Effects ofmidwife-led psychologicalintervention on delivery outcomes:a meta-analysis
2018-09-14YuanJiaSiYuanYangLiMingGuoQianWuFanJieMeng
Yuan Jia,Si-Yuan Yang,Li-Ming Guo,Qian Wu,Fan-Jie Meng,*
1Tianjin University of Traditional Chinese Medicine,Tianjin,China.
Introduction
At 28 weeks or more of pregnancy,the process of fetuses and attachments being delivered from the mother is referred to asdelivery.Delivery is a continuous physiological process that lasts for a long time and goes hand-in-hand with severe pain.Maternal mental and psychological conditions significantly influence the entire delivery process as well as pregnancy outcomes.The meaning of psychological intervention is that medical personnel-guided by the theory of psychological science,based on good interpersonal relationships,and through interaction with patients-affectthe patient's acute psychological state and behavior.
Studies have shown that psychological intervention plays a critical role in the maternal psychological state[1-2].Therefore,a useful psychological intervention on a parturient can help the mother to gain confidence during delivery,which facilitates a smooth transition from the puerperalperiod.Midwives are low-risk maternal professional caregivers[3].Their roles include midwifery and delivery of newborns,providing care for newborns,and comprehensive continuity services for pregnant women and mothers[4].Midwives are required to protect the health of the puerpera and children in all aspects of physical,psychological,social,and cultural needs,and they also take care of women's reproductive needs during pregnancy,childbirth,and puerperium.Psychological intervention provided by midwives is more specific to the entire maternal delivery process.Foreign literature shows that psychological interventions led by midwives have positive effects on maternal psychological status(anxiety,depression,fear)and childbirth self-efficacy(confidence in delivery)[5-6].
The present study has a strict inclusion and exclusion criteria for the literature,studies on midwife-led psychological interventions and the indicators of natural delivery rate,delivery time,postpartum hemorrhage after delivery for two hours,etc.were systematically evaluated.The impact of psychological interventions on maternal outcomes provides more reliable evidence for clinical practice as well as guidance for midwifery practice.
Methods
Search strategy and study selection
Papers published up to March 2018 were searched in databases including Cochrane Library, PubMed,Medicine,EMBASE,CINAHL,CNKI,Wanfang,and VIP database,and unpublished literaturewasalso included.Based on the content of the search,details on the research subjects,intervention,control,research design were extracted;keywords were extracted for the pre-search,mesh words were determined,and free words were combined.The English search terms were“midwife and psychological intervention”, “nursing” or“psychological care”; “maternal”, “pregnant women”,“pregnancy”or “puerpera”; “anxiety”, “depression”or“fear”and “RCT”.The Chinese search terms were “助产士”,“心理护理”or“心理干预”;“第一产程”or“产程”;“自然分娩”,“剖宫产”or“分娩方式”;“产后出血”;“产妇”,“孕产妇”or“孕妇”and “对照”or“对比”.
Inclusion criteria
(1)Intervention target:pregnant woman and puerpera.(2)Interventions:Psychological interventions and routine care that was provided by the midwives to the trial group.The primary measures included midwives talking about the delivery process to first-time mothers prior to delivery,focusing on the cooperation of puerpera during the delivery period,emphasizing the clinical advantages of natural delivery methods,safeguarding their basic needs,being satisfied in improving theirnaturaldelivery confidence,providing instructions on maternal body position during the delivery period,assisting them to breathe and relax,enhancing language comfort,and maintaining an active childbirth state.During the active period of pain,midwives should enhance the management of maternal,help their appropriate relaxation in the contraction clearance and moderate ingest high-calorie foods to ensure that they are energetic and regularly report their basic conditions to their doctor.After the successful delivery of the fetus,the patient is given a reasonableappraisalin atimely manner,and the development condition of the newborn is communicated to ensure maternal self-improvement.After the delivery,based on the status of maternal recovery, the breastfeeding method is described in a timely manner to increase the awareness of breastfeeding.The control group was provided with routine care,which involved bringing mothers with uterine contractions to the delivery room.This was done by the nursing staff and the midwife who was on duty,without psychological intervention.(3)Type of study:Randomized controlled trials(RCTs).(4)Literature quality:in order to ensure the accuracy of the meta-analysis results,Chinese literature was also included in the use of a random number table method or red and blue ball grouping method.
Exclusion criteria
Studies that met one of the following conditions were excluded:(1)random assignment method was unknown;(2) an intervention other than a psychological intervention was used for the experimental group;(3)not a midwife-provided intervention;(4)original text was not available through various channels;(5)abstract provided insufficientinformation;(6)statisticalmethod was incorrect;(7)duplicate articles;(8)review.
Outcome indicators
These included:(1)the number of people who opted for natural delivery;(2)the time required for the first stage of delivery(i.e.,the time from the intermittent regular contractions for 5-6 minutes to the full opening of the cervix);(3)the amount of postpartum hemorrhage after delivery for two hours.
Filing and data extraction of the literature
(1)NoteExpress was used to exclude duplicate articles.(2)Depending on the screening criteria,two researchers independently read the titles and the abstracts for the initial screening.(3)After reading the entire text,the two readers independently read the papers and to exclude studies thatdid notmeetthe inclusion criteria.Disagreements were resolved through discussion.If the discussion could not reach an agreement,a third party made a ruling.(4)The researchers carefully read the papers and independently extracted key information,which included information on the author(s),publication year,number of studies,and outcome measures.See Table 1 for details.
Assessment of risk of bias and grading the quality of evidence
The Cochrane Randomized Controlled Trial Bias Risk Tool was used to evaluate the quality of the included literature[7-8].This method mainly evaluates original studies from seven aspects,which includes random sequence generation,allocation concealment,blinding of researched subjects and researchers,blinding of outcome measure,incomplete outcome data,selective reporting,and other biases.The two evaluators independently made judgments on each aspect of the included studies with high risk of bias,low-risk of bias,or unclear bias.If there were any inconsistencies,it was discussed and resolved by the third evaluator.If a study fully satisfied the above aspects,it was rated as A grade;if it partially satisfied,it was rated as B grade;if it did not satisfy these aspects,it was rated as C grade.

Table 1 Characteristics of the included RCTs
Data analysis
We used a 95%confidence interval(CI)to assess the relative risk of the dichotomous outcomes and 95%CI weighted mean difference of the consecutive outcomes.Random effects models were used regardless of heterogeneity.The heterogeneity report uses I2statistics,and I2>50%indicates significant heterogeneity[9].As long as there is a significant heterogeneity,we will look for potential sources of heterogeneity.For example,if a study showed that the results are completely different from other results,we examined the possible reasons for explaining the differencesand did notperform a sensitivity analysis of the study.P>0.1 and I2<50%indicate homogeneity among the studies,and a meta-analysis was performed using a fixed-effect model.When the number of included studies is more than 10,a funnel plot needs to be drawn to analyze whether the presenceofpublication bias[10].Funneldiagram asymmetry proves a possible publication bias.When it was impossible to judge the sources of the study’s heterogeneity and merger analysis,the meta-analysis was not performed,and only one description was made.
Study selection and characteristics
A detailed flowchart of the search and selection results is given in Figure 1.The search yielded 369 potentially relevant articles.Finally,12 RCTs that met our inclusion criteria were included in the meta-analysis[11-22].The main characteristics of the 12 RCTs are shown in Table 1.These studies were published between 2015 and 2018.Of the 12 studies,two were conducted in Australia[11-12]and ten in China[13-22].The sample size of the RCTs ranged from 25 to 134(a total of 1395).In all studies,midwives were reported to have extensive experience in psychological care.Among the 12 studies,all reported the increase in the number of people who opted for natural delivery,five reported on the decrease the duration of the first stage of delivery,five reported on the decrease in the amount of postpartum hemorrhage after delivery for two hours.

Figure 1 Flowchart of the selection process of the meta-analysis
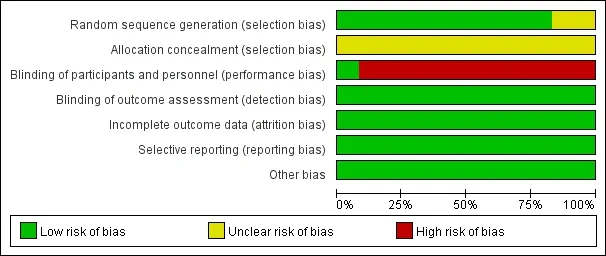
Figure 2 Risk of bias graph of included studies

Figure 3 Risk of bias summary
Risk of bias and grades of evidence
Details on the assessment of the risk of bias were shown in Figure 2-3.Based on Cochrane Handbook 5.1.0 criteria for the evaluation of the quality of the literature,of the 12 RCTs,nine were grouped by a random number table method,one study used red and blue ball grouping method,and the method used in two articles in English is unknown.One of the articles employed a double-blinded method,while the remaining studies did not use a double-blinded method.Therefore,11 studies were rated as high risk.All 12 studies were rated as low-risk and not loss of visit;12 studies were completed and rated as low-risk.The studies were rated as low-risk for other biases.All 12 studies were rated as grade B based on the results of the quality assessment.
Results
The number of people opting for natural delivery
Twelve studies reported the choice of the delivery mode;no significant heterogeneity was found between studies(P=0.05,I2=45%),by using the fixed effects model line meta-analysis,the results showed that mental nursing by midwives can improve the number of people opting for naturaldelivery;themerge effectwasstatistically significant[Z=7.53,95%CI(2.07,3.45),P<0.001](Figure 4).According to the funnel diagram shown in Figure 5,most of the studies were within the 95%CI cutoff.However,three studies were outside the 95%CI cutoff,indicating that the effect of the midwife-led psychological intervention on the number of people opting for natural delivery may be biased,and more RCTs are needed to confirm this result.
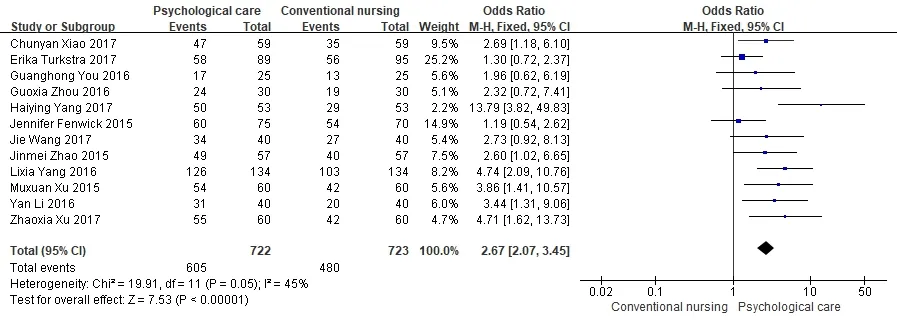
Figure 4 Influence on the number of people choosing natural delivery
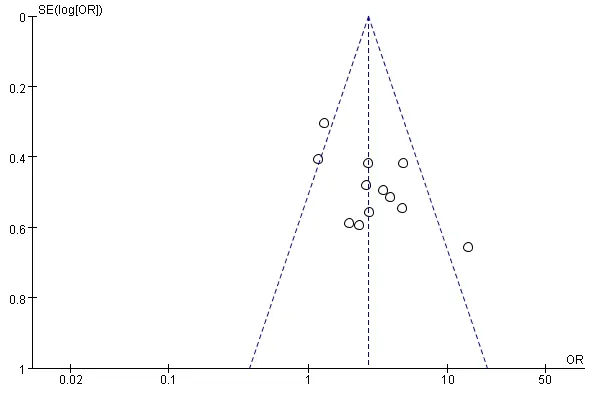
Figure 5 Funnel plot of people choosing natural delivery

Figure 6 Influence on the duration of the first stage of delivery
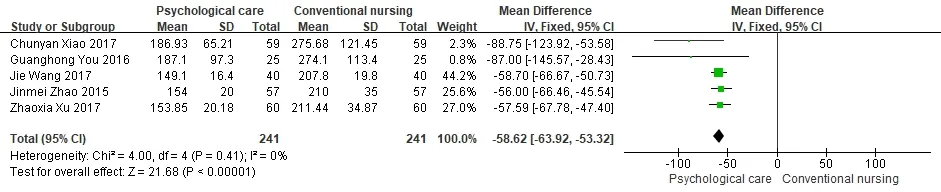
Figure 7 Influence on the postpartum hemorrhage after delivery for two hours
The duration of the first stage of delivery
Five studies[14,15,16,17,21]reported on midwives providing psychological care for mothers for the first time,the duration of the first stage of delivery between different researches has no statistical heterogeneity(P=0.24,I2=27%).Based on the results of the fixed effects model line meta-analysis,psychological nursing provided by midwives can shorten the duration of the first delivery;the merge effect was statistically significant[Z=45.10,95%CI(-4.43,-4.06),P<0.001](Figure 6).
Postpartum hemorrhage after delivery for two hours
Five studies[14,15,19,20,22]reported on the effect of psychological nursing provided by midwives on postpartum hemorrhage after delivery for two hours;there was no significant heterogeneity between the five studies(P=0.41,I2=0).Based on the results of the fixed effects model line meta-analysis,psychological nursing provided by midwives can reduce postpartum hemorrhage after delivery for two hours;the merge effect was statistically significant[Z=21.68,95%CI(-63.92,-53.32),P<0.001](Figure 7).
Discussion
At present,in addition to psychological interventions,commonly used midwife-led, non-pharmacological treatment measures include midwifery outpatient clinics,midwife accompanying,and applying delivery balls[28-30].Research shows that various interventions have a positive effect on maternal outcomes.However,as midwifery outpatient services are highly demanding for midwives and require large amounts of funds,it is difficult to popularize them.The midwife's full-time attendance requires a large amount of manpower for the midwife,and the safety of the delivery ball has not yet been proven.In the process of maternal childbirth,due to fear and other psychological factors,care and support of the midwife are the mostneeded.Psychological interventions require the midwife to use professional knowledge and language and other nonverbal behaviors to provide help and support to the mother.It is easy to implement and very effective.Therefore,it is easy to expand.
Influence on the number of people opting for natural delivery
According to the results of the meta-analysis,midwife-led psychologicalintervention increasesthe numberof people who opt for natural delivery.The international midwifery professionalservice conceptconsistsof advocating for natural delivery and “midwife-led mode”[23-25].The reason for the results obtained in the meta-analysis may be that midwives are the primary service providers for pregnant women.They establish a good relationship with pregnant women through psychologicalinterventions,thereby promoting their confidence in delivery.The midwife gives targeted answers and psychological counseling based on a full understanding of the specific conditions of pregnant women and mothers,in order to improve the mental health of pregnant women and mothers,increase their awareness of childbirth,and help pregnant women choose a more appropriate mode of delivery.Midwives provide psychological interventions to impart knowledge about natural births and the advantages and disadvantages of the cesarean section before birth,inform the mothers of the precautions and main processes involved in childbirth,and promote the physical and mental preparations for childbirth.Maternal women are more likely to choose natural childbirth after receiving guidance on childbirth and receiving psychological support from the midwife.
Influence on the duration of the first stage of delivery
According to the results of the meta-analysis,midwife-led psychological intervention shortens the duration of the first stage of delivery.The reason for this finding might be that the first stage of delivery is the cervix dilatation phase,which is the period from the beginning of regular contractions to the full opening of the cervix.It takes about 11 to 12 hours for first-time mothers,6-8 hours for the experienced mothers,and regular contractions occur in the first stage of delivery.Severe pain not only causes severe physical pain to the mother,but also affects the parturition mood of the mother and causes anxiety,nervousness,fear,and other undesirable emotions,which thereby leads to an increased secretion of catecholamines and prolonged delivery. Through midwife-led psychological intervention during the delivery process,mothers can be observed by midwives and receive psychological interventions in real time.Midwives can help mothers adjust their emotions any time.At the same time,the uterine dilation and contraction are accompanied by pain.Throughout the process,the midwife can guide the mother on easing the pain,adjusting breathing,and using force to facilitate delivery.Midwives provide support and encouragement and use mental power to shorten the duration of the first stage of delivery.They also promote maternal childbirth[26].
Influence on postpartum hemorrhage after delivery for two hours
Studies have shown that maternal tension,anxiety,and other negative emotions lead to a release in a large number of catecholamines, increased angiotensin,increased peripheral arterial flow resistance,increased blood pressure, resulting in uterine contractions,increased bleeding,prolonged labor,dystocia,and other adverse consequences[27].According to the results of the meta-analysis,midwife-led psychological intervention reduces the amount of postpartum hemorrhage after delivery for two hours.This could be because,under the comprehensive psychological intervention provided by midwives,an increasing number of mothers recognize the benefits of natural delivery and opt for natural childbirth.Natural childbirth has been completed faster,the delivery process has been accelerated,and the placenta has been delivered smoothly. Moreover, the psychological intervention provided by midwives helps mothers to adjust their emotions,adjust their breathing,and receive supportand encouragement.Therefore,midwife-led psychological intervention is beneficial to reduce the amount of postpartum hemorrhage after delivery for two hours.
Limitations and prospects
In this study,only papers published in Chinese and English languages were included.Although we conducted extensive searches,the keywords and their combinations used for classification may affect our ability to search without errors.Despite the additional search,this study still has not yet been fully collected,the sample size was limited,there was selection bias,and the conclusion is limited;the quality of the 12 RCTs was moderate,and the funnel plot also showed that there might be publication bias in the included literature.Therefore,we expect more large-scale,high-quality clinical RCTs to be conducted;the effects of psychological interventions are subjective to midwifery and maternal factors.Moreover,subjectivity cannot be eliminated,which may lead to overestimation or underestimation of the actual application effect.The maternal and neonatal women may differ in their psychological status and adaptability,and therefore,there may exist bias.
Conclusion
This study shows thatmidwife-led psychological intervention can improve the number of people opting for the natural delivery,shorten the duration of the first stage of delivery,and reduce postpartum hemorrhage after delivery for two hours.The results of the meta-analysis show that the data combined results are more reliable,it is recommended to promote it for clinical use.
1. Evans K,Morrell CJ,Spiby H.Systematic review and meta-analysis of non-pharmacological interventions to reduce the symptoms of mild to moderate anxiety in pregnant women.J Adv Nurs 2018,74:289-309.
2. Yildiz PD,Ayers S,Phillips L.The prevalence of posttraumatic stress disorder in pregnancy and after birth:a systematic review and meta-analysis.J Affect Disord 2017,208:634-645.
3. Liu MF.Overview of the capabilities a midwife needs.Xinjiang Med J 2015,1:29-32.
4. Zhang JJ,Li F,Wang DM,et al.International definition of a midwife.Shandong Med J 2003,3:20.
5. Toohill J,Fenwick J,Gamble J,et al.A randomized controlled trial of a psycho-education intervention by midwives in reducing childbirth fear in pregnant women.Birth 2014,41:384-394.
6. Turk M,Aydogdu M,Gursel G.Effects of modes,obesity,and body position on non-invasive positive pressure ventilation success in the intensive care unit:a randomized controlled study.Turk Thorac J 2018,19:28-35.
7. Higgins JPT,Green S.Cochrane handbook for systematic reviews of interventions version 5.1.0.London:The Cochrane Collaboration,2011.
8. Cochrane handbook forsystematicreviewsof interventions.Chichester:Wiley-Blackwell,2008.
9. Begg CB,Mazumdar M.Operating characteristics of a rank correlation testfor publication bias.Biometrics 1994,50:1088-1101.
10.Egger M,Davey SG,Schneider M,et al.Bias in meta-analysis detected by a simple,graphical test.BMJ 1997,315:629-634.
11.Fenwick J,Toohill J,Gamble J,et al.Effects of a midwife psycho-education intervention to reduce childbirth fear on women's birth outcomes and postpartum psychological wellbeing. BMC Pregnancy Childbirth 2015,15:284.
12.Turkstra E,Mihala G,Scuffham PA,et al.An economic evaluation alongside a randomised controlled trial on psycho-education counselling intervention offered by midwives to address women's fear of childbirth in Australia.Sex Reprod Healthc 2017,11:1-6.
13.Ren D.Effect analysis of psychological nursing of midwife in promoting natural childbirth.Jilin Med J 2015,2:22-25.
14.Xiao CY.Analysis on the effect of psychological nursing for midwives in promoting natural childbirth.Chin J Mod DrugAppl 2017,11:172-174.
15.XuZX,WangMX,LiY,etal.Effectof whole-course psychological intervention guided by midwives on primipar.China Med Pharam 2017,7:182-184.
16.Xu MX.Explore the effect of psychological nursing for midwives in promoting natural childbirth.World Latest Med Inf 2015,54:232-232.
17.Yang HY.Application of mental nursing to midwife during childbirth.ChinaPracMed 2017,12:173-174.
18.Yang LX.Psychological nursing of midwives during the first deliver.World Latest Med Inf 2016,3:284-285.
19.You GH.Effects of psychological nursing on natural childbirth of midwives were analyzed.World Latest Med Inf 2016,3:288-289.
20.Zhao JM.Effect of midwife psychological nursing on the outcome of parturient delivery.China J Pharm Ecom 2015,10:147-148.
21.Zhou GX.Effects of midwife psychological nursing intervention on parturientdelivery mode were evaluated.China Rural Health 2016,4:53-54.
22.Wang J.Observation on the effect of psychological nursing intervention on the outcome of childbirth.Med Inter 2017,7:323-324.
23.Cooke HM,Waters DL,Dyer K,et al.Development of a best practice model of midwifery-led antenatal care.Aus Midwifery 2004,17:21-25.
24.Spiby H,Munro J.The development and peer review of evidence-based guidelines to support midwifery led care in labor.Midwifery 2009,25:163-171.
25.Bick D.Enhancing safety in the maternity services:a greater role for midwife-led care.Midwifery 2009,25:1-2.
26.Taheri M,Takian A,Taghizadeh Z,et al.Creating a positive perception of childbirth experience:systematic review and meta-analysis of prenatal and intrapartum interventions.Reprod Health 2018,15:73.
27.Zargar M,Nikbakht R,Ahmadi M.The effect of tranexamic acid on preventing post-partum hemorrhage due to uterine atony:a triple-blind randomized clinical trial.Curr Clin Pharmacol 2018,34:290-294.
28.Chan RJ,Marx W,Bradford N,et al.Clinical and economic outcomes of nurse-led services in the ambulatory care setting:a systematic review.Int J Nurs Stud 2018,81:61-80.
29.Hu CY.A study on theeffectofmidwife accompanying the whole delivery process on the outcome of childbirth.Neimengu Med J 2015,47:1382-1385.
30.Roth C,Dent SA,Parfitt SE,et al.Randomized controlled trial of use of the peanut ball during labor.McnAm J Matern Child Nurs 2016,41:140-146.
猜你喜欢
杂志排行
TMR Non-Drug Therapy的其它文章
- Efficacy of Liuzijue respiratory exercise in patients with chronic obstructive pulmonary disease:a meta-analysis
- Based on the theory of traditional Chinese and western medicine for the co-treatment of neck,chest,and waist
- Systematicevaluationand trialsequentialanalysisofwarming acupuncture combined with joint mobilization in the treatment of scapulohumeral periarthritis
- Pricking cupping bloodletting combined with slide cupping for acne:a case report