罕见腰椎椎旁非创伤性骨化性肌炎1例
2015-06-01刘富兵冯振洲陈子贤姜晓幸
刘富兵 梁 运 冯振洲 蒋 淳 陈子贤 姜晓幸
(复旦大学附属中山医院骨科 上海 200032)
罕见腰椎椎旁非创伤性骨化性肌炎1例
刘富兵 梁 运 冯振洲 蒋 淳 陈子贤 姜晓幸△
(复旦大学附属中山医院骨科 上海 200032)
Myositis ossificans(MO),also known as myositis ossificans circumscripta(MOC),describes a pathologic process of which localized,nonneoplastic heterotopic bone formation occurs in muscles or other soft tissues[1-2].Although traumatic MO has been reported occasionally,MO located in lumbar paraspinal muscles without a history of trauma has been rarely seen.To our best knowledge,it is the fifth such case as nontraumatic MO located in the lumbar paraspinal muscles and first young case misdiagnosed as epithelium-like tumor.
Case ReportA 27 year-old male was admitted to Zhongshan Hospital,Fudan University,complaining of left back untouchable soreness and left lower extremity hyperesthesia for one month. He used to be a healthy man and recalled no back injury history.Physical examination revealed tenderness of left L4-5 paraspinal muscle and hyperesthesia of left medial shank.The blood routine,hepatorenal function test,electrolytes,and coagulation time were all normal,indicating no calcium-phosphorus metabolic or hematological disorders.X-ray of lumbar spine also had no positive findings,while magnetic resonance imaging (MRI)he had previously taken ten days following the onset of his symptoms,showed a mass embedded in the left Erector Spinae adjacent to L4 spinous process,with isodensity on T1-weighted scans and high signal intensity on both T2-weighted and enhanced T1-weighted images (Fig 1).Ultrasound revealed a round intramuscular hypoechoic area encircled by a hyperechoic curvature(Fig 2),while the ultrasound guided biopsy suggested an epithelium-derived neoplasm(Fig 3),which seemed questionable as an epithelial tumor was abnormally located at such muscular site.The F-18 fluorodeoxyglucose/PET-CT showed an isolated L4 paraspinal well-marginated mass,characterized by extremely high glucose metabolism,with the maximum Standard Uptake Value(SUV)of 8.5(Fig 4).As all above examinations failed to reach a definite diagnosis,surgical exploration and removal was then made,with paraffin pathology revealing MO(Fig 3).The patient′s symptoms got relieved immediately after surgery and returned to normal activity 1 month postoperatively.Radiography revealed no signs of recurrence at 6 months′follow-up(Fig 5).
DiscussionMO is first introduced by Von Dush in 1868[3],and defined as a benign,localized,heterotopic bone and cartilage formation in soft tissues or muscles[1-2].It most commonly occurs in men within the second and third decades of life[1,4].The common locations of MO include the thigh,upper arm,elbow and shoulder,while it rarely involved some other part of our body[1,4-5]. To our best knowledge,only four lumbar paraspinal MOs have been reported,all with no history of trauma[5-8](Tab 1).There are many causal factors contributing to the happening of MO[9-10],among which,trauma accounts for 60%-75%[1,11].However,the concrete pathogenesis has not been clarified.
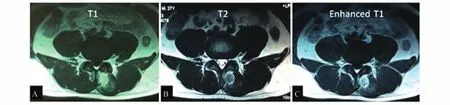
Fig 1 MRI of MO
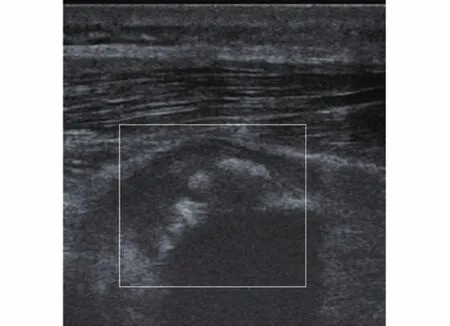
Fig 2 Ultrasound manifestation of MO
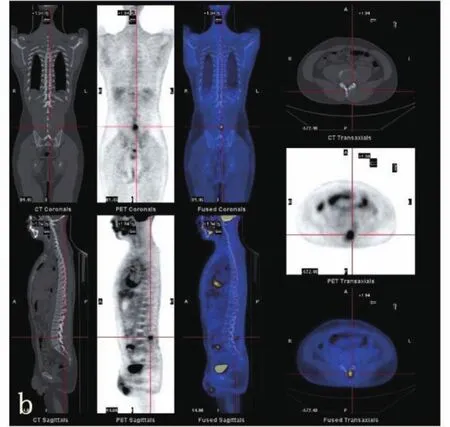
Fig 3 The F-18 fluorodeoxyglucose/PET-CT of MO
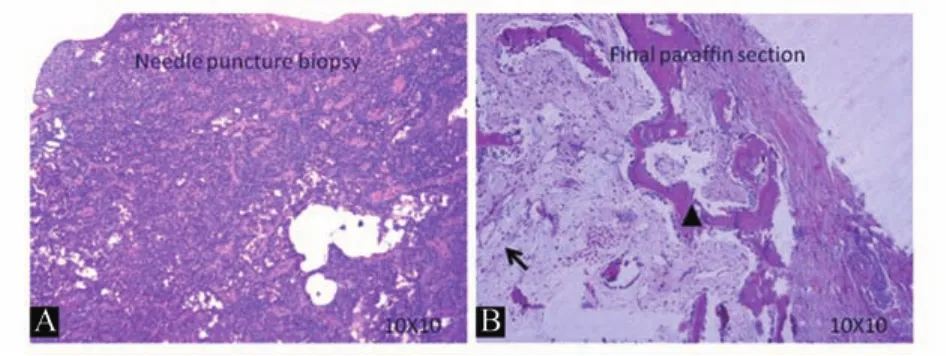
Fig 4 Pathology of MO
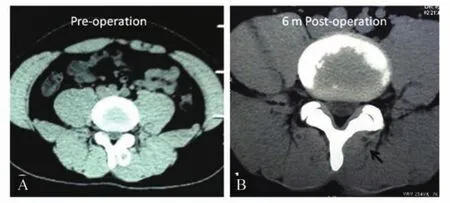
Fig 5 Pre-operative CT(A)and 6 months postoperative CT of L4-5(B)
Patients with MO often present with local pain and swelling,palpable mass or limited freedom of movement,with a definite previous trauma at or near the sites of MO.Laboratory tests can reveal some nonspecific findings while the most characteristic findings are radiological involution and a peripheral rim-like calcification/ossification and central soft tissues,called zonal phenomenon[12].At acute phase(≤2 weeks),MO usually appears as a soft-tissue mass,with MRI showing localized mass and extensive surrounding edema.As the lesion matures,the peripheral ossification occurs and becomes denser,with CT,MRI and ultrasound all revealing zonal phenomenon[3-4,9]. In the current study,although MRI,ultrasound,and CT were taken consecutively and showed zonal phenomenon,the ultrasound-guided biopsy made the misdiagnosis.The reason has been discussed in detailsummarized as follows:firstly,the tissue volume obtained by needle puncture was limited,only a small part of the lesion has been collected;secondly,fast frozen section was such a method that prone to disturb the origin morphology and structure of the tissues,the osteoblasts in the punctured tissues were compressed and looked like epithelial-derived cells;what′s more,the heterogeneity of soft tissue lesions often made a definite diagnosis of MO hard to be established. However,fine needle aspiration(FNA)was still a valuable method in preoperative diagnosis,as Ng,et al.[13]showed that subtyping and grading for malignant lesions were 77.2%and 95.2% accurate,respectively.To improve the accuracy of preoperative diagnosis,clinical examination,radioimaging and histological examination should all be taken into consideration.Core needle with larger diameter other than fine needle,under ultrasound or CT guide could be used to more accurately obtain more lesion tissues.In addition,when CT showed a mass with a zonal phenomenon,MO should be highly suspected.by us with the pathologists and could be
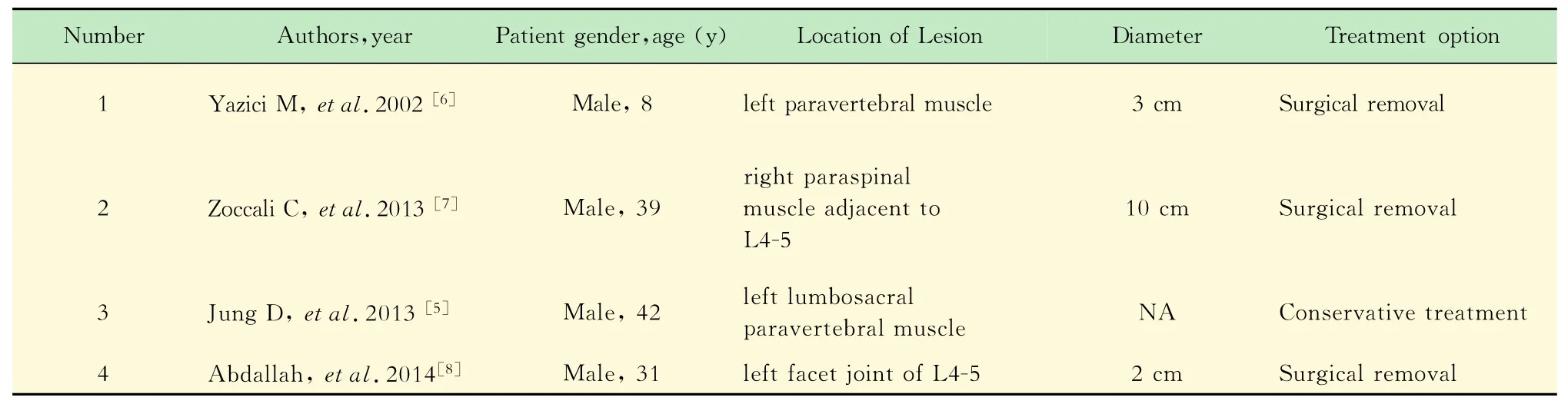
Tab 1 Reports of non-traumatic MO in lumbar paraspinal muscles
In our study,surgical exploration was performed at last to firgue out the true nature of the mass.On paraffin section,a typical zonal pattern,first named by Ackerman,developed with three distinct zones:(1)the inner zone consisted of organizing granulation tissue and proliferating fibroblasts;(2)the intermediate zone was characterized by osteoblasts with immature osteoid formation and islands of cartilage due to enchondral ossification;(3)the peripheral zone was composed of mature bone,usually surrounded by fibrous tissue[8,14].And this zonal pattern was considered to be an important criterion for MO.
[1]McCarthy EF,Sundaram M.Heterotopic ossification:a review[J].Skeletal Radiol,2005,34(10):609-619.
[2]Wu JS,Hochman MG.Soft-tissue tumors and tumorlike lesions:a systematic imaging approach[J].Radiology,2009,253(2):297-316.
[3]Parikh J,Hyare H,Saifuddin A.The imaging features of post-traumatic myositis ossificans,with emphasis on MRI [J].Clin Radiol,2002,57(12):1058-1066.
[4]Kim SW,Choi JH.Myositis ossificans in psoas muscle after lumbar spine fracture[J].Spine(Phila Pa 1976),2009,34(10):E367-E370.
[5]Jung D,Cho KT,Roh JH.Non-traumatic myositis ossificans in the lumbosacral paravertebral muscle[J].J Korean Neurosurg Soc,2013,53(5):305-308.
[6]Yazici M,Etensel B,Gursoy MH,et al.Nontraumatic myositis ossificans with an unusual location:case report [J].J Pediatr Surg,2002,37(11):1621-1622.
[7]Zoccali C,Chichierchia G,Covello R.An unusual case of lumbar paravertebral miositis ossificans mimicking muscular skeletal tumor[J].Musculoskelet Surg,2013,97 (3):251-253.
[8]Abdallah A,Gokcedag A,Ofluoglu AE,et al.Nontraumatic myositis ossificans in the lumbar spine[J].Am J Case Rep,2014,15:421-425.
[9]Lin TY,Wu CC,Chiang FY,et al.Noninfectious painful neck mass mimicking malignancy in a child[J].Head Neck,2011,33(5):753-755.
[10]Lee DG,Lee S H,Hwang SW,et al.Myositis ossificans in the paraspinal muscles of the neck after acupuncture:a case report[J].Spine J,2013,13(7):e9-e12.
[11]Baysal T,Baysal O,Sarac K,et al.Cervical myositis ossificans traumatica:a rare location[J].Eur Radiol,1999,9(4):662-664.
[12]Sirvanci M,Ganiyusufoglu AK,Karaman K,et al. Myositis ossificans of psoas muscle:magnetic resonance imaging findings[J].Acta Radiol,2004,45(5):523-525.
[13]Ng VY,Thomas K,Crist M,et al.Fine needle aspiration for clinical triage of extremity soft tissue masses[J].Clin Orthop Relat Res,2010,468(4):1120-1128.
[14]Meara RS,Bell W,Chhieng DC,et al.An unusual neck mass clinically mimicking an enlarged supraclavicular lymph node:cytological features of myositis ossificans circumscriptus[J].Cytopathology,2009,20(2):121-126.
[15]Falliner A,Drescher W,Brossmann J.The spine in fibrodysplasia ossificans progressiva:a case report[J]. Spine(Phila Pa 1976),2003,28(24):E519-E522.
[16]Findlay I,Lakkireddi PR,Gangone R,et al.A case of myositis ossificans in the upper cervical spine of a young child[J].Spine(Phila Pa 1976),2010,35(25):E1525-E1528.
The differential diagnosis consists of fibrodysplasia ossificans progressive(FOP),osteosarcoma,and other sarcomatous neoplasms[15].FOP is an extremely rare,severely disabling and autosomaldominant disorder characterized by postnatal progressive heterotopic ossification of the connective tissue[1,15].Different from MO,the more heavily ossified portion of osteosarcoma is in the center,and the poorly organized radiolucent tissue is at the periphery[9,11].Besides,pleomorphic atypical cells with atypical mitotic figures can be found in osteosarcoma,which is absent in MO[10].
Since MO is a self-limited disease,it is often treated conservatively.By applying rest,ice,and non-steroidal anti-inflammatory agents[10],most patients can get complete remission.Radiation therapy can be used to reduce the size and accelerate the maturation of the lesion[9,16]. Surgical excision is indicated for patients with severe pain,limitation of movement,or neurovascular compression,and also for those difficult to diagnose[9],like ours.Besides,6 month′s follow-up revealed no recurrence,which meant total removal didn′t necessarily lead to recurrence.
Non-traumatic myositis ossificans located in lumbar paraspinal muscles is rarely reported. Surgical excision should be taken into considerationfor patients with severe pain,limitation of movement,or neurovascular compression,and also for those difficult to diagnose.
myositis ossificans; non-traumatic;lumbar; paraspinal muscles
R 685.2
B
10.3969/j.issn.1672-8467.2015.05.024
2014-11-04;编辑:王蔚)
△Corresponding author E-mail:jiang.xiaoxing@zs-hospital.sh.cn
