GBS培养联合阴道假丝酵母菌检测预测足月前胎膜早破的价值研究
2019-06-04邱海凡潘圆圆王连云华莹
邱海凡 潘圆圆 王连云 华莹


[摘要] 目的 探討B族链球菌(GBS)及外阴阴道假丝酵母菌病(VVC)联合检测用于预测未足月胎膜早破(PPROM)的价值。 方法 选取2016年8月~2017年8月我院收住的符合入选标准的PPROM孕妇227例为观察组,入院后立即行GBS培养、阴道假丝酵母菌检测;随机选取同期足月正常分娩的孕妇743 例为对照组,于妊娠35~37周进行GBS培养、阴道假丝酵母菌检测;并记录两组孕妇年龄、孕周、体重指数、孕次、产次等一般资料。观察两组孕妇GBS及VVC的阳性率及两者之间的关系。 结果 两组孕妇的基本资料比较,差异无统计学意义(P>0.05);227例PPROM孕妇中,GBS阳性率为9.69%,明显高于对照组的5.11%,且差异有统计学意义(P<0.05);观察组VVC阳性率为25.11%,明显高于对照组的18.71%,且差异有统计学意义(P<0.05);VVC阳性组孕妇GBS阳性率9.69%高于VVC阴性组5.30%,且差异有统计学意义(P<0.05)。 结论 GBS或VVC阳性均可增加PPROM发生的风险,有必要在妊娠35周前常规行GBS筛查及VVC检测来预测PPROM发生的风险,并对阳性者进行治疗。
[关键词] B族链球菌;外阴阴道假丝酵母菌病;预测;未足月胎膜早破
[中图分类号] R714.433 [文献标识码] B [文章编号] 1673-9701(2019)10-0072-04
Study on the value of GBS culture combined with candida vaginalis detection for predicting preterm premature rupture of membranes
QIU Haifan PAN Yuanyuan WANG Lianyun HUA Ying
Department of Obstetrics and Gynecology, Second Affiliated Hospital of Wenzhou Medical University, Wenzhou 325027, China
[Abstract] Objective To investigate the value of combined detection of group B streptococcus(GBS) and vulvovaginal candidiasis(VVC) for predicting preterm premature rupture of membranes(PPROM). Methods A total of 227 pregnant women with PPROM who were hospitalized from August 2016 to August 2017 were selected as observation group. Immediately after admission, patients were given GBS culture and detection of Candida vaginalis. 743 cases of pregnant women with term delivery in the same period were randomly selected as the control group, and were given GBS culture and detection of Candida vaginalis at 35-37th week of pregnancy. General data such as age, gestational weeks, body mass index, pregnancy time, and parity of the two groups were recorded. The positive rates of GBS and VVC and the relationship between them were observed. Results There was no significant difference in the basic data between the two groups(P>0.05). Among the 227 pregnant women with PPROM, the positive rate of GBS was 9.69%, which was significantly higher than that of the control group(5.11%), and the difference was statistically significant(P<0.05). The positive rate of VVC in the observation group was 25.11%, which was significantly higher than that in the control group(18.71%), and the difference was statistically significant(P<0.05). The positive rate of GBS in pregnant women with positive VVC was 9.69%, higher than that in those with negative VVC, and the difference was statistically significant(P<0.05). Conclusion Positive GBS or VVC can increase the risk of PPROM. It is necessary to routinely perform GBS screening and VVC testing before 35 weeks of gestation to predict the risk of PPROM and treat the patients with positive results.
[Key words] Group B Streptococcus; Vulvovaginal candidiasis; Prediction; Premature rupture of membranes before term
未足月胎膜早破(preterm premature rupture of me-mbranes,PPROM)是指在妊娠20周以后、未满37周在临产前发生的胎膜破裂。B 族溶血性链球菌(group B streptococcus,GBS)正常寄居于阴道和直肠,属于条件致病菌。研究认为,GBS定植可能增加胎膜早破、新生儿感染等发生率[1]。但也有研究显示,胎膜早破与是否GBS定植无明显相关性[2]。另有研究发现,外阴阴道假丝酵母菌病(vulvovaginal candidiasis,VVC)可引起胎膜早破、早产等。而对GBS感染人群的研究分析认为,VVC可能是GBS定植的独立危险因素[3]。本研究回顾性分析2016年8月~2017年8月在温州医科大学附属第二医院产科分娩的部分孕产妇的GBS定植及VVC发病情况,旨在探讨GBS定植及VVC与PPROM的相关性研究及孕35周之前的GBS及VVC联合检测对PPROM是否有预测作用。
1 资料与方法
1.1 一般资料
选取2016年8月~2017年8月在温州医科大学附属第二医院产科分娩的部分孕产妇作为研究对象。根据未足月胎膜早破(PPROM)诊断标准入选227例孕妇为观察组,年龄20~43岁,平均28.75岁,平均孕周(33.27±3.59)周,其中初产妇117例,经产妇110例;同期足月正常分娩的孕妇743例为对照组,年龄21~45岁,平均29.12岁,平均孕周(38.17±2.25)周,其中初产妇386例,经产妇357例。两组孕妇基本资料具有可比性(P>0.05)。见表1。
入选标准:①单胎头位妊娠;②无妊娠合并症及并发症;③孕周核对准确无误;④标本采集前1周内未使用抗生素;⑤标本采集前1周内未使用阴道栓剂;⑥知情同意,自愿受试,观察资料完整。排除标准:①不符合纳入标准者;②羊水过多者;③宫颈机能不全者;④不同意参加本研究者。
1.2 方法
1.2.1 检查时间 观察组(PPROM)227例孕妇,入院后立即行GBS培养、阴道假丝酵母菌檢测;对照组743 例于妊娠35~37周行GBS培养、阴道假丝酵母菌检测;并记录两组孕妇年龄、孕周、体重指数、孕次、产次等一般资料。
1.2.2 标本采集 严格按照《围产期GBS筛查与预防指南》中的方法进行样本采集:先擦去外阴过多的分泌物,将1 根无菌棉拭子置阴道下1/3 内旋转1周取阴道分泌物,再将另外1根插入肛门,在肛门括约肌上2~3 cm处轻旋取直肠分泌物。2根棉拭子取材后置于2根无菌试管中,密闭立即送检,用于GBS培养,其中任一阳性,即诊断为GBS定植。另用窥阴器扩张阴道,用1根无菌棉拭子取阴道后穹窿及侧壁的分泌物,取材后置于无菌试管中,用于假丝酵母菌检测。
1.2.3 GBS培养 将标本接种到5%的羊血琼脂平板上,置5% CO2环境中培养24~48 h,挑取β溶血的可疑菌落进行纯培养后,做涂片进行革兰染色镜检,镜下形态为革兰阳性球菌,呈链状排列,触酶试验阴性确定为链球菌属,判断为GBS 阳性。
1.2.4 假丝酵母菌检测 将标本接种到玻片上,用10%氢氧化钾溶液湿片后镜检,找到芽生孢子或假菌丝,确诊VVC阳性,未找到芽生孢子或假菌丝,则为VVC阴性。
1.3 统计学处理
本实验所有数据用SPSS20.0软件进行统计分析,计数资料采用χ2检验,P<0.05表示差异有统计学意义。
2 结果
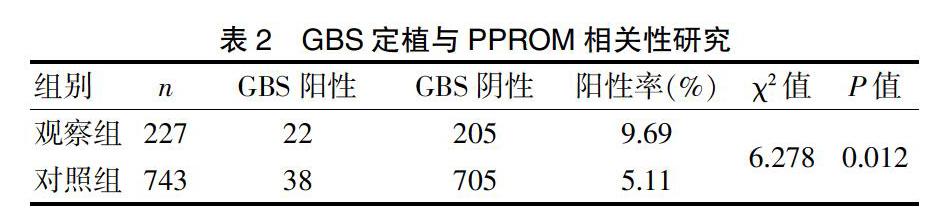
2.1 GBS定植与PPROM相关性研究
227例PPROM组孕妇中GBS定植者有22例,阳性率为9.69%,高于正常足月分娩的孕妇(5.11%),且结果有显著性差异(P<0.05)。见表2。
2.2 VVC与PPROM相关性研究
227例PPROM组孕妇中VVC阳性者有57例,患病率达25.11%,高于正常足月分娩者(18.71%),且有显著性差异(P<0.05)。见表3。
2.3 VVC阳性与GBS定植相关性研究
观察组与对照组中共有VVC阳性孕妇196例,其中GBS阳性者有19例,阳性率为9.69%,高于VVC阴性组的阳性率5.30%,且有显著性差异(P<0.05)。见表4。
3讨论
未足月胎膜早破(PPROM)是产科面临的一大难题,可引起早产、胎盘早剥、羊水过少、脐带脱垂、胎儿窘迫和新生儿呼吸窘迫综合征等,孕周越小,围产儿预后越差,可导致孕产妇及胎儿感染率和围产儿病死率显著升高[4]。
感染是造成PPROM的重要原因,而GBS已被证实为围生期母婴感染的主要致病菌之一[5,6]。GBS是β溶血性链球菌的一种,又称无乳链球菌,是兼性厌氧的革兰阳性链球菌,为条件致病菌。GBS一般寄生在人体下消化道或者泌尿生殖道中,在健康人群中带菌率高达20%~40%[7],在孕妇阴道直肠中的带菌率为10%~35%[8]。研究发现,GBS感染后,会引起磷脂酶A、前列腺素及细胞因子如肿瘤坏死因子、白细胞介素等的释放,刺激子宫收缩导致晚期流产及早产[9,10]。GBS感染上行至胎膜,通过炎症细胞的吞噬作用和细菌产生的蛋白水解酶的直接侵袭,使胎膜局部张力减低,从而导致胎膜早破,尤其是未足月胎膜早破[11]。孙雪梅等[12]对103例未足月胎膜早破孕妇的病因进行分析,发现生殖系统炎症尤其是GBS感染是导致PPROM的重要原因。但也有不少国内研究认为胎膜早破、早产等与孕妇GBS带菌没有明显的相关性[7,13,14]。本研究结果提示,PPROM组孕妇GBS阳性率(9.69%)明显高于足月正常分娩的孕妇(5.11%),说明GBS感染与PPROM的发生存在相关性。
外陰阴道假丝酵母菌病(VVC)属深部真菌性感染疾病,在女性中很普遍,有资料显示,80%以上的女性在其一生有过该病病史,且其中超过45%会反复发作[15]。酸性环境适宜假丝酵母菌生长,VVC患者的阴道pH值多在4.0~4.7,通常<4.5[16]。在妊娠期,由于孕妇机体免疫力下降,雌激素水平升高,阴道组织内糖原含量增加,酸度增高,从而导致VVC的发病率上升。
研究证实,孕妇生殖道感染后,阴道内的病原微生物可产生胶质酶和弹性蛋白酶,这些酶类均可降解胎膜的基质和胶质;病原微生物可减少宫颈IgA和IgG的活性,使黏蛋白酶活性增加,黏液分泌量减少,这些情况均增加胎膜早破发生率[17]。李琼芳等[18]研究发现,PPROM孕妇阴道内假丝酵母菌的感染率要显著高于对照组,Logistic回归分析说明VVC孕妇发生PPROM的风险是正常孕妇的6.218倍。本研究结果提示PPROM组孕妇的VVC发病率是25.11%,明显高于正常分娩孕妇的18.71%,与前述学者结论一致。
Alfei等[19]认为B族链球菌感染与外阴阴道假丝酵母菌病有一定的相关性,GBS 可抑制乳酸杆菌的生长,使阴道微生态失衡,有利于阴道假丝酵母菌的繁殖。王昕等[20]应用条件Logistic回归模型进行多因素分析,发现VVC可能是妊娠晚期GBS感染的一个独立危险因素。本研究发现VVC阳性组孕妇GBS阳性率明显高于VVC阴性组孕妇,且差异有统计学意义,与上述学者研究结果相符。
美国疾控中心防治指南建议对所有妊娠35~37周的孕妇进行GBS筛查。然而临床工作中发现有不少孕妇在妊娠35周之前就发生胎膜早破,这类人群未行GBS筛查,容易漏诊漏治,其母婴不良结局的风险更大。在本研究基础上,建议进行更大样本量的研究,来探讨在妊娠35周以前用GBS联合VVC的检测来预测PPROM发生的价值。并对阳性孕妇及时给予相应治疗,降低PPROM的发生率,降低围产儿感染率及病死率。
[参考文献]
[1] Tan Yujie,Hai Jujun,Zhang Chen,et al. Influence of genital tract infection with group B streptococcus in third trimester pregnant women on maternal and infant prognosis[J].Chinese Journal of Nosocomiology,2015,18(3):4279-4281.
[2] 孙丹华,李宣,杨翠芳,等.妊娠晚期B 族链球菌带菌状况分析及其对妊娠结局的影响[J].中国综合临床,2014, 30(7):764-767.
[3] Revised guidelines from CDC. Prevention of perinatal group B streptococcal disease[R]. MMWR,2010,59(10):1-32.
[4] Modi BP,Teves ME,Pearson LN,et al. Mutations infetal genes involved in innate immunity and host defense against microbes increase risk of preterm premature rupture of membranes(PPROM)[J].Mol Genet Genomic Med,2017,5(6):720-729.
[5] Verani JR,McGee L,Schrag SJ,et al. Prevention of perinatal group B streptococcal disease-revised guidelines from CDC,2010[J].MMWR Recomm Rep,2010,59(RR-10):1-36.
[6] Van Dyke MK,Phares CR,Lynfield R,et al. Evaluation of universal antenatal screening for group B streptococcus[J].N Engl J Med,2009,360(25):2626-2636.
[7] Li Xiaofang,Zhou Fengqin. Vaginal Candida infections at different pregnancy stage and its effect on pregnancy outcomes[J].The Chinese Journal of Human Sexuality,2016, 25(10):115-118.
[8] Yang Xiaolan,Li Juan,Wang Ping,et al. Clinical effect of perinatal pregnant women infected group B streptococcus on maternal and infant prognosis[J].Chin J Nosocomiol,2016,26(20):4698-4700.
[9] Stapleton RD,Kahn JM,Thomas MJ,et al. Risk factors for group B streptococcal genitourinary tract colonization in pregnant women[J]. Obstetric Gynecol,2005,106(6):1246-1252.
[10] Cagno CK,Pettit JM,Weiss BD. Prevention of perinatal group B streptococcal disease:Updated CDC guideline[J].Am Fam Physician, 2012,86(1):59-65.
[11] Turrentine MA,Colicchia LC,Hirsch E,et al. Efficiency of screening for the recurrence of antenatal group B streptococcus colonization in a subsequent pregnancy:A systematic review and meta-analysis with independent patient data[J].American Journal of Perinatology,2016, 33(5):510-517.
[12] 孫雪梅,田鹏,杨敏,等. 妊娠期未足月胎膜早破病因分析[J].现代生物医学进展,2016,16(13):2487-2489.
[13] 时春艳,曲首辉,董悦,等.妊娠晚期孕妇B族链球菌带菌状况的检测及带菌对妊娠结局的影响[J].中华妇产科杂志,2010,45(1):12-16.
[14] Santhanam S,Jose R,Sahni RD,et al. Prevalence of group B streptococcal colonization among pregnant women and neonates in a tertiary hospital in India[J].Journal of the Turkish German Gynecological Association,2017, 18(4):181-184.
[15] 张晓梅.外阴阴道假丝酵母菌感染分布及抗真菌药物敏感性分析[J].中国实验诊断学,2010,14(9):1465-1466.
[16] 刘魏,张旭,刘朝晖,等.时间、二相性、pH环境对白色假丝酵母菌药物敏感性的影响[J].现代妇产科进展,2011,20(1):30-34.
[17] Chmait RH,Chon AH,Korst LM,et al. Risks of preterm premature rupture of membranes and preterm birth post fetoscopy based on location of trocar insertion site[J].Am J Perinatol,2018,35(8):801-808.
[18] 李琼芳,胡传翠,李波,等.足月前胎膜早破的诊治分析[J].实用心脑肺血管病杂志,2012,20(3):454-455.
[19] Alfei A,Rizzo A,Cavanna C,et al. Candida glabrata and preterm premature rupture of membrane complicating in vitro pregnancy:Case report and confirmation of mother to neonate transmission[J].Arch Gynecol Obstet,2014, 290(2):211-214.
[20] 王昕,高玉东,张晓兰,等.妊娠B族链球菌感染人群分析及药物干预的影响[J].医学信息,2014,27(12):102-103.
