肝脏炎性肌纤维母细胞瘤的CT表现与病理对照
2015-10-17蒋玲君徐晓晓张道春
蒋玲君,徐晓晓,张道春
(1.浙江省台州市路桥区第三人民医院,浙江 台州 318056;2.浙江省台州恩泽医疗中心(集团)路桥医院放射科,浙江 台州 318050)
肝脏炎性肌纤维母细胞瘤的CT表现与病理对照
蒋玲君1,徐晓晓2,张道春2
(1.浙江省台州市路桥区第三人民医院,浙江 台州318056;2.浙江省台州恩泽医疗中心(集团)路桥医院放射科,浙江 台州318050)
目的:探讨肝脏炎性肌纤维母细胞瘤(HIMT)的CT表现,以提高对本病的认识。材料和方法:回顾性分析本院经病理证实的6例HIMT的临床资料及CT表现,其中男4例,女2例;年龄48~59岁,平均43岁。6例均行CT平扫及动态增强扫描。结果:6例中,5例单发,1例多发;边界不清4例,边界清晰2例;肝左叶3例,右叶2例,跨肝左、右叶1例。CT平扫均表现为低密度影,密度均匀者2例,密度不均者4例;动态增强扫描动脉期无明显强化2例,轻-中度强化4例;门脉期呈进一步中-重度强化6例,延迟期呈持续性强化5例,强化程度下降1例。另动脉期病变内见供血动脉1例,周围见斑片状异常强化1例;合并肝内胆管扩张1例。结论:HIMT的CT表现多样,动态增强扫描可充分反映病变的病理学特征,结合临床资料,应考虑到本病的可能;但最终确诊仍依赖于病理和免疫组织学检查。
肝肿瘤;肿瘤,肌组织;体层摄影术,螺旋计算机
炎性肌纤维母细胞瘤 (Inflammatory myofibroblastic tumor,IMT)是以纤维结缔组织增生伴大量炎性细胞浸润形成的一种少见的中间性肿瘤;常见的发病部位是肺,发生于肝脏者甚为罕见,最早由Pack于1953首次报道[1]。 笔者搜集本院2005年7月—2014年9月6例经手术病理证实的肝脏IMT(HIMT)的影像学及临床资料,旨在分析、总结本病的CT表现特征,从而增加对本病的认识,提高术前诊断准确率。
1 材料与方法
1.1研究对象
6例HIMT中男4例,女2例;年龄48~59岁,平均43岁;临床表现为上腹部疼痛、不适2例;腹胀、纳差1例;体质量下降1例,另2例为体检偶然发现。6例患者均无肝炎、肝硬化病史,肝功能检查均无异常,肿瘤标志物如AFP、CEA均为阴性。
1.2检查方法
采用Siemens Esprit螺旋CT扫描仪,行CT平扫+三期动态增强扫描。扫描参数:130 kV,120 mAs,层厚5mm,层间距5mm,螺距1.8mm。增强扫描使用非离子型对比剂碘海醇 (350 mgI/mL)1.0~1.5 mL/kg,流率为2.5~3.5 mL/s,注射对比剂25 s、60 s及120 s分别行动脉期、门脉期及延迟期扫描。
2 结果
2.1CT表现
本组6例中,肝左叶3例,肝右叶2例,同时累及肝左、右叶1例;5例单发,1例多发;病变呈类圆形5例,结节状及斑片状1例;边界不清4例,边界清晰2例;范围约17 mm×20 mm~57 mm×47 mm。CT平扫6例均呈低密度(图1a,2a,3a),其中4例密度不均,病变中心可见更低密度区。动态增强扫描动脉期无明显强化2例,轻-中度强化4例;门脉期呈进一步中-重度强化6例;延迟期呈持续性强化5例,其中,2例见“靶征”(图1b~1d),即病变中心可见类圆形、斑片状低密度区,外周带呈等、稍高密度影,最外周为低密度影环绕,增强扫描病变中心低密度区始终无强化,外周带呈不同程度延迟性强化;延迟期强化程度下降1例(图2d)。另动脉期病变内见供血动脉伸入1例(图3b),周围见斑片状异常强化区1例(图3c);合并肝内胆管扩张1例。
2.2病理表现
本组6例表现为良性或低度恶性肿瘤。肿瘤大体观呈实性肿块或息肉样肿物。光镜下肿瘤组织由增生的肌纤维母细胞、纤维母细胞及炎细胞构成,其中可见大量的浆细胞、淋巴细胞浸润。免疫组化显示Vimentin、SMA均为阳性或强阳性表达,ALK、CD-68部分阳性表达,其他标记物 S-100、CD117和CD34均为阴性。
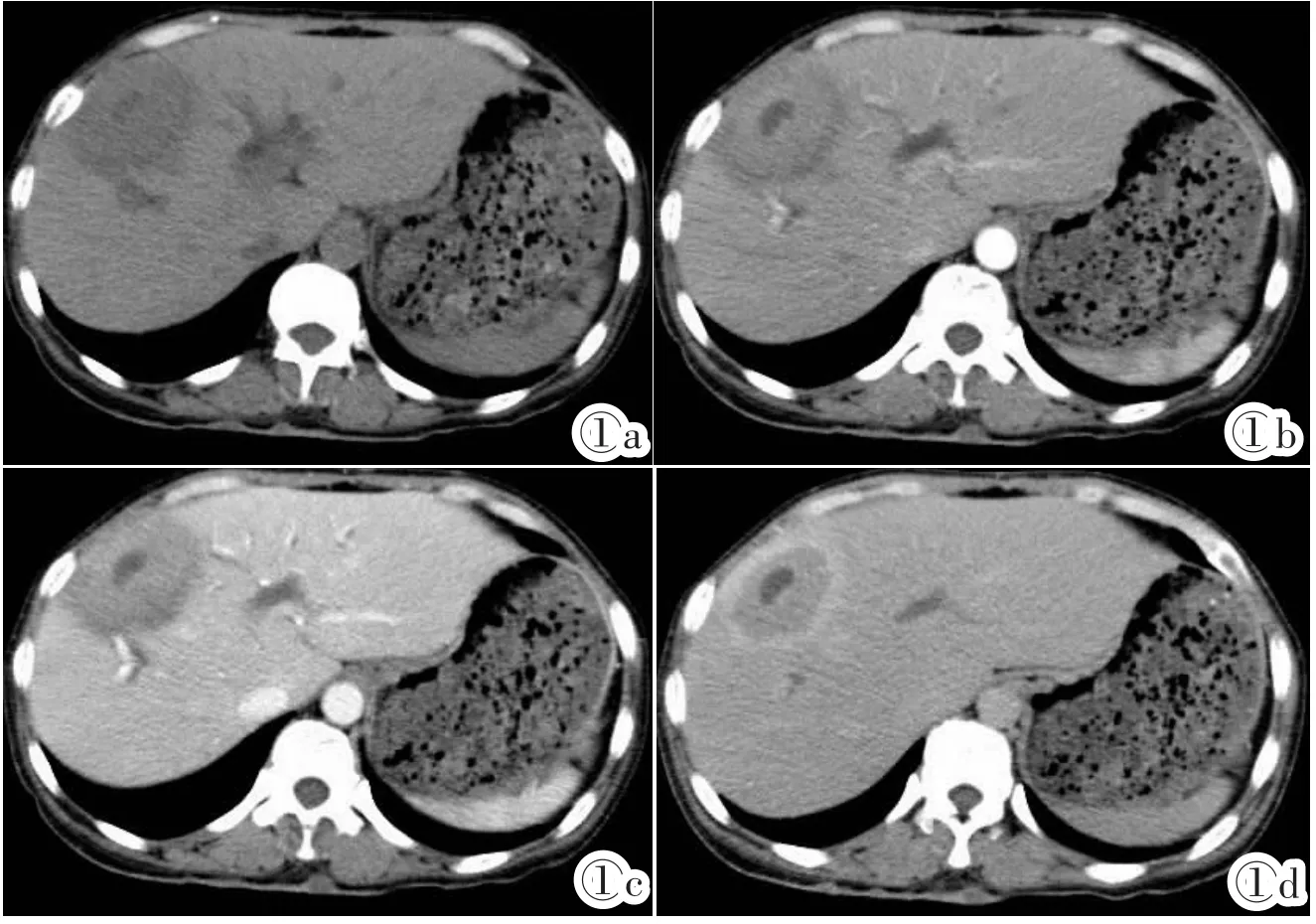
图1a~1d 女,43岁,肝右前叶IMT。图1a:CT平扫示肝右前叶类圆形低密度影,边界尚清,密度不均,中心见斑片状更低密度坏死区;图1b~1d:增强扫描示病变内见“靶征”形成,图1b,1c:动脉期及门脉期示病变内更低密度坏死区,无明显强化,稍外周带呈轻-中度强化,最外周带呈轻度强化,其中,门脉期强化程度略高于动脉期;图1d:延迟期示病变内低密度影始终无强化;稍外周带仍呈持续性强化,最外周带呈明显延迟性强化。Figure 1a~1d. Female,43 years old. IMT in the right anterior lobe of liver.Figure 1a:A round hypo-densitymasswith some patchy necrosis and defined border in right anterior lobe of the liver were shown in the precontrasted enhancement CT images.Figure 1b~1d:A“target sign”was shown in the lesion in the post-contrasted enhancement CT scan.Figure 1b,1c:In the arterial and portal phase,the mass with no clear enhancement in the necrosis lesion and mild/moderate enhancement around the lesion.Otherwise,the enhancement of the lesion in portal phase was more obvious.Figure 1d:The outside segment of lesion was shown obvious enhancement in the delayed phase,but the inside necrosis segment was still no enhancement.
3 讨论
2002年WHO软组织肿瘤新分类中对IMT进行了正确定义:即是由分化的肌纤维母细胞性梭形细胞组成,并常伴大量浆细胞和(或)淋巴细胞的一种肿瘤;并将其归为纤维母细胞/肌纤维母细胞肿瘤;中间性,少数可转移类[2]。从而避免了与其之前一些命名的混淆,如:炎性假瘤、浆细胞肉芽肿、组织细胞瘤等。IMT是一种少见的间叶源性肿瘤,其发病机制尚不明确,部分可发生于手术或创伤后,有研究认为,IMT最初可能是人体对炎症的一种异常或过度反应,最终激活具有增殖潜能的肌纤维母细胞显著增生或失控性生长形成肿瘤性病变[3-4]。
3.1临床特点
IMT好发于肺部,亦可发生于肺外软组织、头颈、腹部脏器、纵隔及生殖道等;但原发于肝脏IMT极为罕见。HIMT临床表现无明显特异性,部分患者仅在体检时偶然发现;常见临床表现有:发热、上腹部疼痛、呕吐,体质量减轻等;绝大多数患者无肝炎、肝硬化病史,肝功能多正常,肿瘤标志物如AFP、CEA多为阴性。本组患者临床表现主要有:上腹部疼痛、腹胀、纳差,体质量下降等,肝功能均无明显异常,与文献报道基本一致。
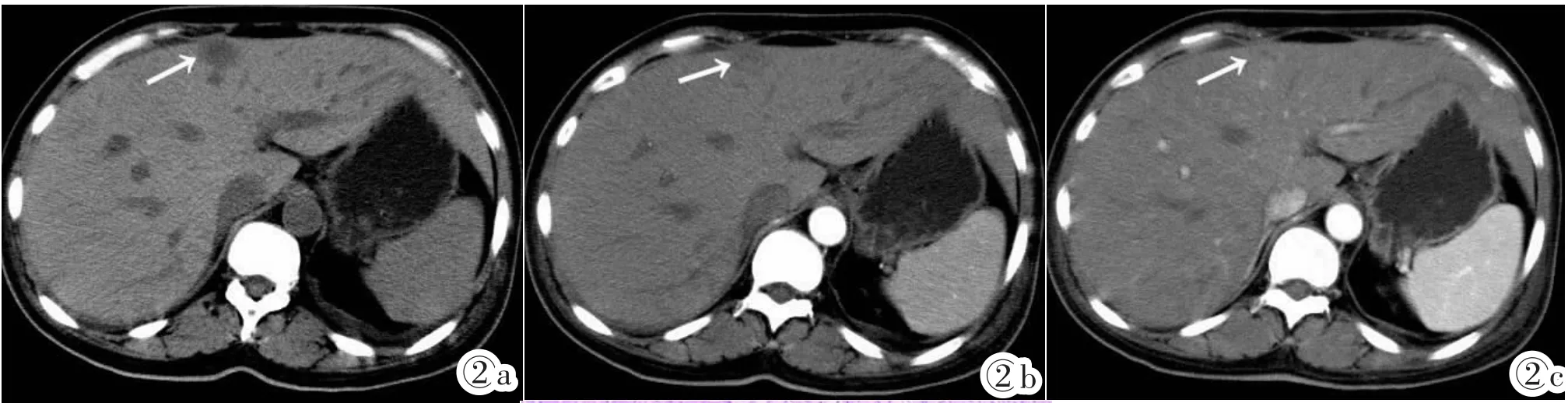
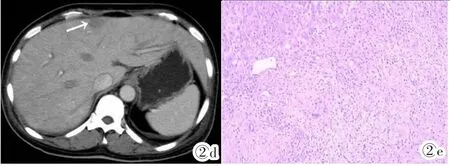
图2a~2e 女,49岁,肝左内叶IMT(箭头)。图2a:CT平扫示肝左内叶类圆形低密度影,边界不清,密度均匀;图2b:增强扫描动脉期病变呈轻度不均匀强化,相对于肝实质仍呈稍低密度影;图2c:门脉期呈进一步持续性强化,强化范围略扩大,以周边强化为主,呈相对稍高密度影,内见斑片状稍低密度区;图2d:延迟期病变强化程度下降,呈相对稍低密度影。图2e:病变内见纤维组织细胞增生,及少许淋巴样细胞浸润,并伴有多量泡沫状细胞灶性增生,形成结节状结构(HE)。Figure 2a~2e. Female,49 years old.IMT in the left medial lobe of liver(arrow).Figure 2a:A round homogeneous hypo-density mass with unclear border in the left medial lobe of liver was shown in the pre-contrasted CT scan.Figure 2b:In the arterial phase,the lesion was shown mild heterogeneous enhancement lower density relative to liver.Figure 2c:In the portal phase,the lesion was shown continued heterogeneous enhancement with some no enhanced low density inside.The enhanced area was larger and then shown hyper-density.Figure 2d:In the delayed phase,the enhancement of the lesion was decreasing and its density was lower than the liver.Figure 2e:HE.There were hyperplastic fibrous tissue cells and a few lymphoid cells,accompanied foamy cells formed a nodular structure in the lesion.

图3a~3c 女,59岁,肝右后叶IMT。图3a:CT平扫示肝右后叶类圆形低密度影,密度均匀,边界欠清;图3b:动脉期肝右后叶见一迂曲血管伸入病变内(箭头);图3c:动脉期示病变呈中度不均匀强化,周围见斑片状明显异常强化区(箭头)。Figure 3a~3c. Female,59 years old.IMT in the right posterior lobe of liver.Figure 3a:A round hypo-density mass with homogeneous density and unclear border in the right posterior lobe of liver was shown in the pre-contrasted CT scan.Figure 3b:In the arterial phase,there was a right hepatic artery branch crossed the lesion(arrow).Figure 3c:In the arterial phase,the lesion with moderate heterogeneous enhancement and obvious abnormal enhancement around it was shown in the lesion(arrow).
3.2病理特点
HIMT是以肝脏局部非肝实质细胞成分炎性增生形成瘤样结节为主要病理特征。大体上病灶可表现为孤立性结节或多个结节融合,部分有完整包膜;剖面呈灰白色或黄白色,部分可见出血、坏死,少数可有中央疤痕。镜检可见不同数量的纤维母细胞及毛细血管代替正常的肝脏组织,其间散在有较多增生组织细胞、多克隆细胞,亦可有淋巴细胞、嗜酸性粒细胞等慢性炎性细胞浸润。其镜下表现与疾病的演变过程相符合:病变初期会出现大量的炎细胞、肉芽组织及坏死;随着病变进展,胶原纤维增多,最后可出现胶原团。免疫组化常表达Vimentin、SMA、MSA,部分病例 Desmin阳性,S-100、myoglobin、CD34阴性[5]。
3.3影像学表现
HIMT可发生于任何年龄,以青壮年居多,男性多于女性;可单发或多发,以肝右叶多见。本组6例中,男4例,女2例,平均年龄43岁;肝左叶3例,肝右叶2例,同时累及肝左、右叶1例;其中1(1/6)例多发;本组发病年龄及部位与文献报道不完全相符,可能与病例数较少有关。
CT平扫常表现为边界清或不清低密度影,密度均匀或不均匀,钙化少见。根据病变不同的病理发展阶段,HIMT可表现为不同的CT动态增强表现,无明显特异性。笔者学习本组6例HIMT CT动态增强表现并结合相关文献复习[6],总结如下:①HIMT动态增强扫描常见表现有:动脉期不强化或轻度强化,门脉期强化较动脉期明显,这与病变主要由门静脉供血,肝动脉供血较少有关;延迟期呈持续性强化,强化范围进一步扩大,呈等、稍高密度影;病变内常可见斑点、片状低密度不强化区,部分可见“靶征”形成,即病变中心可见类圆形、斑片状低密度区,外周带呈等、稍高密度影,最外周为低密度影环绕,增强扫描病变中心低密度区始终无强化,外周带呈不同程度延迟性强化;本组可见2(2/6)例,与病灶中心为散在斑点状、片状凝固性坏死,而周围多为环带状纤维组织包裹及炎性细胞浸润的病理基础相对应;其中,低强化区以纤维组织细胞浸润为主,而高强化区以炎性细胞(包括泡沫组织细胞、浆细胞及淋巴细胞等)浸润为主。另增强扫描动脉期部分病变周围可见斑片状强化,经病理证实其血管内皮细胞标记物CD34(+)[7],本组中可见1(1/6)例。②HIMT动态增强扫描少见表现有:动脉期呈轻度强化,门脉期呈进一步强化,强化程度较动脉期明显,范围略扩大,延迟期病变强化程度下降,呈相对稍低密度影;笔者推测可能与病变内纤维组织成分相对较少,造影剂廓清较快有关;本组仅1例(1/6)见此类似表现,与Liu等[8]报道相一致。
3.4鉴别诊断
HIMT需与肝脓肿、肝转移瘤、肝内胆管细胞癌及原发性肝细胞癌等相鉴别。①肝脓肿起病急,常有腹痛、发热及白细胞升高等症状,病灶内常见多房、分隔状改变,外周水肿带无延迟性强化;但当其外周带有肉芽组织形成时二者难以鉴别;且肝脓肿可向HIMT转归,即所谓假瘤样肝脓肿。②肝转移瘤常多发,并有原发肿瘤病史,病灶周围少见低密度环及延迟性强化改变等。③肝内胆管细胞癌亦可表现为动态增强早期轻度强化,门脉期、延迟期呈持续性轻中度强化;但胆管细胞癌常以肝左叶多见,并常可见邻近肝被膜皱缩,病灶内或周边常可见胆管扩张,管壁增厚等征象。④原发性肝细胞癌,典型者容易鉴别;但对于少数不典型者,如少血供者或有门静脉参与供血者,其强化形式常与HIMT重叠,二者鉴别较困难;因此,常需要结合临床有无肝炎、肝硬化病史及AFP的测定等进行辅助诊断。
3.5治疗及预后
HIMT是肝脏偏良性肿瘤,发展缓慢,极少发生恶变;大部分患者经激素或抗生素治疗后肿块可缩小或消失;而对于术前不能完全除外肝脏其他恶性肿瘤,经激素、抗生素等药物治疗无效或病情进展者,则应积极采取手术治疗。由于HIMT是一种惰性肿瘤,且患者很少合并肝炎、肝硬化等病史,因此其预后良好,患者可长期存活。
[1]Pack GT,Banker HW.Total right hepatic lobectomy.Report of a case[J].Ann Surg,1953,138(3):253-258.
[2]Fletcher CDM,Unni KK,Mertens F.World Health Organization classification of tumours:pathology and genetics of tumours of soft tissue and bone[M].Lyon:IARC Press,2002:48-106.
[3]Gale N,Zidar N,Podboj J,et al.Inflammatory myofibroblastic tumor of paranasal sinuses with fatal outcome:reactive lesion or tumor[J].J Clin Pathol,2003,56(9):715-717.
[4]Coffin CM,Watterson J,Priesmt JR,et al.Extrapulmonary inflammatorymyofibroblastictumor.Aclinicopathologicandimmunohistochemical study of 84 cases[J].Am J Surg Pathol,1995,19(8):859-872.
[5]Cook JR,Dehner LP,Collins MH,et al.Anaplastic lymphoma kinase(ALK)expression in the inflammatory myofibroblastic tumor:a comparative immunohistochemical study[J].Am J Surg Pathol,2001,25(11):1364-1371.
[6]唐威,周纯武.肝脏炎性肌纤维母细胞瘤的影像学诊断[J].放射学实践,2009,24(2):217-220.
[7]See TC,Davies SE,Appleton DS,et al.CT and angiographic features of hepatic inflammatory myofibroblastic tumour[J].Clin Radiol,2005,60(6):718-722.
[8]Liu XF,He BM,OU-Yang XH,et al.Different imaging findings of inflammatory myofibroblastic tumor of the liver[J].World J Gastroenterol,2012,18(40):5821-5825.
Comparison with CT imaging features and pathologic findings of hepatic inflammatory myofibroblastic tumor
JIANG Ling-jun1,XU Xiao-xiao2,ZHANG Dao-chun2
(1.Luqiao District of Taizhou City Third People's Hospital,Taizhou Zhejiang 318056,China;2.Department of Radiology,Taizhou Enze Medical Center(Group)Luqiao Hospital,Taizhou Zhejiang 318050,China)
Objective:To evluate the CT imaging features of hepatic inflammatory myofibroblastic tumor(HIMT),so as to improve its diagnostic accuracy.Materials and Methods:The clinical and CT imaging findings of 6 cases of HIMT which confirmed by pathology in our hospital were analyzed retrospectively,including 4 males and 2 females,aged from 48 to 59 years old,mean age was 43 years old.Pre-and post-contrast CT images were examined for all six cases.Results:Five of six cases were single lesion,the other one was multiple.Clear margin was in four cases and unclear margin in two cases. Three cases were located in the left lobe of liver,2 cases were in the right lobe of the liver and 1 case was located both the left and right lobe.In the pre-contrasted enhancement CT scan,heterogeneous(n=2)or homogeneous(n=4)hypo-density were shown in six cases.No enhancement(n=2)or mild/moderate enhancement(n=4)was shown in arterial phase respectively. Delayed enhancement was shown in the portal phase(n=6)and the delayed phase(n=5).Moreover,on the arterial phase image,feeding artery were shown in one case,having patchy enhancement around it in one case.The dilatation of the intra-hepatic bile duct was seen in one case.Conclusion:The dynamic contrast enhancement CT features of HIMT are multiple characteristic,which correlate with its pathologic findings.But the final diagnosis relies on pathology and immunohistochemistry examination.
Liver neoplasms;Neoplasms,muscle tissue;Tomography,spiral computed
R735.7;R730.262;R814.42
A
1008-1062(2015)07-0487-04
2014-12-16;
2015-01-20
蒋玲君(1977-),女,浙江台州人,主治医师。
