Serological investigation of lgG and lgE antibodies against food antigens in patients with inflammatory bowel disease
2019-03-14HaiYangWangYiLiJiaJiaLiChunHuaJiaoXiaoJingZhaoXueTingLiMeiJiaoLuXiaQiongMaoHongJieZhang
Hai-Yang Wang, Yi Li, Jia-Jia Li, Chun-Hua Jiao, Xiao-Jing Zhao, Xue-Ting Li, Mei-Jiao Lu, Xia-Qiong Mao,Hong-Jie Zhang
Abstract
Key words: Inflammatory bowel disease; Food-specific immunoglobulin G; Food intolerance
INTRODUCTION
Inflammatory bowel disease (IBD) is a chronic relapsing inflammatory disease of the gastrointestinal tract, which includes ulcerative colitis (UC) and Crohn’s disease (CD).Increasing evidence indicates that IBD results from an abnormal mucosal immune system triggered by environmental factors[1,2].
Various environmental factors such as environmental pollution, smoking, stress and foods[3-6]are thought to induce or aggravate IBD.Of these factors, diet is considered to contribute to the course of IBD[7].A multicenter case-control study in Japan found that sweets, fats, including monounsaturated and polyunsaturated fatty acids, soil, fish and shellfish were positively associated with IBD risk[8].Another study showed that increased consumption of alcohol or red meat was associated with an increased probability of relapse in UC patients[9].Two large prospective cohort studies in Japan and Europe verified that high consumption of n-6 polyunsaturated fatty acids may aggravate IBD by altering the fatty acid composition of the cell membrane and immunomodulating leukotrienes and prostaglandins[10,11].Studies have shown that food intolerance may be involved in this process[12].Some food antigens are thought to be involved in the formation and development of human chronic intestinal inflammatory diseases in genetically susceptible patients[13,14].
Food allergy and food intolerance are two types of adverse reactions to food.Food allergy is typically mediated by immunoglobulin E (IgE) antibodies, which produce an immediate and sometimes life-threatening response, the most well-known being type 1 food allergy to peanuts or shellfish.The immune system mounts an attack against normally harmless food ingredients.In contrast, food intolerance is mediated by immunoglobulin G (IgG) antibodies, and the underlying mechanism may be the stimulation of neutrophils or other cells in the innate immune system, creating a complex clinical course.Food intolerance significantly contributes to IBD patients’symptoms.The advantages of removing certain foods from the daily diet have been a focus in recent studies[15-17].It is thought that classic food intolerance is caused by food allergies based on IgE-mediated antibody responses; however, immediate allergic reactions are rare in IBD[18,19].Therefore, a delayed immune response mediated by IgG antibodies following exposure to a particular antigen may account for adverse food reactions in IBD[20].However, this mechanism is debatable, as some studies found that food IgG antibodies can be expressed in healthy individuals[21-26].The purpose of this study was to analyze the levels of IgG and IgE antibodies against food antigens in IBD patients and determine their clinical value in IBD pathogenesis.
MATERIALS AND METHODS
Subjects
We performed a retrospective study using blood samples obtained from patients who visited the First Affiliated Hospital of Nanjing Medical University between August 2016 and January 2018.According to the consensus on the diagnosis of IBD drawn up by European Crohn’s and Colitis Organization[27,28], each patient met the diagnostic criteria for CD or UC.We excluded patients who had been diagnosed with ischemic bowel disease, radiation enteritis, cardio-cerebral vascular diseases, infectious diseases, cancer or received surgery within 3 months.Healthy controls (HCs) were chosen from our Physical Examination Center to represent the general population.Finally, a total of 137 IBD patients, including 40 patients with UC and 97 patients with CD, and 50 HCs were enrolled in this study.Written informed consent was obtained from all patients.The Ethics Committee of the First Affiliated Hospital of Nanjing Medical University approved the study and the consent procedure.
Serum IgG/IgE assay
Serum IgG antibodies to 14 unique food antigens (chicken, beef, codfish, egg, crab,shrimp, milk, pork, rice, corn, mushroom, wheat, soybean and tomato) were assessed using enzyme-linked immunosorbent assay according to the manufacturer’s protocol(Biomerica Inc., Irvine, CA, United States).The IgG concentration was classified into the following four grades:negative (Grade 0, less than 50 U/mL), mild sensitivity(Grade +1, 50-100 U/mL), moderate sensitivity (Grade +2, 100-200 U/mL) and high sensitivity (Grade +3, > 200 U/mL).IgE-specific antibodies to food allergens (chicken egg white, cow’s milk, peanut, beef, mutton, shrimp, crab, marine fish including gadus, lobster, scallop, and freshwater fish including trout, weever, carp) were examined by western blotting according to the manufacturer’s instructions(EUROIMMUN Medizinische Labordiagnostika AG, Germany).An IgE concentration less than 0.35 kU/L was considered negative.Levels of 0.35-3.5 kU/L, 3.5-17.5 kU/L and > 17.5 kU/L were classified as mild specific antibody concentration, moderate specific antibody concentration with obvious clinical symptoms, and high specific antibody concentration, respectively.
Statistical analysis
The data were analyzed using SPSS software (version 21.0).Enumeration data were analyzed by the Chi-squared test.Continuous numerical variables were expressed as the mean ± SD.Comparisons between groups were performed using the Student’sttest or ANOVA test, as appropriate.Correlations among variables were analyzed by binary logistic regression.P< 0.05 was considered statistically significant.
RESULTS
Demographic and clinical characteristics of the patients
The demographic and clinical characteristics of the 50 HCs, 40 UC patients and 97 CD patients are summarized in Table 1.The average age in the UC, CD and HC groups was similar, the mean disease course in the UC and CD group was similar.The percentage of rectum, left-sided and entire colon type in UC patients was 25%, 17.5%,and 57.5%, respectively; 76.29% of CD patients had ileal or ileal-colon lesions, and 30.93% of CD patients had undergone IBD-related surgery.In total, 61.86% of CD patients and 75% of UC patients were in the active stage.In addition, 61.86% of CD patients and 30% of UC patients received treatment with steroids, immunosuppressive agents, or anti-TNFα; and 18.56% of CD patients received enteral nutrition.
Proportion of serum food-specific IgG in UC and CD patients
The positive rate of food-specific IgG in UC patients, CD patients and HCs was 57.5%,90.72% and 42%, respectively.CD patients showed higher positive rate of foodspecific IgG than HCs (P= 0.000).However, there was no significant difference between UC patients and HCs (P= 0.144) (Figure 1A).The number of IgG-positive food items was higher in UC and CD patients than in HCs (UCvsHCs,P= 0.029; CDvsHCs,P= 0.000; CDvsUC,P= 0.006) (Figure 1B).CD patients showed positive IgG against an average of 3.8 foods [range 1-8; 95% confidence interval (CI):3.41-4.20],while UC patients and HCs showed positive IgG against an average of 2.56 foods(range 1-8; 95%CI:1.73-3.39) and 1.57 foods (range 1-3; 95%CI 1.26–1.87), respectively.The average levels of total serum IgG in CD patients, UC patients and HCs were 138.6± 75.65, 115.6 ± 80.11, and 105.9 ± 52.3 U/mL, respectively.The average levels of total serum IgG in CD patients were significantly different from those in UC patients and HCs (CDvsUC,P= 0.03; CDvsHCs,P= 0.017), while there was no significant difference between UC patients and HCs (P= 0.554) (Figure 1C).The seropositive rate of moderate and high sensitivity was 39.13% in UC patients, 84.09% in CD patients and 71.43% in HCs, and the CD group had higher sensitivity to specific food allergens than the UC group (P= 0.000).
Distribution spectrum of food-specific IgG to 14 unique food allergens in UC and CD patients
In CD patients, the top nine food allergens causing positive serum IgG were tomato(80.68%), corn (69.32%), egg (63.64%) rice (61.36%), soybean (46.59%), milk (19.32%),wheat (17.65%), codfish (13.64%), and mushroom (3.4%).In UC patients, the nine main food allergens causing positive serum IgG were egg (60.87%), corn (47.83%),tomato (47.83%), rice (26.09%), soybean (21.74%), milk (21.34%), codfish (17.39%),wheat (8.7%) and mushroom (4.35%).The food-specific IgG detected in HCs was due to egg (66.7%), milk (28.6%), corn (19%), soybean (14.3%), mushroom (14.3%), rice(4.8%), and tomato (4.8%) (Figure 2), similar to the findings in a previous report[29].In the present study, CD patients were more sensitive to tomato, corn, rice, soybean,wheat and codfish, while UC patients were more sensitive to tomato, corn and rice(Table 2).CD patients had significantly higher levels of food-specific IgG than UC patients and HCs against rice (CDvsHCs,P= 0.000; CDvsUC,P= 0.01), soybean(CDvsHCs,P= 0.001; CDvsUC,P= 0.015), corn (CDvsHCs,P= 0.000; CDvsUC,P= 0.013), wheat (CDvsHCs,P= 0.012; CDvsUC,P= 0.016), tomato (CDvsHCs,P=0.001; CDvsUC,P= 0.201), and egg (CDvsHCs,P= 0.054; CDvsUC,P= 0.021).No significant differences were observed for beef (P= 0.148), chicken (P= 0.429), crab (P=0.385), shrimp (P= 0.164), codfish (P= 0.812), pork (P= 0.496), milk (P= 0.452) or mushroom (P= 0.122) specific IgG compared with HCs.No significant differences in food-specific IgG to 14 dietary antigens were observed between UC patients and HCs(Figure 3).
Relationship between food-specific IgG and disease location
The disease location of CD and UC patients was divided into subgroups according to the Montreal classification.The positive rates of food-specific IgG among subgroups of UC or CD patients were not significantly different.
Association between food-specific IgG and disease activity
The Crohn’s Disease Activity Index (CDAI) was used to evaluate CD patients’ disease activity, and the Mayo score was used to assess UC patients’ disease activity.Both CD and UC patients were divided into positive and negative food-specific IgG subgroups,with no marked statistical difference (CDAI:Food-specific IgG+vsfood-specific IgG-,P= 0.27; Mayo:food-specific IgG+vsfood-specific IgG-,P= 0.58).It was found that the group with more than three positive allergens had a higher CDAI score compared with the group with two positive allergens (P= 0.033).The Mayo score in the group with multiple positive allergens was higher than that in the group with a single positive allergen (2 positivevs1 positive,P= 0.024; ≥ 3 positivevs1 positive,P=0.046).We also divided CD and UC patients into three subgroups according to the degree of seropositivity.There were no significant differences among the threesubgroups (Figure 4).
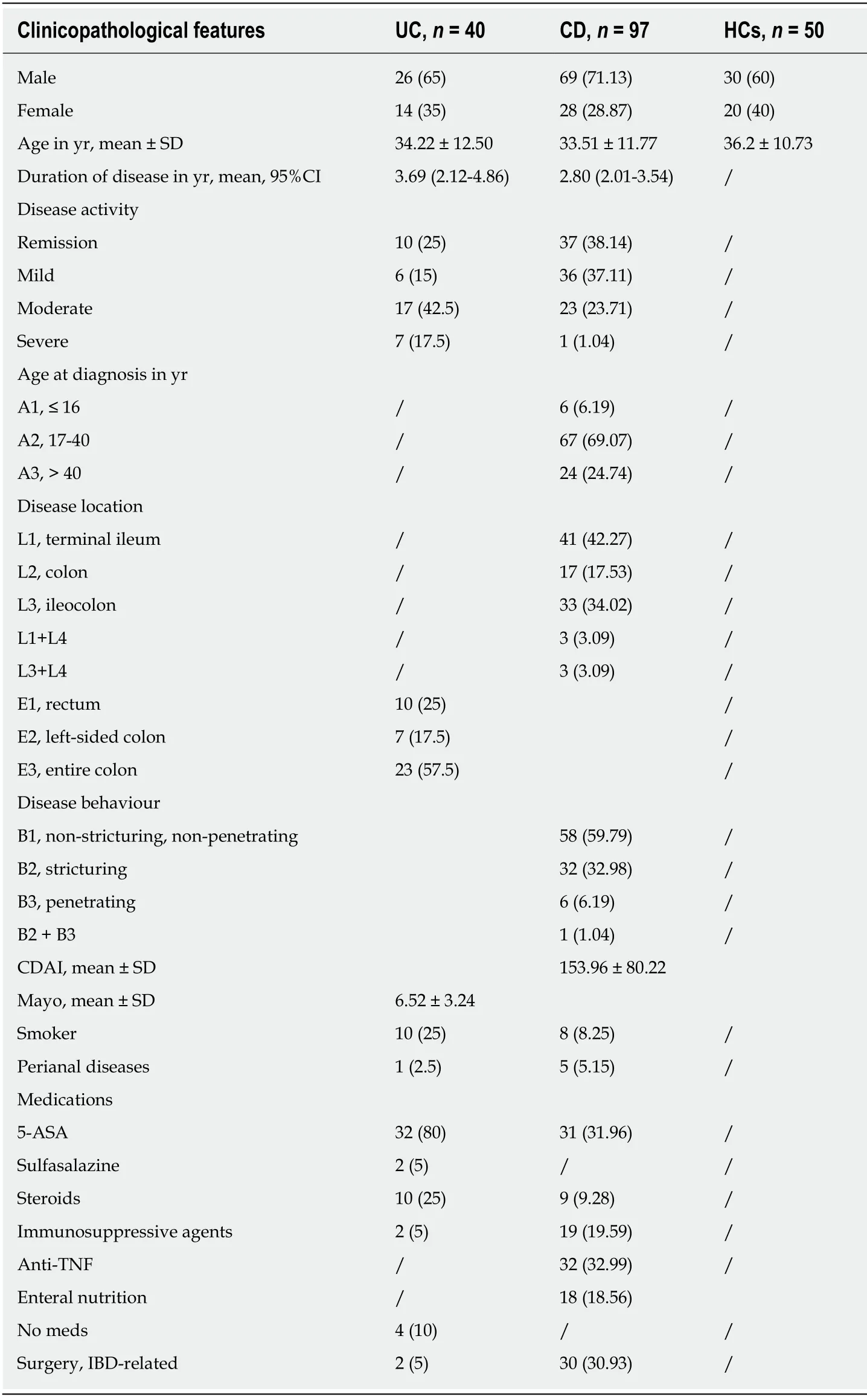
Table 1 Clinical characteristics of all subjects, n (%)
Relationship between food-specific IgG and clinical characteristics
The food-specific IgG-positive group had higher levels of inflammatory biomarkers,such as leukocyte count, platelet count, erythrocyte sedimentation rate (ESR) and Creactive protein (CRP) compared with the food-specific IgG-negative group, although there was no significant difference between the groups (Table 3).
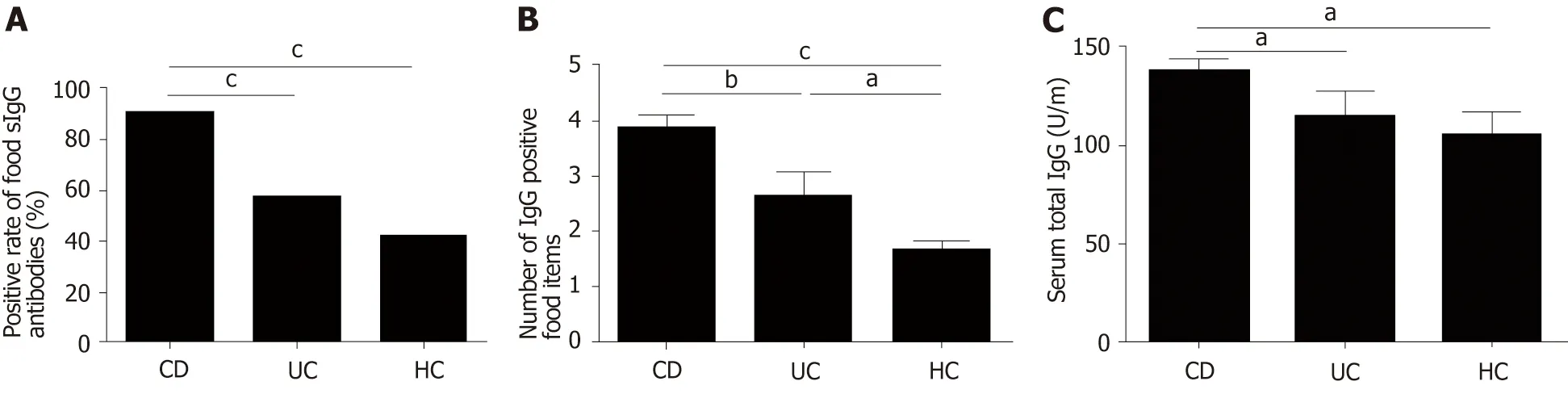
Figure 1 High sensitivity to food antigens in inflammatory bowel disease patients.
The association between demographic and other factors with food-specific IgG is shown in Table 4.Subjects who smoked were prone to developing serum food-related IgG antibodies [OR (95%CI):17.6 (1.91-162.26);P= 0.011].CD patients were more predisposed to food intolerance than UC patients [OR (95%CI):12.48 (3.45-45.09);P=0.000] (Table 4).
Anti-TNFα was an effective biological agent in IBD patients.Higher total food IgG levels were found in patients treated with anti-TNFα compared to patients treated with steroids or immunosuppressants (anti-TNFαvssteroids,P= 0.013; anti-TNFαvsimmunosuppressants,P= 0.000) (Figure 5A).However, we found a decrease in foodspecific IgG levels in IBD patients after introducing anti-TNFα (before anti-TNFαvsafter anti-TNFα,P= 0.009) (Figure 5B).
Prevalence of serum specific IgE to antigens
It was shown that 65.2% of CD patients, 57.1% of UC patients and 60% of HCs had specific IgE antibodies; and 62.5%, 12.5%, and 25% of UC patients and 26.67%, 30%,and 43.33% of CD patients were sensitive to one, two, or three or more allergens,respectively.These values were 25%, 33.33%, and 41.67% in HCs.The seropositive rate of moderate and high sensitivity was 50% in UC patients, 56.67% in CD patients and 71.43% in HCs.The differences among the three groups in the occurrence of IgE positivity were not statistically significant (P= 0.831).The average levels of total serum IgE in subjects with CD, UC and HCs were 3.68 ± 6.62, 0.61 ± 0.17, and 0.90 ±0.68 kU/L, respectively.There was no significant difference among CD patients, UC patients and HCs (CDvsHCs,P= 0.202; UCvsHCs,P= 0.933; CDvsUC,P= 0.316)(Figure 6).
Proportion of serum food-specific IgE antibodies
In this study, 16.67% of HCs had food-specific IgE against marine fish in contrast to 46.67% of CD patients and 25% of UC patients.In addition, 20% of CD patients had IgE to beef in contrast to only 8.33% of HCs.This was even more pronounced in terms of IgE antibodies to egg white, with 6.67% of CD patients and 12.5% of UC patients showing IgE antibodies, while HCs showed no egg white IgE antibodies (Figure 7).
DISCUSSION
Immune tolerance to exogenous antigens, including commensal bacteria and food proteins is a pivotal regulation mechanism for maintaining intestinal homeostasis.A breakdown in immune tolerance to exogenous antigens is considered to play a role in the initiation and development of chronic inflammation in IBD[30].Some IBD patients have shown an improvement in symptoms following exclusion diets[31-33].Previous studies have investigated the potential role of serum IgG/IgE in food intolerance/allergy[34,35], and a thorough study of exclusion diet according to food IgG/IgE tests has been conducted[36,37].However, the reliability and clinical practicability of food-specific IgG/IgE detection remain controversial, although it is a potential method for the diagnosis of food intolerance/allergy.
In the present study, CD patients had high levels of serum food-specific IgG antibodies compared to UC patients and HCs.Most (90.72%) of the CD patients had higher levels of IgG antibodies, similar to previous findings[17].Both CD and UC patients also had more IgG-positive food items and higher sensitivity.Similar results were reported by Caiet al[17], who found that IBD patients were sensitive to multiple food antigens.Food allergy was once thought to play a part in the progression ofIBD[38].However, food-specific IgE was not found in CD patients in the studies by Huberet al[39]and Bartůnkováet al[40].In the present study, 57.1% of UC patients, 65.2%of CD patients, and 60% of HCs had detectable specific IgE to different food antigens,but these values were not statistically significant.
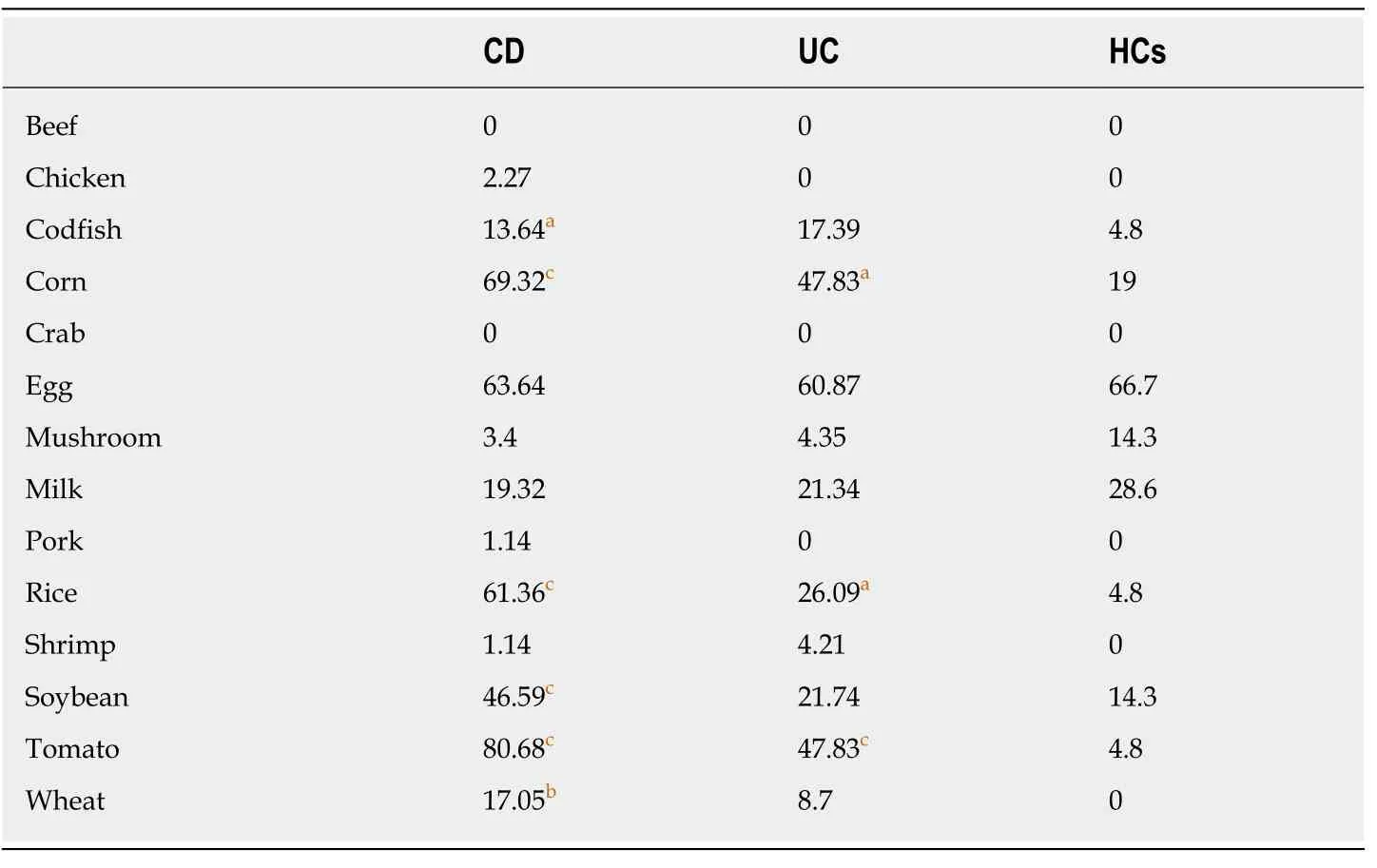
Table 2 Percentage of positive food-specific lgG antibodies against 14 food items in ulcerative colitis patients, Crohn’s disease patients, and healthy controls
A study showed that the common food allergens that caused positive IgG in CD patients were egg (73.3%), rice (56.7%), corn (56.7%), tomato (46.7%) and soybean(43.3%).In addition, the frequent food allergens in UC patients were egg (81.0%), rice(14.3%), corn (14.3%), tomato (9.5%) and milk (9.5%).The corresponding food allergens in HCs were egg (69.3%), milk (14.8%), and crab (14.8%)[17].In the present study, the most common food-specific IgG antibodies detected in CD patients were against tomato in 80.68% of patients, followed by corn in 69.32%, egg in 63.64%, rice in 61.36%, soybean in 46.59%, milk in 19.32%, wheat in 17.65%, and codfish in 13.64%of patients.The most common food-specific IgG antibodies detected in UC patients were egg (60.87%), corn (47.83%), tomato (47.83%), rice (26.09%), soybean (21.74%),milk (21.34%), codfish (17.39%), and wheat (8.7%).The most common food-specific IgG antibodies detected in HCs were egg (66.7%), milk (28.6%), and corn (19%).Collectively, these data suggest that both IBD patients and HCs showed a high level of egg-specific IgG antibodies, while IBD patients may be prone to rice, corn, tomato and soybean intolerance.Foods such as rice, wheat, corn, soybean, and tomato are traditional products and some of the most commonly used ingredients in China.As such, most Chinese people are frequently exposed to these intestinal antigens.No marked changes were observed in beef, shrimp, crab, chicken, pork, or mushroom specific IgG between CD patients and HCs.This may be because CD patients subconsciously avoid triggering foods (e.g., beef, shrimp, crab, chicken, pork, and mushroom) to alleviate the antibody response.
Food-specific IgG antibodies are often discovered in IBD patients whose small intestine is affected, which might be related to lactose malabsorption[17,41].A survey showed that IgG-positive IBD patients had higher mean levels of ESR and high sensitivity-CRP and had severe disease activity[26].In our study, there was no significant difference in the CDAI and Mayo score between the positive and negative IgG antibody subgroups.The multiple positive allergens group had a higher CDAI/Mayo score compared with the single positive allergen group.In addition, the food-specific IgG-positive group had higher levels of inflammatory biomarkers, such as ESR and CRP, leukocyte count, and platelet count compared to the food-specific IgG-negative group, although no significant differences were observed.
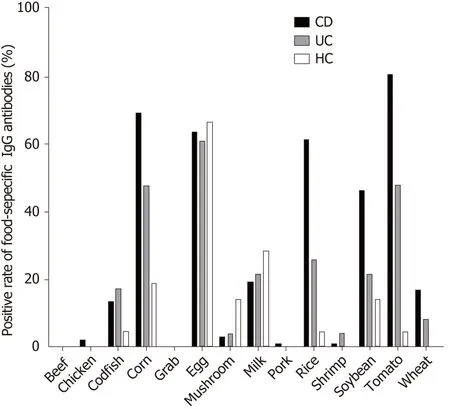
Figure 2 Distribution of positive lgG to food allergens in CD patients, UC patients and HCs.
In some studies, it was reported that food intolerance was more common in females than in males[42-45].In this study, females were 2.07-fold more likely than males to develop food intolerance, but this difference was not statistically significant.Some studies have demonstrated that female hormones exert a pro-inflammatory effect,while testosterone inhibits the pro-inflammatory process, such as histamine release and mast cell degranulation[46].Some investigations have reported that the elderly population may be more likely to develop food allergies than younger individuals[47].However, other studies have revealed that the younger age group had higher levels of food-specific IgG compared with older people[45,48], which is similar to the results in the present study.Maturation of intestinal mucosa with increasing age may influence food intolerance resulting in differential immune responses at different ages.This study also demonstrated that CD patients were more predisposed to food intolerance than UC patients.Smoking was found to be a risk factor for food intolerance in IBD patients.The etiology and pathogenesis of smoking in IBD is not yet entirely clear due to the complex chemical composition of tobacco.Potential mechanisms worth considering include gene expression changes relevant to immune responses and the citrullination of various proteins, which then influence the three-dimensional structure of proteins in such a way that the altered proteins subsequently act as antigens[49].
Anti-TNFα, a biological agent, has been confirmed to be effective in the treatment of IBD patients.Our study showed higher levels of total food-specific IgG in IBD patients receiving anti-TNFα therapy compared to patients receiving treatment with steroids or immunosuppressants.A decrease in total food-specific IgG levels in IBD patients was observed after the introduction of anti-TNFα therapy.Anti-TNFα treatment can result in long-term remission and mucosal healing.Intestinal barrier repair and prolonged inflammation suppression may improve intestinal barrier dysfunction, which prevents food antigens from entering the circulation leading to the production of food-specific IgG[45].
The present study has several limitations.Firstly, we only tested common foodspecific IgG antibodies and did not measure food-specific IgG to nuts, fruits or food ingredients.Secondly, we did not conduct a follow-up study to determine whether excluding IgG-positive foods had an effect on IBD patients.Thirdly, children were not included in our study.Finally, our sample size was small; therefore, larger cohort studies should be conducted to confirm our results and to reveal the possible underlying mechanism.
In conclusion, the level of food-specific IgG is higher in CD patients than in UC patients and HCs.IBD patients may be prone to rice, corn, tomato and soybean intolerance.Although the mechanism of food intolerance in IBD is still unclear, we believe that food-specific IgG antibodies may provide a clinical benefit for IBD patientsviadiet restriction.The role of food-specific IgG in food intolerance should be investigated in future studies.
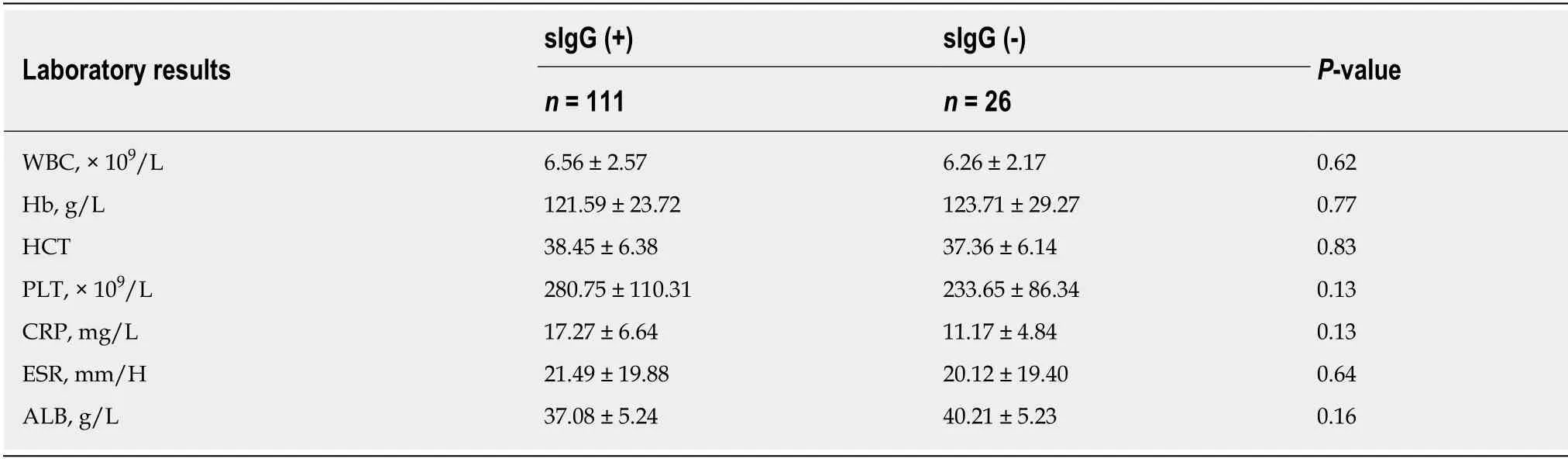
Table 3 Comparison of laboratory results between positive and negative food-specific lgG subgroups in inflammatory bowel disease patients
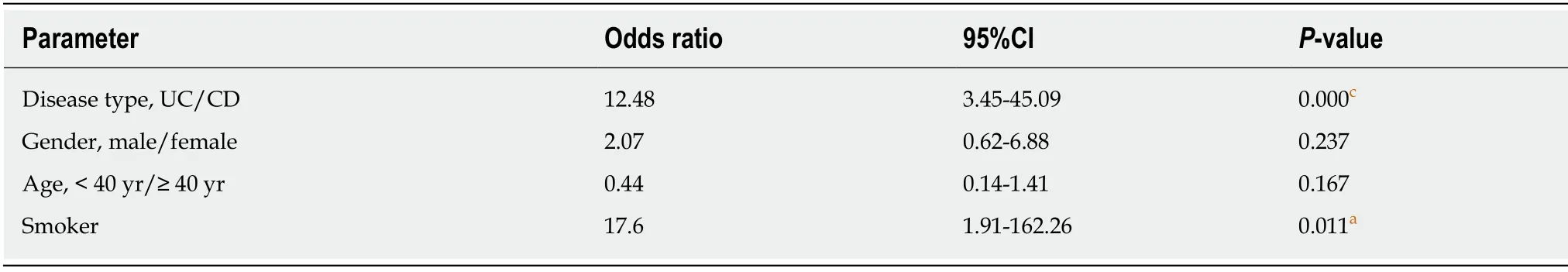
Table 4 Correlation between food-specific lgG and clinical parameters
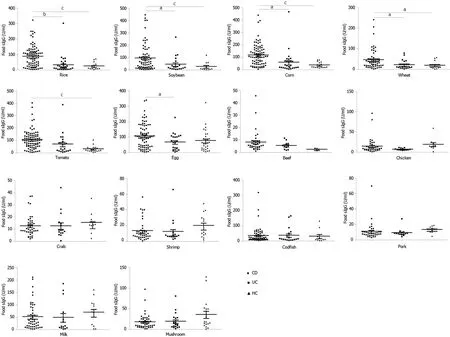
Figure 3 The levels of food-specific lgG against 14 common daily foods in CD patients, UC patients and HCs.
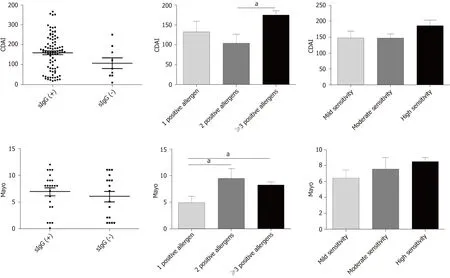
Figure 4 Association between food-specific lgG antibodies and disease activity.
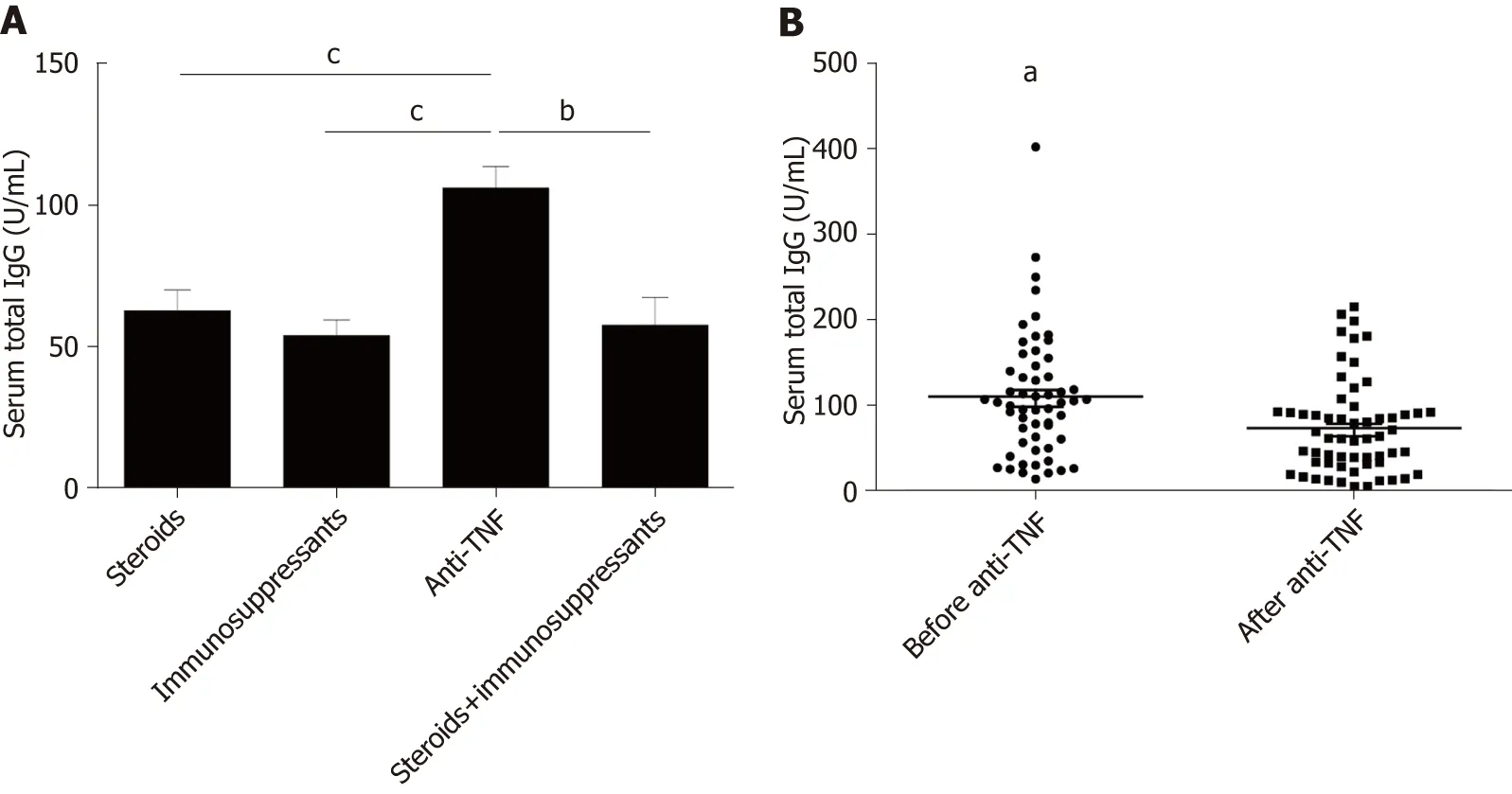
Figure 5 Serum food-specific lgG concentrations in patients treated with different medications and comparison of food-specific lgGs for inflammatory bowel disease patients before and after lnfliximab treatment.
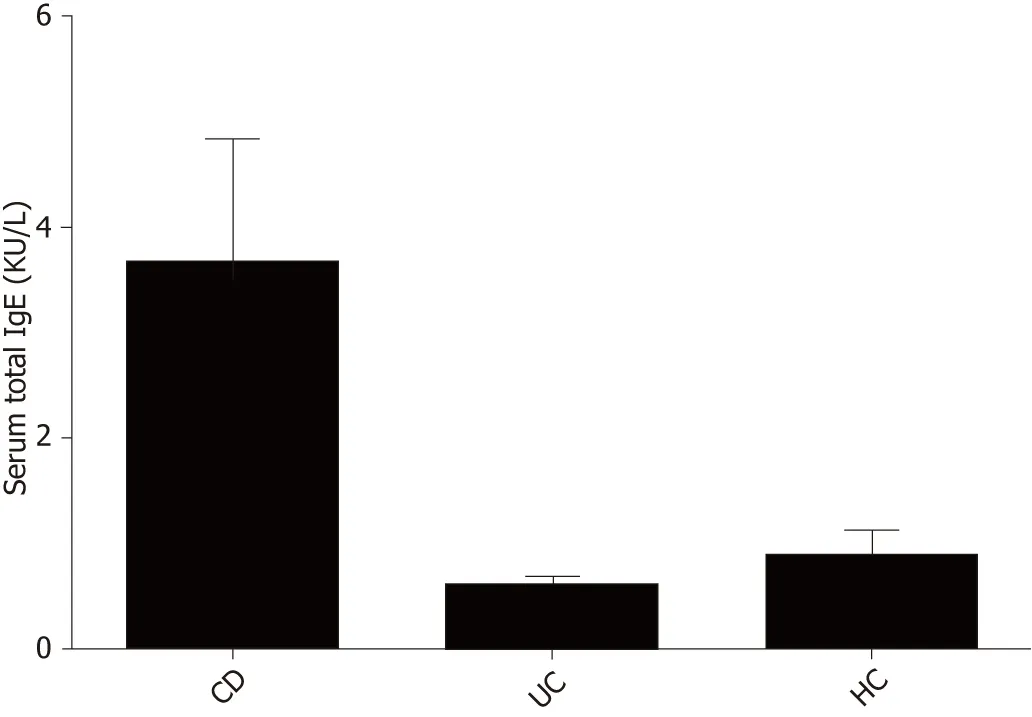
Figure 6 Comparison of total serum lgE levels between CD patients, UC patients and HCs.
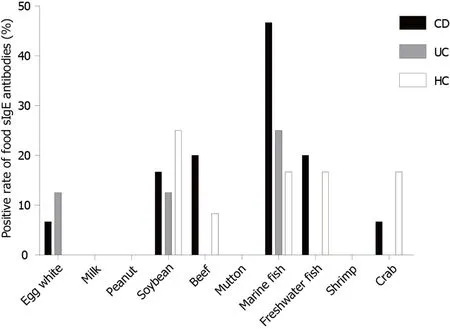
Figure 7 Distribution of positive lgE to food allergens in CD patients, UC patients and HCs.
ARTICLE HIGHLIGHTS
Some food antigens have been considered to be involved in the processes of formation and development of human chronic intestinal inflammatory diseases.Food allergy and food intolerance are two types of adverse reactions to food.Food allergy is typically mediated by IgE antibodies.In contrast, food intolerance is mediated by IgG antibodies.However, this mechanism is disputable, as some studies found that food IgG and IgE antibodies can be expressed in healthy individuals.The purpose of this study was to analyze the levels of immunoglobulin G (IgG) and E (IgE) antibodies against food antigens in inflammatory bowel disease (IBD) patients and explore their clinical value in IBD pathogenesis.
Research background
IBD is a chronic relapsing inflammatory disease of the gastrointestinal tract, which includes ulcerative colitis (UC) and Crohn’s disease (CD).Increasing evidence indicates that IBD results from an abnormal mucosal immune system triggered by environmental factors.Of these factors,food antigens have been considered to involve in the processes of formation and development of IBD.Food allergy and food intolerance are two types of adverse reaction to food.Food allergy is typically mediated by IgE antibodies.In contrast, food intolerance is mediated by IgG antibodies.However, this mechanism is disputable, as some studies found that food IgG and IgE antibodies can be expressed in healthy individuals.
Research motivation
Food antigens have been suggested to participate in the etiopathogenesis of IBD.The advantages from removing certain foods from daily diet was focused on in recent studies.A number of IBD patients suffer from food intolerances, and they show an improvement of well-being by avoiding specific nutritive components.Previous studies have either researched on the potential involvement of various IgG/IgE subclasses in food intolerance/allergy.Although testing for the presence of food-specific IgG/IgEs has been regarded as a potential tool for the diagnosis of food intolerance/allergy, the accuracy and clinical utility of such testing remain unknown.
Research objectives
The purpose of this study was to analyze the levels of IgG and IgE antibodies against food antigens in IBD patients and explore the clinical value in the pathogenesis of IBD.
Research methods
A total of 137 IBD patients, including 40 patients with UC and 97 patients with CD, and 50 healthy controls (HCs) were enrolled in this study.Blood samples were obtained from patients who visited the First Affiliated Hospital of Nanjing Medical University between August 2016 and January 2018.Serum IgG antibodies to 14 unique food antigens were assessed using enzyme-linked immunosorbent assay.IgE-specific antibodies to food allergens were examined by Western blot.
Research results
CD patients had a higher prevalence of food-specific IgG compared to UC patients.CD patients were more sensitive to tomato, corn, rice, soybean, wheat and codfish, while UC patients were more sensitive to tomato, corn and rice.Significantly higher levels of total food-specific IgG were detected in IBD patients treated with anti-TNFα therapy compared to patients receiving steroids or immunosuppressants.A decrease in food-specific IgG levels was detected in IBD patients after receiving anti-TNFα therapy.Smokers and CD patients were prone to developing serum food-specific IgG antibodies.
Research conclusions
The prevalence of food-specific IgG is higher in CD patients than in UC patients and HCs.IBD patients may be prone to rice, corn, tomato and soybean intolerance.
Research perspectives
Food-specific IgG antibodies may provide a clinical benefit for IBD patientsviadiet restriction.In the future, the role of food-specific IgG in food intolerance should be further investigated.
ACKNOWLEDGEMENTS
An abstract of this study was invited as an E-poster in APDW 2018 and was published as an abstract only in the Journal of Digestive Disease, 2018.
杂志排行
World Journal of Clinical Cases的其它文章
- Role of infrapatellar fat pad in pathological process of knee osteoarthritis:Future applications in treatment
- Application of Newcastle disease virus in the treatment of colorectal cancer
- Reduced microRNA-451 expression in eutopic endometrium contributes to the pathogenesis of endometriosis
- Application of self-care based on full-course individualized health education in patients with chronic heart failure and its influencing factors
- Predicting surgical site infections using a novel nomogram in patients with hepatocelluar carcinoma undergoing hepatectomy
- lncidence of infectious complications is associated with a high mortality in patients with hepatitis B virus-related acute-on-chronic liver failure
