Acupuncture for low back pain: a clinical practice guideline from the Hong Kong taskforce of standardized acupuncture practice
2022-11-17CHENHaiyongYEUNGWingFaiYANGMingxiaoMUJinglanZIEATatChiNGBaconFungLeungLAOLixing
CHEN Haiyong,YEUNG Wing-Fai,YANG Mingxiao,MU Jinglan,ZIEA Tat-Chi,NG Bacon Fung-Leung,LAO Lixing
CHEN Haiyong,School of Chinese Medicine,University of Hong Kong,Hong Kong SAR,China
YEUNG Wing-Fai,School of Nursing,Hong Kong Polytechnic University,Hong Kong SAR,China
YANG Mingxiao,Bendheim Integrative Medicine Center,Memorial Sloan Kettering Cancer Center,1429 First Avenue,New York 10021,USA
MU Jinglan,Department of Anesthesiology,Nanjing Drum Tower Hospital,Nanjing University Medical School,Nanjing,210008,China
ZIEA Tat-Chi,NG Bacon Fung-Leung,Chinese Medicine Department,Hong Kong Hospital Authority,Hong Kong SAR,China LAO Lixing,Virginia University of Integrative Medicine,Fairfax,VA 22031,USA
Abstract OBJECTIVE: To develop a clinical practice guideline to guide the treatment of low back pain by acupuncture.METHODS: An integrative approach of systematic review of literature,clinical evidence classification,expert opinion surveying,and consensus establishing via a Delphi program was utilized during the developing process.Both evidence-based practice standards and the personalized features of acupuncture were taken into considerations.RESULTS: Based on clinical evidence and expert opinions,we developed a clinical practice guideline for the treatment of low back pain with acupuncture.These recommendations have a wide coverage spanning from Western Medicine diagnosis and Traditional Chinese Medicine syndrome differentiation,to acupuncture treatment procedures,as well as post treatment care for rehabilitation and follow-ups.The recommendations for acupuncture practice included treatment principles,therapeutic regimens,and operational procedures.The levels of evidence and strength of recommendation were rated for each procedure of practice.CONCLUSION: A clinical practice guideline for acupuncture treating low back pain was developed based on contemporary clinical evidence and experts′consensus to provide best currently agreeable practice guideline for domestic and international stakeholders.
Keywords: acupuncture;low back pain;diagnosis;syndrome differentiation;rehabilitation;practice guideline
1.INTRODUCTION
Low back pain (LBP) is characterized as pain localized at the lumber area and radiates to the general low back and abdominal area.In Hong Kong,an estimated 57.1%of the population has suffered from LBP at least once and 42.1% at least once within the past year.1In the U.S.,the prevalence of LBP is rising from 3.4% to 10.2% during 1992 and 2006 with increased medical demands and economic costs.2The recurrence rate one year after the symptomatic resolution of an episode is as high as 25%.3Over one third cases epidemically develop into persistent LBP.4Current treatment strategies include education and reassurance,analgesic medicines,non-pharmacological therapies,and timely review,with a focus of treatment on the pain management.5
Acupuncture is used as alternative treatment for patients with LBP globally.Clinical trial showed that acupuncture is effective to reduce pain and improve physical activity.6Meta-analysis of individual patient data confirmed the analgesic effect of acupuncture.7As one of the major tools for fighting against opioid epidemics in the States,acupuncture is being accepted as a powerful,evidence-based,cost-effective and safe treatment for pain and other conditions.8Many national clinical guidelines of western medicine extensively recommend acupuncture for LBP management.Despite all,how acupuncture should be conducted by practitioners and used by patients in clinical practice has not been addressed.Lacking step-by-step guidance for clinical practice represents a major clinical challenge for the delivery of acupuncture treatment for patients with LBP.As such,current acupuncture practice diversifies due to evidence-based and standardized practice guideline.Those issues are associated with concerns about the sufficiency of treatment delivery and its safety.As such,the Hospital Authority of Hong Kong launched a project to develop the clinical practice guideline (CPG)of acupuncture for treating low back pain and commissioned the School of Chinese Medicine of The University of Hong Kong to undertake the work.The guideline development committee,called the Hong Kong Taskforce of Standardized Acupuncture Practice,was formed by a panel of experts in epidemiology,clinical medicine,evidence-based medicine and acupuncture.During the development process,evidence from valid clinical trials and traditional values of syndrome differentiation and treatment that are deemed essential to acupuncture were comprehensively reviewed and utilized as raw material to develop the clinical practice guideline.
2.METHODS
According to the development protocol of the previous Chinese medicine CPGs launched by the Hospital Authority of Hong Kong,9,10the process consists of preparation,development,and finalization phases.The preparation phase consists of forming the committee and settling on the schedule,the methods,and tools.The development phase comprises a literature search and a systematic review,as well as text mining in acupuncture classics and modern textbooks;consultation with the experts for their clinical experience;drafting of the first CPGs;and investigating their applicability to local registered acupuncturists.In the finalization phase,by means of a consensus conference,the committees finalize,implement,and publish the CPGs.The development committee,convened by L Lao,included 11 experts in the areas of acupuncture,clinical research,and evidence-based medicine.
2.1.Development committee
The development committee was composed of a steering panel and working panel.A steering panel of eight acupuncture experts from Hong Kong and China supervised the development process and advised on key issues.The working panel,including acupuncturists (Lao Lixing,Chen Haiyong,Yeung Wing-Fai,Yang Mingxiao) and clinical researchers and experts of evidence-based medicine (Chen Haiyong,Yeung Wing-Fai,Yang Mingxiao,Mu Jinglan),conducted the specific studies following the development protocol.The committee members were shown in the Supplementary Material 1.
2.2.Developmental methods and procedures
The evidence-grading system for TCM research,11which had been used in previous Hong Kong TCM CPGs,was adopted (Table 1).We also referred to the guideline developer’s handbook published by Scottish Intercollegiate Guidelines Network (SIGN)12for related issues.(See Supplementary Material 2 for details)
3.RESULTS
Through this study,we have developed the CPGs with clinical recommendations for acupuncture treatment of LBP,with a wide coverage spanning from western medicine diagnosis and Traditional Chinese Medicine(TCM) Syndrome Differentiation,to treatments as well as rehabilitation and follow-up recommendations.The executive summary is listed in the Supplementary material 2 &3,and the overall recommendations are visualized in Figure 1.In current version of guidelines,acupuncture refers to the needling treatment based on the theory of TCM.

Figure 1 .Recommendations on Diagnosis and Acupuncture Treatment Procedure for Low Back Pain.
3.1.Diagnosis for LBP
LBP refers to pain and discomfort localized between the lower rib and the inferior gluteal folds.Nonspecific LBP is defined as pain in the lower back area not attributable to a recognizable or known specific pathology (e.g.,infection,tumor,osteoporosis,lumbar spine fracture,structural deformity,inflammatory disorder,radicular syndrome,or cauda equina syndrome).13Nonspecific LBP is classified into acute (≤ 3 months) and chronic pain (> 3 months),according to the amount of time the person has suffered.13
3.2.Syndrome differentiation
This study formed a TCM syndrome differentiation roadmap for acupuncture treatment of LBP (Supplementary Material 4).In TCM,both TCM etiology-based diagnosis and meridian-based syndrome differentiation are permitted to use for the identification of a TCM syndrome of LBP.It is noteworthy that the TCM syndrome differentiation of LBP depends on traditional theories and clinical experience.The grade of recommendation and level of evidence are relatively low(Grade of Recommendation: C,Level of Evidence: IV.Shorted as C,Ⅳ.Same as follows).The grade system was shown in Table 1.
3.3.Exclude LBP Not Suitable for Acupuncture Treatment
The LBP assessment form shown in the Supplementary material 5 is recommended to assist further exclusion of the unsuitable conditions (C,Ⅳ).Patients with bleeding disorder and other severe visceral diseases are deemed inappropriate for acupuncture treatment.Written informed consent should be obtained prior to the performance of acupuncture.Moreover,patient with LBP that is secondary to any form of severe spinal or systematic pathology may consider acupuncture as a complementary treatment.
3.4.Clinical practice paradigm of acupuncture in treating LBP
An evidence-based recommendation of acupuncture formula is shown in Table 2.Patients should be informed about the effect,in addition to possible side effects,14and daily care.Acupuncturists are recommended to continue monitoring the vital signs,if necessary,during acupuncture treatment (C,Ⅳ).Acupuncturists are also recommended to apply clean needle techniques (A,Ib).15(a) Acupuncture practice paradigm for acute LBP or acute episode of chronic LBP

Table 1 Level of Evidence and Strength of Recommendations for TCM CPGs
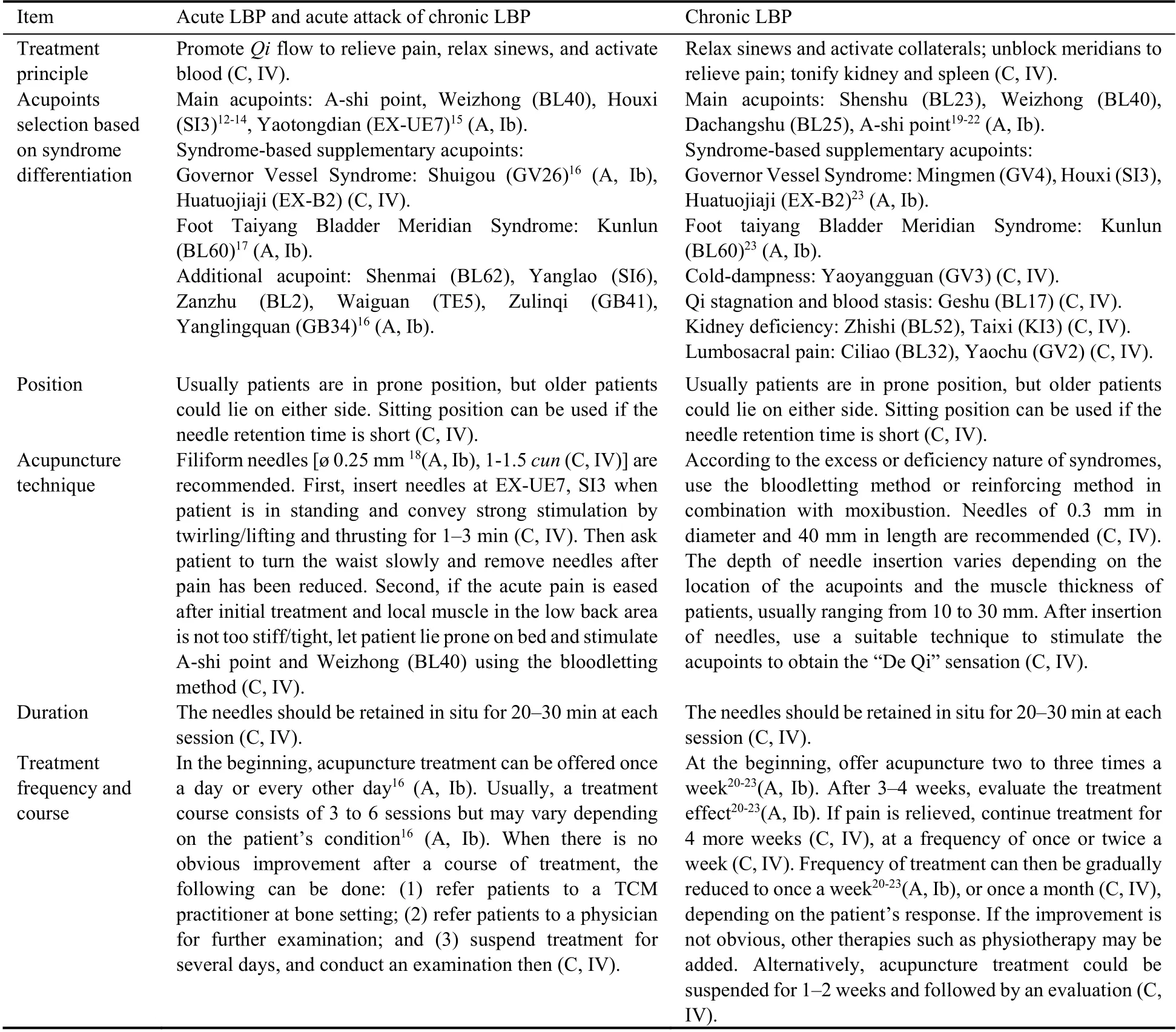
Table 2 Roadmap of recommended practice of acupuncture treatment for low back pain (LBP)
Goal and Treatment principle: For acute attacks of LBP,the primary treatment goal is to immediately alleviate pain and maximally restore patient’s physical function.The basic treatment principle is to promoteQicirculation to relieve pain,relax sinews,and activate blood (C,Ⅳ).Acupuncture treatment procedures: patients can either keep a prone/ sitting position or lie on either side (C,Ⅳ).Filiform needles with diameter of 0.25 mm16(A,Ib)and lengths of 1-1.5cun(C,Ⅳ) are recommended.First,motion-style acupuncture treatment can be used.Ask the patient to stand,and then insert needles at Yaotongdian [also named Yaotongxue,(EX-UE7)]and/or Houxi (SI3) and stimulate the acupoints strongly by twirling or lifting and thrusting for 1-3 min (C,IV).At the same time,ask the patient to turn the waist slowly.Remove the needles after the pain has been reduced.Second,if the acute pain has eased after the initial treatment and the local muscle in the low back area is not too stiff and tight,then let the patient lie prone on the bed and stimulate the tenderness point at the lumbar region and Weizhong (BL40) using the draining methodbut should avoid using strong thrusting and lifting technique (C,IV).The depth of the needle could vary within a range of 0.5-1.2cun,depending on the acupoints’location and body size(C,IV).The treatment of acupuncture for acute LBP was reported by a highquality randomized controlled trial.16In this study,patient was asked to walk with two assistants on each side while the needles at points GV16,LI11 and LV2 in situ.However,more than 50% of Delphi members commented that this regimen does not suit local settings for acupuncture practice,as most of them would not have sufficient workforce to have two assistants to support the patient while the patient is walking.The needles will be retained in situ for 20-30 min at each session (C,IV).
Treatment frequency and course: In the beginning,acupuncture treatment can be offered once a day or every other day(A,Ib).17Usually,a treatment course consists of three to six sessions but may vary depending on the patient’s response to the treatment (A,Ib).17
Recommended concurrent therapies: In order to strengthen the effect of acupuncture for acute LBP attacks,other forms of acupuncture related therapy can be used in combination.Consider applying an electric stimulation with a continuous wave at about 2-6 Hz,or a dense-disperse wave with an alternating frequency of 2 Hz/15 Hz.A continuous wave at 40 Hz and 20 mA current (C,IV) could also be used for 20 min after eliciting the “DeQi” sensation on the acupuncture points(A,Ib).According to animal studies,18clinical practitioners are encouraged to adopt an alternative 2/100 Hz electroacupuncture frequency to potentiate the analgesic effect.In addition to acupuncture,cupping could be performed at the lumbar region.Different sizes of cups should be chosen with reference to the area of the acupoints.If cupping is not appropriate because of severe muscle tension,bloodletting could be performed.For sudden severe LBP attacks,consider using a three-edged needle for bloodletting at the Weizhong (BL40) points(A,Ib),or using a plum-blossom needle for bloodletting at the local area;perform cupping on the local area to facilitate bloodletting.The cupping plus bloodletting therapy can be used for the emergent relief of acute attack of LBP.However,patient’s body constitution should be considered before initiation of treatment and its use will be stopped whenever the acute symptoms is relieved (C,IV).
Precautions for safe acupuncture practice:In addition,acupuncture therapy is safe when it’s properly conducted by qualified practitioners.19It is recommended that during the treatment process acupuncture practitioners should pay attention to the patient’s reaction to the insertion of needles and side effects,such as pain at needling site or weakness of body and minor bruising (A,Ib).17
(b) Clinical practice paradigm of acupuncture in treating chronic LBP
Goal and Treatment principle: Chronic LBP always have a long-term disease course and is associated with relative low-level recurrent pains that affect patient’s physical function and life quality.The aim of acupuncture treatment at this stage is to reduce the frequency and intensity of pain attacks,maximize physical function and increase patient’s quality of life.The treatment principle of acupuncture is to relax sinews and activate collaterals,unblock meridians to relieve pain,tonify kidney and spleen (C,IV).
Acupuncture treatment procedures: Patients are in a prone position,but older patients could lie on either side.Sitting position can be used if the needle retention time is short (C,IV).According to the excess or deficiency nature of syndromes,use the draining method or supplementation method in combination with moxibustion.Needles of 0.3 mm in diameter and 40 mm in length are recommended.The depth of needle insertion varies depending on the location of the acupoints and body size,usually ranging from 10 to 30 mm.After insertion of needles,use a suitable technique to stimulate the acupoints to obtain the “DeQi”sensation (C,IV).The needles should be retained in situ for 20-30 min at each session (C,IV).
Treatment frequency and course:at the beginning,offer acupuncture two to three times a week (A,Ib).20-23After 3-4 weeks,evaluate the treatment effect (A,Ib).20-23If pain is relieved,continue treatment for 4 more weeks,(C,IV) at a frequency of once or twice a week (C,IV).Frequency of treatment can then be gradually reduced to once a week (A,Ib),20-23or once a month (C,IV),depending on the patient’s response.If the improvement is not obvious,other therapies such as physiotherapy may be added.Alternatively,acupuncture treatment could be suspended for 1-2 weeks and followed by an evaluation (C,IV).Many studies have adopted semi-standardized23-25or standardized acupuncture protocols,26,27and a number of trials have administered 7-to 12-session treatments for chronic nonspecific LBP.6,25,27,28
Recommended concurrent therapies:consider applying electric stimulation with a continuous wave at about 2-6 Hz or a dense-disperse wave with an alternating frequency of 2 Hz/15 Hz,or a continuous wave at about 10-20 Hz at the ends of needles in most painful acupoints(C,IV).For patients with cold-dampness and kidney deficiency,direct and indirect moxibustion,such as suspended moxibustion and moxibustion through aconitum (Fuzi) or ginger,could be performed.Direct moxibustion could be conducted on Shenshu (BL23),Zusanli (ST36),Mingmen (GV4),Yinlingquan (SP9),and the A-shi point.The burning moxa stick should be held 3-4 cm away from the acupoints and moved along the meridian until the skin becomes warm and slightly red but not burning.Recommend 15-20 min per session(C,IV).The moxibustion treatment could be performed following each acupuncture needling treatment or alternated with acupuncture needling treatment.For LBP due to blood stasis,warm needling followed by cupping is suggested.It could be performed on four to six selected acupoints from the following: Shenzhu (BL23),Mingmen (GV4),Dachangshu (BL25),Yaoyan (EX-B7),Yaoyangguan (GV3),Huatuojiaji (EX-B2),and the Ashi point.After needle removal,cupping could be performed on the selected acupoints for 5-10 min.“Slide cupping” along the bladder meridian could also be considered.Alternatively,the plum-blossom needling technique for bloodletting followed by cupping could also be considered (C,Ⅳ).Other than body acupuncture,auricular acupuncture could be applied to enhance the effect of treatment by inserting filiform needles on auricular acupoints such as the lumbosacral vertebrae,kidney,and Shenmen.During needle retention time,ask the patient to stand and move his/her waist.Vaccaria seeds instead of needles could also be used (C,IV).
Precautions for safe acupuncture practice:Be cautious about the following side effects: minor bleeding,weakness,dizziness,muscle twitches,stuck needle,headache,dry mouth,pain and bruising in the sites at which the needles were inserted,and pain or numbness in the legs(A,Ib).15
3.5.Recommendations for Posttreatment Care (C,IV)
3.5.1 Posttreatment Care for Acute LBP
Help patients establish a positive attitude toward their recovery.
Encourage bed rest;recommend self-acupressure on the pain sites in the lower back.
Recommend increasing exercise gradually,protecting the low back muscles against injury.
Advise patients to try physiotherapy or see doctors if the LBP becomes worse.
3.5.2 Posttreatment Care for Chronic LBP
Help patients establish a positive attitude toward their recovery.
Recommend mind/body exercises such asTaichi quan,Baduanjin,and self-acupressure on the pain sites in the lower back.
Advise patients to keep the low back warm and correct the working position.
Recommend Chinese herbs as prescribed by registered Hong Kong traditional Chinese pharmacists.
Recommend physiotherapy or seeing doctors if the pain repeatedly occurs.
4.DISCUSSION
This is the first edition of CPGs for acupuncture for LBP treatment in Hong Kong.The guidelines focus on diagnosis,syndrome differentiation,and treatment protocol including common supplementary therapies.The Delphi approach was adopted to investigate the applicability among local acupuncturists,and an agreement rate of 80% was finally reached.This is the strength of the present CPGs that the work efficiently converged the opinions from involved local registered acupuncturists.
Evidence-based medicine emphasizes the use of current best available evidence in guiding clinical practice,which is a key solution to standardize the delivery of medicine and diminish difference in efficacy.However,the evidence that justifies acupuncture treatment for LBP is not sufficient.When good quality evidence is insufficient,the rule of thumb may be applied and evidence from other sources are available to use for the formation of CPGs of acupuncture treating LBP.Acupuncture is a practice-based therapy which has been used in China and other Asian countries for a long history.There are numerous medical records preserved and many medical compilations developed.Those literatures,though not a source of best evidence available,provide empirical knowledge-and experience-based evidence.Moreover,there are plenty of observational studies in acupuncture treating LBP.Those studies are nevertheless not flawless from the perspectives of evidence-based medicine but are still a source of real-world evidence that can be used to assist clinical decision making,if properly used.It is obvious that the current form of CPGs is not stationary,because new evidence emerges as time goes by.The CPGs will be updated every 5 years or immediately at the time when solid evidence that is able to change current practice is indicative.
The CPGs have wide potential applications.Acupuncturists should consider prioritizing items supported by higher quality evidence over those supported by only weak evidence when developing an acupuncture protocol for individual patients.For example,for acute nonspecific LBP,there is high-quality evidence with the strong recommendation that acupuncture can be offered once a day or every other day,with a course of three to six sessions (Figure 1,Table 2).Acupuncturists can administer the treatment at the suggested frequency within the course if no contraindications are found.For other items,such as syndrome differentiations and a couple of associated acupoints chosen either for acute or chronic LBP,there has been no research published concerning those components.The related recommendations were graded low with weak recommendations,as they were based on the results of text mining,experience of the experts,and the subsequent consensus of 13 local acupuncturists.
The other promising sides of using those CPGs include dismissing geographical disparity on clinical practice,promoting evidence-informed education of acupuncture,providing safety assurance and potentiating the implementation of integrative medicine.Firstly,geographical disparity in the understanding and practice of the basics of acupuncture is prevalent.In different areas of China,different schools of acupuncture have different recognitions towards the stimulation parameters of acupuncture for improving LBP.The CPGs with evidence backups by clinical trials offer generalized information to guide the acupuncture procedures and will exert positive influences on resolving those differences.Second,lecture-based learning is prevailing in the education of TCM and the teaching materials are made of ancient books and expert experiences.To introduce evidence-based practice into the education of acupuncture is essential,for it helps to evolve the practice of acupuncture.Third,acupuncture is one of the pioneer therapies that gear up the development of integrative medicine.With evidence-based standards and guidelines,acupuncture will no longer be caged with limited use.It provides unique opportunities for acupuncture to communicate with western medicine in an integrative medicine environment.Furthermore,this guideline may also be used as a reference for those who design clinical trials on acupuncture for LBP,while the results of these trials could enhance the level of strength of the evidence for future guidelines.
In order to catch up with latest evidence and adhere to the up-to-date guideline developing methodology,several key factors are required to be considered with more perspective visions.Firstly,this study is limited that the GRADE system or other systems were not employed due to the lack of sufficient clinical evidence.With evidence mounting up in future,the update work (5 or 10 years hereafter) should adopt the well-accepted evidence-grading models,such as the GRADE system,or the Levels of Evidence system from the Oxford Centre for Evidence-based Medicine (the Oxford grading system).At this stage,a common drawback is the lack of clinical evidence for formulating recommendations.Following the advice from our expert panel,we employed a practical model which is adjusted from the Oxford grading system and the SIGN code.This model has been used by a WHO-initiated program in the development of 5 acupuncture CPGs and 28 Chinese medicine CPGs.29Secondly,the updated guidelines should be more patient group-oriented and be tailored to meet the specific needs of different patient groups,such as pregnant women with LBP or elder people with chronic LBP.30As available evidence was not categorized according to patient groups,the current CPGs should be considered applicable to the general population.Providing instructions of LBP management with more details including age,sex,comorbidity and other special conditions,in the updated version will considerably enrich the CPGs and facilitates its clinical utilizations across disciplines.
The present CPGs were developed using an evidencebased and consensus-reached approach to provide the best currently agreeable clinical practice guidelines for all stakeholders in Hong Kong and other areas.
5.ACKNOWLEDGEMENTS
We sincerely thank Dr.Andrea Furlan,from the Department of Medicine at the University of Toronto,who gave constructive comments to improve the quality of the manuscript.The authors also would like to thank Ms.Lam Wing Lok,a graduate of the School of Chinese Medicine at University of Hong Kong,for the language editing in the treatment protocol.
杂志排行
Journal of Traditional Chinese Medicine的其它文章
- Flavonoids from traditional Chinese herbs for diabetes in rats: a network Meta-analysis
- In-vitro and in-vivo pharmacological screening of Iris albicans
- Detailed approach toward the anti-hyperglycemic potential of Sterculia diversifolia G.Don against alloxan-induced in vivo hyperglycemia model
- Efficacy of Bushen Culuan decoction (补肾促卵方) on ovarian follicle and follicular granulosa cells in mice with premature ovarian insufficiency induced by tripterygium wilfordii polyglycoside
- Efficacy of Wumei Baijiang prescription (乌梅败酱方) on regulatory T cells/ helper T cells Immune balance in mice with ulcerative colitis
- Shenweifang-containing serum inhibits transforming growth factorβ1-induced myofibroblast differentiation in normal rat kidney interstitial fibroblast cells
