Clinical Observation of Acupuncture plus Patent Chinese Medicine for Post-stroke Constipation
2014-06-24
1 People’s Hospital of Qitaihe City, Heilongjiang Province, Qitaihe 154000, China
2 Xiyuan Hospital of Beijing University of Chinese Medicine, Beijing 100091, China
3 Shaanxi University of Chinese Medicine, Xianyang 712046, China
4 Affiliated Hospital of Hebei United University, Tangshan 063000, China
SPECIAL TOPIC STUDY
Clinical Observation of Acupuncture plus Patent Chinese Medicine for Post-stroke Constipation
Song Xue-feng1, Wu Ying2, Zhang Zheng-xu3, Zheng De-song4
1 People’s Hospital of Qitaihe City, Heilongjiang Province, Qitaihe 154000, China
2 Xiyuan Hospital of Beijing University of Chinese Medicine, Beijing 100091, China
3 Shaanxi University of Chinese Medicine, Xianyang 712046, China
4 Affiliated Hospital of Hebei United University, Tangshan 063000, China
Author: Song Xue-feng, bachelor, attending physician.
E-mail: liqi19801211@163.com
Objective: To observe the clinical efficacy of acupuncture plus patent Chinese medicine in treating post-stroke constipation.
Methods: Sixty eligible patients with post-stroke constipation were randomized into a treatment group and a control group, 30 in each group. The treatment group was intervened by acupuncture plusMa Zi Renpill, while the control group was byMa Zi Renpill alone. The symptoms of constipation were observed before and after intervention.
Results: After 2-week treatment, the constipation condition was improved in both groups, and the improvement in the treatment group was statistically more significant than that in the control group (P<0.05); respectively two weeks and a month after the intervention, the treatment group was superior to the control group in comparing the constipation score (P<0.05). However, acupuncture didn’t show marked effect in improving defecation speed, initial defecation time, and spontaneous discharge frequency. The treatment group had a significantly higher short-term markedly-effective rate compared with the control group (P<0.05); the long-term therapeutic efficacy of the treatment group was significantly higher than that of the control group (P<0.05). The adverse events happened in the treatment group were significantly less than those in the control group (P<0.05).
Conclusion: Acupuncture at specific acupoints plus patent Chinese medicine can produce a content therapeutic efficacy.
Acupuncture Therapy; Acupuncture Medication Combined; Stroke; Complications; Constipation
As one of the complications of stroke, constipation usually interacts with stroke, not only affecting the patients’ quality of life but may also aggravate stroke, leading to severe consequences. Regular treatments for constipation somehow have some limitations[1]. Therefore, we adopted acupuncture plus patent Chinese medicine in treating post-stroke constipation. The report is now given as follows.
1 Clinical Materials
1.1 Diagnostic criteria
1.1.1 Diagnostic criteria of stroke
Referring the diagnostic criteria of stroke in theCriteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine[2]and the diagnostic criteria of cerebral accident of Western medicine[3]. Sudden loss of consciousness, wry mouth, trouble speaking,hemiplegia; or wry mouth and hemiplegia without loss of consciousness.
1.1.2 Diagnostic criteria of constipation
Constipation was diagnosed according to Rome III diagnostic criteria of functional constipation[4]. (1) Must include at least 2 of the following 6 symptoms:① straining ≥25% of defecations; ② lumpy or hard stools ≥25% of defecations; ③ sensation of incomplete evacuation ≥25% of defecations; ④sensation of anorectal obstruction or blockage≥25% of defecations; ⑤manual maneuvers to facilitate ≥25% of defecations (e.g. digital evacuation, support of the pelvic floor);⑥<3 defecations a week. (2) Loose stool rarely present without use of laxatives. (3) Insufficient criteria for irritable bowel syndrome (IBS).
The onset ≥6 months prior to diagnosis, and the symptoms ≥3 months.
1.2 Inclusion criteria
Conforming to the above diagnostic criteria of stroke and constipation; no gender predilection; age between 49 and 69 years old.
1.3 Exclusion criteria
Digestive diseases involving liver, gallbladder, or pancreas; with a history of anorectal operation; with primary fatal diseases of liver, kidney, or hematopoietic system; with mental diseases.
1.4 Dropout criteria
Those who failed to follow the treatment protocol or used other treatments during the study; those who failed to insist on treatment; severe adverse events happened during the study; severe complications or aggravation during the study.
1.5 Statistical methods
All data were processed by using SPSS 19.0 version software. The measurement data were expressed byand analyzed byt-test. The enumeration data were analyzed by using Chi-square test. The ranked data were by usingRidittest.
1.6 General data
Totally 60 patients with post-stroke constipation were included from the Rehabilitation Department of the Affiliated Hospital of Hebei United University. The patients were divided into a treatment group and a control group by using random number table, 30 in each group. There were no significant differences in comparing gender, age, disease duration, or disease type between the two groups (allP>0.05), indicating the comparability (Table 1).
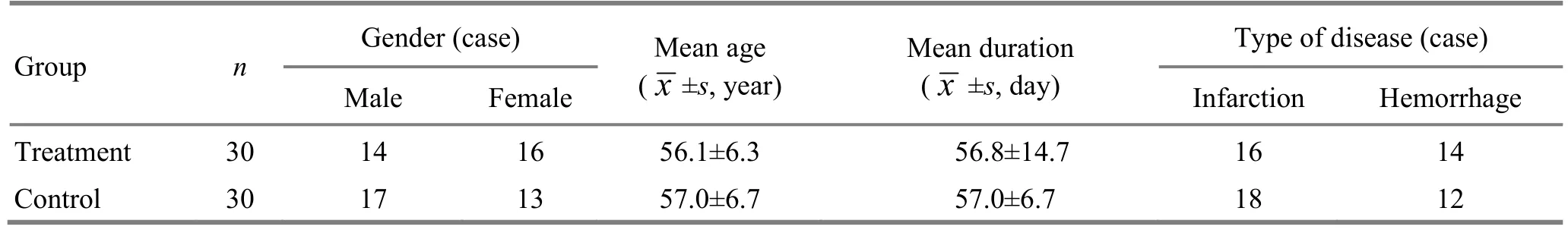
Table 1. Comparison of general data
2 Treatment Methods
2.1 Treatment group
2.1.1 Acupuncture
Acupoints: Bilateral Tianshu (ST 25), Fenglong (ST 40), Zhigou (TE 6), Zhongchong (PC 9), Shenshu (BL 23), Zhaohai (KI 6), left Fujie (SP 14), and Shuigou (GV 26).
Operation: The patient took a supine position first. Filiform needles of 0.35 mm in diameter and
50-100 mm in length were used. After routine sterilization, Fenglong (ST 40), Shenshu (BL 23), and Fujie (SP 14) were perpendicularly punctured for 1.5-2 cun; Zhigou (TE 6) was punctured perpendicularly for 1-1.5 cun; when needles were inserted into Zhongchong (PC 9) and Zhaohai (KI 6), needling manipulations were applied to produce a distending sensation in the local area, and the punctured depth was 0.5-1 cun. Shuigou (GV 26) was punctured obliquely with the needle tip towards nasal septum for 0.3-0.5 cun, applied with birdpecking reducing manipulation within the patient’s tolerance. Lifting-thrusting and twirling reinforcing manipulations were used for Zhongchong (PC 9), Zhaohai (KI 6), and Shenshu (BL 23), twirling amplitude <180°, frequency 40-50 r/min, 2 min for each point. The needle in Shenshu (BL 23) was not supposed to retain, but the other needles were retained for 30 min. The treatment was given once a day, for successive 14 d.
2.1.2 Patent Chinese medicine
Ma Zi Renpill (manufactured by Tong Ren Tang Pharmaceutical Factory of Beijing Tong Ren Tang Group Co., Ltd., China Food and Drug Administration approval number: Z11020159), 2 pills each time, once a day, by warm water, for 14 d.
2.2 Control group
The same patent Chinese medicine was used for the control group, with same dosage and usage.
3 Therapeutic Observation
3.1 Observation indexes
3.1.1 Constipation score
Constipation symptoms were observed before intervention, right after intervention, 2 weeks after intervention, and 1 month after intervention, and scored by using semi-quantitative symptom scoring method[5]. See the scoring criteria below (0 for degree 1, 2 for degree 2, and 4 for degree 3).
Defecation desire: Urgent, score 0; mild, score 2; no desire score 4.
Defecation speed: Defecation <5 min, score 0; 5-10 min, score 2; >10 min, score 4.
Stool shape: Normal, score 0; hard, score 2; lumpy, score 4.
Difficulty in defecation: Without effort, score 0; pushing hard, score 4; requiring manual maneuvers, score 4.
Pain due to defecation: No pain, score 0; mild pain, score 2; extreme pain, score 4.
Constipation duration: Duration <1 month, score 0; 2-3 months, score 2; >3 months, score 4.
Sensation of incomplete evacuation: In absence of sensation of incomplete evacuation, score 0; accidentally, score 2; frequently, score 4.
Difficulty passing stool: In absence, score 0; accidentally, score 2; frequently, score 4.
Time prior to the initial defecation: Time <8 h, score 0; 8-16 h, score 2; >24 h, score 4.
Defecation interval: Interval <24 h, score 0; 24-48 h, score 2; >48 h, score 4.
Defecation times per week: Defecation >4 times, score 0; 2-3 times, score 2; <2 times, score 4.
The sum of the above scores was the total score.
3.1.2 Short-term and long-term therapeutic efficacies
The short-term therapeutic efficacy at treatment day 14 was observed, as well as the long-term therapeutic efficacies 2 weeks and 1 month after the intervention.
3.1.3 Adverse events
The adverse events were also observed and recorded.
3.2 Criteria of therapeutic efficacy
The criteria of therapeutic efficacy were made based upon theGuiding Principles for Clinical Study of New Chinese Medicines[6]and the improvement rate of symptom score.
Improvement rate of symptom score =(Pre-treatment total score - Post-treatment total score) ÷ Pre-treatment total score × 100%.
Recovery: Normal stools, improvement rate≥95%.
Marked effect: Significant improvement of constipation, improvement rate ≥70% but <95%.
Effective: Improvement of constipation, and improvement rate ≥30% but <70%.
Invalid: No improvement of constipation, improvement rate <30%.
3.3 Results
3.3.1 Comparison of short-term constipation score
Before intervention, there were no significant differences in comparing the component symptom scores (P>0.05) between the two groups. Right after 2-week treatment, the symptom scores were changed significantly in the treatment group (P<0.05); in the control group, except for the score of defecation times per week, the other item scores were changed significantly (P<0.05); there were significant differences in comparing the item scores between the two groups (P<0.05). The results showed that the improvements in the treatment group were superior to those in the control group (Table 2).3.3.2 Comparison of short-term therapeutic efficacy
Table 2. Comparison of the symptoms score (point)
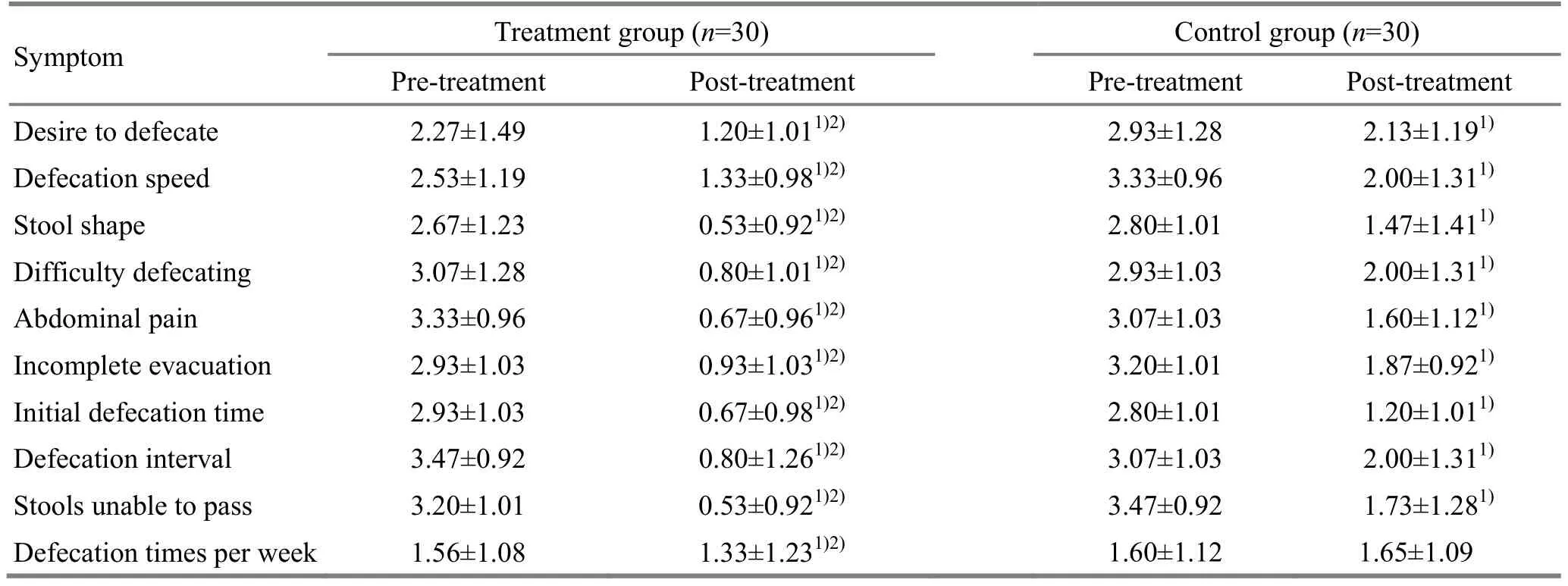
Table 2. Comparison of the symptoms score (point)
Note: Intra-group comparison, 1) P<0.05; compared with the control group after treatment, 2) P<0.05
?
Two weeks after intervention, there were significant differences in comparing the markedlyeffective rate and total effective rate between the two groups (bothP<0.05), indicating that the shortterm therapeutic efficacy of the treatment group is higher than that of the control group (Table 3).
3.3.3 Comparison of long-term therapeutic efficacy
A month after intervention, there were significant differences in comparing the markedly-effective rate and total effective rate between the two groups (bothP<0.05), indicating that the long-term therapeutic efficacy of the treatment group is higher than that of the control group (Table 4).
3.3.4 Comparison of adverse events
A patient experienced diarrhea and abdominal pain in the treatment group. Three patients had abdominal pain, 2 cases had diarrhea, 1 case had nausea and vomiting, and 1 case had abdominal distension in the control group.
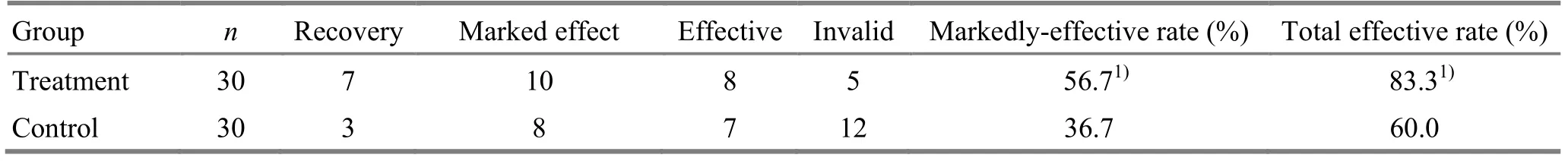
Table 3. Comparison of short-term therapeutic efficacy (case)
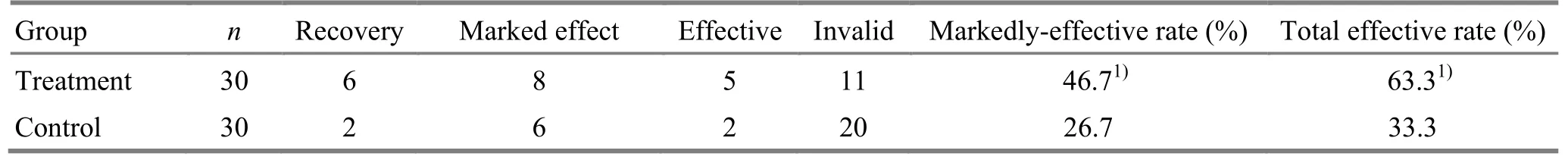
Table 4. Comparison of therapeutic efficacy a month after intervention (case)
4 Discussion
In recent years, with the increase of incidence of stroke, the incidence of post-stroke constipation is also rising, deeply affecting the patients’ quality of life and health[7]. The intra-abdominal pressure increases when constipation patient defecates, inducing the rising of blood pressure. When more blood enters cerebral vessels, the vessel may rupture at its weak point, leading to cerebral hemorrhage, what Chinese medicine calls stroke. Stroke also increases the risk of constipation. In stroke patients in coma, the local cerebral nervous dysfunction can inhibit the defecation reflex and subsequently cause stools to over-retain in intestines. When water in stools is over-absorbed, constipation will occur. Besides, due to limitation of movement, stroke patients usually stay in bed for a long time and change his old habits of diet, defecation and posture of defecation. Gastrointestinal movements are also reduced because of limited movements. These factors all can lead to constipation. Therefore, constipation and stroke often interact as both cause and effect. It’s essential to keep smooth bowel movements in stroke patients for the recovery and treatment[8].
Currently, oral laxatives or enema is commonly used in clinic for post-stroke constipation. Indeed, these methods can improve the symptoms for a while, but the long-term therapeutic efficacy is not satisfactory, and adverse events are easy to happen[9]. Chinese medicine holds that the pathogenesis of post-stroke constipation involves the obstruction of qi in Fu organs and the turbid qi failing to descend[10]. In this study, Tianshu (ST 25), Zhongchong (PC 9), Shenshu (BL 23), Fujie (SP 14), Fenglong (ST 40), Zhaohai (KI 6), Shuigou (GV 26), and Zhigou (TE 6) were selected for intervention. Tianshu (ST 25) is the Front-Mu point of the large intestine, boosted by the qi of Stomach Meridian of Foot Yangming, functioning to regulate intestines, activate qi flow and unblock stagnation[11]. A bidirectional regulation effect of Tianshu (ST 25) has been discovered by researchers in recent years[12]. As the Luo-Connecting point of the Stomach Meridian, diverting into the Spleen Meridian of Foot Taiyin, Fenglong (ST 40) can modulate the function of spleen and stomach, reduce phlegm and promote qi flow of the spleen and stomach[13]. Zhigou (TE 6) can modulate the qi activities in three jiao, and therefore is often used in treating constipation. The pericardium can protect and assist the function of heart. As the Jing-Well point of the Pericardium Meridian of Hand Jueyin, Zhongchong (PC 9) can adjust the function of qi and blood, dredge and unblock meridians and collaterals when stimulated[14]. It’s found in clinic that pressing Zhongchong (PC 9) can release tension and promote defecation in constipation, hence especially useful for the aged. Shenshu (BL 23) is the Back-Shu point of kidney, while kidney is in charge of discharge, and normal urination and defecation both rely on sufficient kidney qi. Hence, acupuncture at bilateralShenshu (BL 23) plus reinforcing needling manipulations can boost kidney qi and promote defecation. Fujie (SP 14) is where abdominal qi gathers, working to tonify spleen and resolve dampness, descend the adverse-rising qi and promote defecation. In this study, Fujie (SP 14) was only selected from the left side because the descending colon is located there. It can enhance the movement of descending colon and promote defecation by stimulating this point. Zhaohai (KI 6) is one of the Eight Confluent points, connecting to the Yin Heel Vessel. It’s good for reinforcing kidney and producing essence, and can modulate the discharge, especially effective for constitution in the elderly. As the crossing point of the Yangming Meridians and the Governor Vessel, Shuigou (GV 26) can significantly promote the restore of intelligence in patients with cerebral infarction and is effective in treating post-stroke depression and post-stroke constipation. The qi can flow smoothly in Fu organs when the above points are used together.Ma Zi Renpill is a patent Chinese medicine commonly used for constipation. In this formula,Huo Ma Ren(Fructus Cannabis) works as the monarch drug to moisturize intestines and promote defecation;Da Huang(Radix et Rhizoma Rhei) reduces heat and promotes defecation,Xing Ren(Semen Armeniacae Amarum) descends qi and moisturizes intestines, andBai Shao(Radix Paeoniae Alba) nourishes yin and harmonizes the internal, all as the minister drugs;Zhi Shi(Fructus Aurantii Immaturus) andHou Pu(Cortex Magnoliae Officinalis) can descend qi and unblock stasis, thus helping promote defecation, with honey to moisturize intestines, together as the assistant drugs. The pill consisting of the above herbs functions to moisturize intestines and reduce heat, activate qi flow and promote defecation.
This study shows that acupuncture plus medication can produce a more significant therapeutic efficacy than use ofMa Zi Renpill alone in treating post-stroke constipation. This treatment is effective and safe with few adverse effects, and thus is worthy of promotion in clinic.
Conflict of Interest
The authors declared that there was no conflict of interest in this article.
Acknowledgments
This work was supported by the Affiliated Hospital of Hebei United University.
Statement of Informed Consent
All of the patients in the study signed the informed consent.
[1] Liu AW, Wu QM, Li XR, Tan T, Shi XH, Li L. Therapeutic observation of electroacupuncture for post-stroke constipation. Zhenjiu Linchuang Zazhi, 2008, 24(9): 17-18.
[2] Liu M. Clinical research progress of cerebrovascular diseases. Zhonghua Yixue Xinxi Daobao, 2002, (14): 21-22.
[3] Chinese Neuroscience Society, Chinese Neurosurgical Society. Key diagnostic points for cerebrovascular diseases. Zhonghua Shenjingke Zazhi, 1996, 29(6): 379-380.
[4] Maron BJ, Towbin JA, Thiene G, Antzelevitch C, Corrado D, Arnett D, Moss AJ, Seidman CE, Young JB, American Heart Association; Council on Clinical Cardiology, Heart Failure and Transplantation Committee, Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups, Council on Epidemiology and Prevention. Contemporary definitions and classification of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation, 2006, 113 (14): 1807-1816.
[5] State Administration of Traditional Chinese Medicine. Criteria of Diagnosis and Therapeutic Effects of Diseases and Syndromes in Traditional Chinese Medicine. Nanjing: Nanjing University Press, 1994: 11.
[6] Ministry of Health of the People’s Republic of China. Guiding Principles for Clinical Study of New Chinese Medicines. Beijing: China Medico-Pharmaceutical Science & Technology Publishing House, 2002: 131.
[7] Wu YM, Wu XM, Ding WT, Zhang B, Ma L. Clinical observation of electroacupuncture plus iontophoresis to Tianshu (ST 25) for post-stroke constipation. Zhongguo Linchuang Yisheng, 2013, 41(11): 63-67.
[8] Li SY, Xie HW. Nursing of constipation in patients with intracranial hypertension. Qilu Yixue Zazhi, 2001, 16(4): 314.
[9] Feng XZ, Huang CY, Su HD. Observation and intervention of elderly constipation treated with massage around umbilicus. Hushi Jinxiu Zazhi, 2005, 20(4): 347-348.
[10] Wang DS, Wang S, Kong LL, Wang WY, Cui XM. Clinical observation on abdominal electroacupuncture for treatment of poststroke constipation. Zhongguo Zhenjiu, 2008, 28(1): 7-9.
[11] Liao WF, Zhang H. Discussion of Tianshu (ST 25). Zhongyi Zhongyao, 2007, 4(4): 166-167.
[12] Huang QF. Metrological analysis and evaluation of acupuncture-moxibustion treatment for constipation in modern literature. Liaoning Zhongyi Zazhi, 2009, 36 (3): 368-369.
[13] Ni HP. Effect observation of treating elderly constipation by massage. Zhongyi Linchuang Yanjiu, 2011, 3(21): 101-102.
[14] Luo L, Wang J, Ren YL, Lu SF, Yu SG. Study on ancient classic acupuncture points combination in treating stroke. Chengdu Zhongyiyao Daxue Xuebao, 2010, 33(4): 1-4.
Translator:Hong Jue
R246.1
: A
Date:June 10, 2014
杂志排行
Journal of Acupuncture and Tuina Science的其它文章
- Therapeutic Observation on Tuina plus Electroacupuncture for Lateral Humeral Epicondylitis
- Comparative Study on the Analgesic Effects of Different Moxibustion Methods with Tai-yi Moxa Stick in Treating Primary Dysmenorrhea
- Clinical Analysis of Acupuncture Combined with Tuina in Treating Cervical Vertigo
- Warm Needling Combined with Iontophoresis of Chinese Medicine for Temporomandibular Joint Disorder
- Effect of Electroacupuncture Combined with Tuina on Lumbar Muscle Tone in Patients with Acute Lumbar Sprain
- Observation on Clinical Effects of Acupotomy plus Cupping for Knee Osteoarthritis
