Clinical characteristics of childhood cancer in emergency room in a tertiary hospital in Pakistan
2016-11-23AmnaJawaidKhubaibArifNickBrownZehraFadoo
Amna Jawaid, Khubaib Arif, Nick Brown, Zehra Fadoo
1Department of Emergency Medicine, Aga Khan University Hospital, Karac hi 74800, Pakistan
2Visiting faculty, Salisbury District Hospital, Salisbury, United Kingdom
3Department of Oncology and Pediatrics, Aga Khan University Hospital, Karac hi 74800, Pakistan
Corresponding Author: Amna Jawaid, Email: Jawaid.amna@gmail.com; amna.jawaid@aku.edu
Clinical characteristics of childhood cancer in emergency room in a tertiary hospital in Pakistan
Amna Jawaid1, Khubaib Arif1, Nick Brown2, Zehra Fadoo3
1Department of Emergency Medicine, Aga Khan University Hospital, Karac hi 74800, Pakistan
2Visiting faculty, Salisbury District Hospital, Salisbury, United Kingdom
3Department of Oncology and Pediatrics, Aga Khan University Hospital, Karac hi 74800, Pakistan
Corresponding Author: Amna Jawaid, Email: Jawaid.amna@gmail.com; amna.jawaid@aku.edu
World J Emerg Med 2016;7(4):300–302
INTRODUCTION
Worldwide, cancer is an important cause of mortality in children aged over 1 year.[1]Numerically, the major cancers include acute lymphoblastic leukemia, CNS tumors and lymphomas.[2–6]Cancer incidence is increasing in children globally as well as in Pakistan but the etiology is poorly understood.[7]There are an estimated 160 000 new cases and 90 000 deaths per year worldwide in children aged under 15 years.[8]The exact incidence in Pakistan is not known as there is no national tumor registry.
Early diagnosis in childhood is vital in terms of outcome.[9–14]However, presentations are non-specific which may lead to a delay in both diagnosis and treatment and a poorer outcome.[15–17]
Knowledge of common presentation and initial management of oncological emergencies is, therefore, essential for the emergency department (ED) care provider. Common oncological emergencies with which the emergency physician might encounter include tumor lysis syndrome, coagulopathy, hyperleukocytosis, mediastinal mass with airway obstruction and spinal cord compression all of which have substantial morbidity and mortality if left untreated. There is no previous data available on frequency and clinical presentations of childhood cancer in the emergency room from Pakistan, so our goal was to identify the presentation of childhood malignancy in ED.
METHODS
The Aga Khan University Hospital is a 600-bedded tertiary-care teaching hospital serving a population of approximately 20 million. It has sub-specialists in all the major pediatric specialties.
A retrospective, chart review of patients presenting to the AKUH ED between January 2009 and December 2013 was undertaken. After approval from ethical review committee, data was retrieved through medical record and composed of six components: demographic, presenting symptoms, examination findings, laboratory investigation, diagnosis and outcome.
Data was collected on a proforma and transferred into SPSS for analysis. Percentages and frequency were used for descriptive statistics and mean (SD) and median (IQR) estimated for normally and non-normally distributed continuous variables respectively.
RESULTS
Over the 5 years period, 81 151 children were assessed in the ED. Of these, 59% were male and 41% female. A malignancy was diagnosed in 154, a rate of 1.9/1 000. The median age at presentation was 5.6 years (IQR 2.6–10). There were more boys (76, 62.3%), and common symptoms observed in the patients were fever (76.6%), weight loss (40.3%), pallor (38.3%) and petechial rash (24.7%). Childhood leukemia was the most common malignancy diagnosed with B-Cell ALL being the most common subtype. This was followed by CNS tumors with medulloblastoma being the most common. The median time between admission to the pediatric ward was 6 days (IQR 5–9 days) with a range of 3 to 25 days. Fever, weight loss and rash were the most common symptoms in children with leukemia. Headachewas the most frequent presentation of intracranial tumors whereas abdominal mass was the main fi nding in children with renal tumor and neuroblastoma (Table 1). Hepatomegaly was found in 66%, splenomegaly in 46% and lymphadenopathy in 51% of children with leukemia and lymphoma.
Laboratory data also revealed average hemoglobin of 8.76±2.79 with minimum of 3.4 g/dL. Hyperleukocytosis was present in 26 (16.9%) children with the lowest total leukocyte count (TLC) of 0.7×109/L and highest being 459×109/L (Table 2).
Relevant radiological imaging was conducted on all children seeking emergency care depending on the presenting complaints. Mediastinal mass was detected in 6.6% of patients with leukemia and 9% of children with lymphoma. All children suspected of having space occupying lesion (SOL) had evidence of intracranial tumor on CT head.
Leukemia was the most common in children less than 5 years of age. CNS tumors predominated in children between 5–10 years and lymphoma in those aged 10 years. The most common acute complication encountered was hyperleukocytosis 26 (16.88%), bleeding 25 (16.23%), breathing difficulty 24 (15.58%) with 6 (3.89%) requiring ventilator support and seizure 10 (6.49%). Shock was seen in 7 (4.54%), coma in 6 (3.89%), and cardiac failure secondary to anemia in 5 (3.24%) patients. From the ED, 73% were admitted to a ward and 24% to pediatric intensive care. Despite explanation, 3% of families were self-discharged. In terms of long-term outcome, 70 (47%) survived, 33 (22%) died at AKUH. Of the others, 41 (28%) were referred to other health care facility after starting treatment and 6 (4%) patients left against medical advice because of fi nancial reasons.
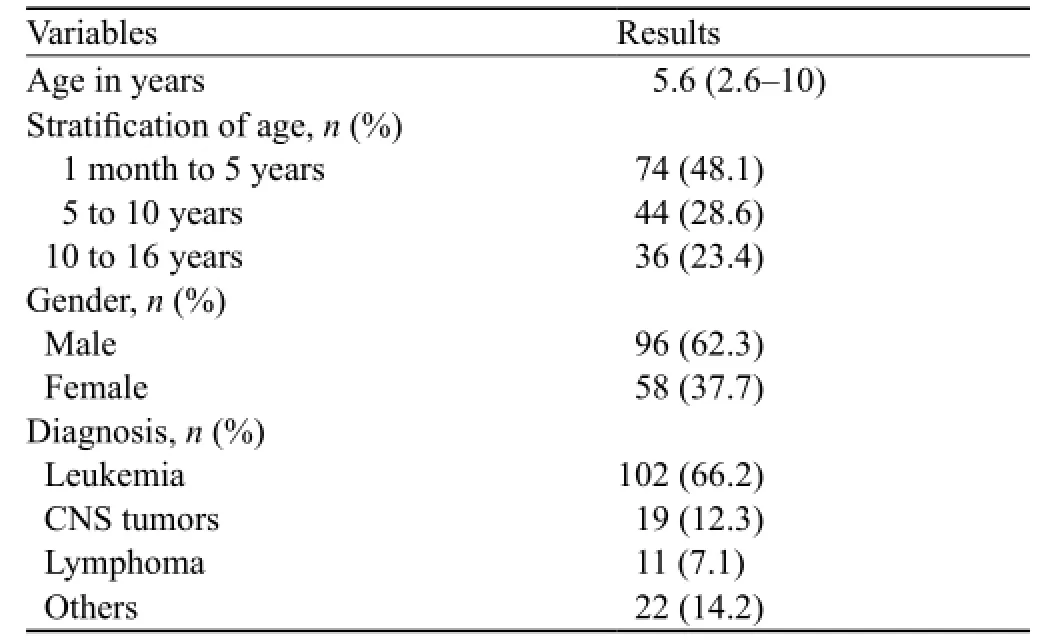
Table 1. Demographics
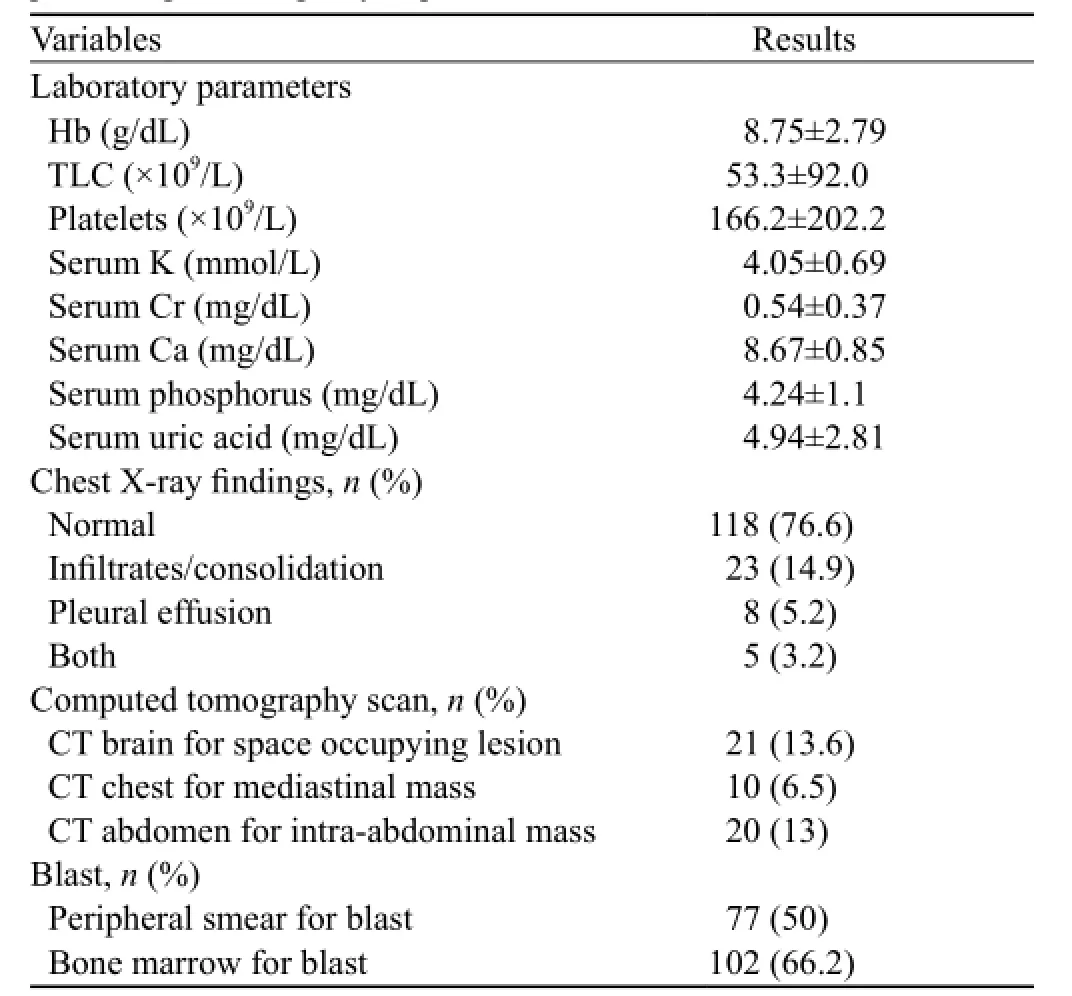
Table 2. Laboratory parameters of suspected oncology patients presenting to emergency department
DISCUSSION
It is estimated that about 150 cases per one million are diagnosed annually with cancer worldwide.[18–19]The exact incidence of childhood cancer remains unknown in Pakistan owing to the absence of a National Cancer Registry, though available data estimates that 600 children per year are diagnosed[9]representing 11% of the total number of new diagnoses.[20]This is almost certainly an underestimate of the reality as a result of the lack of diagnostic facilities in many parts of the country.
There is little previous literature from lower-middleincome countries (LMICs) but some from high income countries. Jaffe et al[21]in a study from Philadelphia reported cancer detection as 1 per 4 500 ED visits. Xing et al[22]and Haase et al[23]reported 22.8 cases of cancer being diagnosed per 100 000 children in pediatric ED from Michigan. These rates are much lower than ours suggesting that in high-income countries, children with cancer enter their respective health systems through different routes. In Pakistan, the ED is the main portal of entry to acute secondary care, which reinforces the need for vigilance and training emergency physicians.
The importance of history and physical examination is highlighted in this study and there is a good case for including a check list of relevant clinical signs on the standard ED admission form including: lymphadenopathy, hepatosplenomegaly, weight loss, oral ulcers of candida, and bruising. In children withany of these signs, consideration of laboratory workup, especially complete blood count, film, chemistry, LDH and chest X-ray is important and an algorithm to guide investigation could help ED juniors.
In conclusion, in Pakistan, children with cancer often make their initial presentation to the ED. Delay in diagnosis can be disastrous and we have identified a number of warning signs of potential use to emergency doctors to enable this window of diagnostic opportunity to be seized.
ACKNOWLEDGEMENTS
I thank almighty Allah, the most Merciful, for blessing me with the opportunity of carrying out and completing this study successfully.
Funding: None.
Ethical approval: The study was approved by ethical review committee.
Conflicts of interest: The authors declare there is no competing interest related to the study, authors, other individuals or organizations.
Contributors: Jawaid A proposed the study and wrote the first draft. All authors read and approved the fi nal version of the paper.
REFERENCES
1 Teo WY, Chan MY, Ng KC, Tan AM. Bony presentations of childhood haematological malignancy to the emergency room. J Paediatr Child Health 2012; 48: 311–316.
2 Hussain M, Khattak TAK, Bano Q. Spectrum of hematological disorders in children observed in 424 consecutive bone marrow aspirations/biopsies. Pak J Med Sci 2005; 21: 433–436.
3 Nazemi KJ, Malempati S. Emergency department presentation of childhood cancer. Emerg Med Clin North Am 2009; 27: 477–495.
4 Khalid S, Moiz B, Adil SN, Khurshid M. Retrospective review of pediatric patients with acute lymphoblastic leukemia: a single center experience. Indian J Pathol Microbiol 2010; 53: 704–710.
5 Yasmeen N, Ashraf S. Childhood acute lymphoblastic leukaemia; epidemiology and clinicopathological features. J Pak Med Assoc 2009; 59: 150–153.
6 Fadoo Z, Nisar I, Yousuf F, Lakhani LS, Ashraf S, Imam U, et al. Clinical features and induction outcome of childhood acute lymphoblastic leukemia in a lower/middle income population: A multi-institutional report from Pakistan. Pediatr Blood Cancer 2015; 62: 1700–1708.
7 Kadan-Lottick NS. Epidemiology of childhood and adolescent cancer. Nelson Textbook of Pediatrics 18th ed Philadelphia, Pa: Saunders Elsevier 2007: 2097.
8 Globocan I, Ferlay J, Bray F, Pisani P, Parkin D. Cancer incidence, mortality and prevalence worldwide. IARC Press GLOBOCAN. 2000; 2001.
9 Aburn G, Gott M. Educatin given to parents of children newly diagnosed with acute lymphoblastic leukemia: the parent's perspective. Pediatr Nurs 2014; 40: 243–248, 256.
10 Jamal S, Mamoon N, Mushtaq S, Luqman M. Pattern of childhood malignancies: study of 922 cases at Armed Forces Institute of Pathology (AFIP), Rawalpindi, Pakistan. Asian Pac J Cancer Prev 2006; 7: 420–422.
11 Shahab F, Raziq F. Clinical presentations of acute leukemia. J Coll Physicians Surg Pak 2014; 24: 472–476.
12 Meert AP. Oncological emergencies. Rev Mal Respir 2008; 25 (8 Pt 2): 3S145–50.
13 Brown BJ, Ajayi SO, Ogun OA, Oladokun RE. Factors influencing time to diagnosis of childhood cancer in Ibadan, Nigeria. Afr Health Sci 2009; 9: 247–253.
14 Haut C. Oncological emergencies in the pediatric intensive care unit. AACN Clin Issues 2005; 16: 232–245.
15 Brasme JF, Morfouace M, Grill J, Martinot A, Amalberti R, Bons-Letouzey C, et al. Delays in diagnosis of paediatric cancers: a systematic review and comparison with expert testimony in lawsuits. Lancet Oncol 2012; 13: e445–459.
16 Shandro J, Sohoni A. A practical guide to pediatric emergency medicine: caring for children in the emergency department: Cambridge University Press; 2011.
17 Zonfrillo MR. Management of pediatric tumor lysis syndrome in the emergency department. Emerg Med Clin North Am 2009; 27: 497–504.
18 Fragkandrea I, Nixon JA, Panagopoulou P. Signs and symptoms of childhood cancer: a guide for early recognition. Am Fam Physician 2013; 88: 185–192.
18 Prusakowski MK, Cannone D. Pediatric oncologic emergencies. Emerg Med Clin North Am 2014; 32: 527–548.
19 Young G, Toretsky JA, Campbell AB, Eskenazi AE. Recognition of common childhood malignancies. Am Fam Physician 2000; 61: 2144–2154.
20 States LJ, Meyer JS. Imaging modalities in pediatric oncology. Radiol Clin North Am 2011; 49: 579–588.
21 Jaffe D, Fleisher G, Grosflom J. Detection of cancer in the pediatric emergency department. Pediatr Emerg Care 1985; 1: 11–15.
22 Xing XZ, Gao Y, Wang HJ, Yang QH, Huang CL, Qu SN, et al. Risk factors and prognosis of critically ill cancer patients with postoperative acute respiratory insufficiency. World J Emerg Med 2013; 4: 43–47.
23 Haase R, Merkel N, Diwan O, Elsner K, Kramm CM. Leukapheresis and exchange transfusion in children with acute leukemia and hyperleukocytosis. A single center experience. Klin Padiatr 2009; 221: 374–378.
Accepted after revision July 18, 2016
10.5847/wjem.j.1920–8642.2016.04.011
Letter to the editor
January 9, 2016
杂志排行
World journal of emergency medicine的其它文章
- The state and future of emergency medicine in Macedonia
- Amiodaron in atrial fi brillation: post coronary artery bypass graft
- Short lessons in basic life support improve self-assurance in performing cardiopulmonary resuscitation
- Is current training in basic and advanced cardiac life support (BLS & ACLS) effective? A study of BLS & ACLS knowledge amongst healthcare professionals of North-Kerala
- Effects of a general practitioner cooperative co-located with an emergency department on patient throughput
- Acute Care/Trauma Surgeon's role in obstetrical/ gynecologic emergencies (The OBCAT Alert)