Y,et al. DPP-4 inhibition improves cardiac function in experimental myocardial infarction:role of SDF-1 alpha [J]. J Diabetes,2015,8(1):1-8.
(收稿日期:2016-12-16 本文編辑:李亚聪)
