Clinical Observation on Brachial Plexus Block with “One Injection Two Points” Method Guiding by Ultrasound
2017-06-05HungQing黄强CiLingling蔡玲玲ShiWnjing石静纹FngZhiyun方志远WuMicho吴美超SunZhohui孙朝辉SunYuln孙玉兰LiYong李勇LuShngting卢尚亭XuHui徐辉HWANGDONGWOOK黄童郁WngHongling王洪亮ZhngTo张涛
Hung Qing(黄强), Ci Lingling(蔡玲玲), Shi Wnjing(石静纹), Fng Zhiyun(方志远), Wu Micho(吴美超), Sun Zhohui(孙朝辉), Sun Yuln(孙玉兰), Li Yong(李勇), Lu Shngting(卢尚亭), Xu Hui(徐辉), HWANG DONGWOOK (黄童郁), Wng Hongling(王洪亮), n Zhng To(张涛)
Clinical Observation on Brachial Plexus Block with “One Injection Two Points” Method Guiding by Ultrasound
Huang Qiang(黄强)a, Cai Lingling(蔡玲玲)b, Shi Wenjing(石静纹)b, Fang Zhiyuan(方志远)b, Wu Meichao(吴美超)b, Sun Zhaohui(孙朝辉)a, Sun Yulan(孙玉兰)a, Li Yong(李勇)a, Lu Shangting(卢尚亭)a, Xu Hui(徐辉)c*, HWANG DONGWOOK (黄童郁)d, Wang Hongliang(王洪亮)e, and Zhang Tao(张涛)f
OBJECTIVE: To compare the clinical effect of brachial plexus block with “One Injection Two Points” guided under ultrasound and the conventional method guiding by ultrasound.
METHODS: 70 patients were randomized evenly into 2 groups, with 35 patients in each group, while the Experiment Group (Group B) received One Injection Two Points” method, the Control Group (Group A) received the conventional method. The nerve block every 5s, the success rate of anesthesia, the dosage of local anesthetics, second remedial anesthesia, adverse reactions, etc.were recorded.
RESULTS: Group B was superior to group A in the success rate of anesthesia; There were 6 patients in group A who required constant pump injection of Remifentanil to remedy, while no patients in Group B needed remedy treatment. There were no serious adverse reactions in both groups.
CONCLUSIONS: The clinical effect of brachial plexus block with “One Injection Two Points” method guided under ultrasoundguiding by ultrasound was superior to that of the conventional method.
Clinical observation; Ultrasound-guided; Brachial plexus block; “One Injection Two Points” method
INTRODUCTION
Brachial plexus nerve block guided under ultrasound was visual completely, while the first application was supraclavicular approach1. It was also known as “Spinal Anesthesia”of the upper limbs which was mainly applied to the upper limb surgery under the shoulder, but it was not complete in clinical.2Supraclavicular brachial plexus lies between trunks and strands, continues along the subclavian vessels. According to its anatomical characteristics, this research took the method of changing angle of ultrasonic probe to block the brachial plexus and comparing its effect with that of the conventional method for the purpose of solving incompletely brachial plexus nerve block.
MATERIALS AND METHODS
General materials
The clinical research was approved by the ethics committee of our hospital and every patient signed the informed consent. 70 cases of upper limb surgery were observed, including 48 male and 32 female, aged from 18 to 72 years old, ASAior ASA II. No patient had disturbance of blood coagulation or bleeding disorder, allergic history of local anesthetic, skin infection or damage of puncture site, psychogenia or communication difficulties. 70 patients were randomized evenly into 2 groups, with 35 patients in each group, while the Experiment Group (Group B) received One Injection Two Points” method, the Control Group (Group A) received the conventional method
Anesthesia method
ECG, SpO2 and BP of patients in the operation room were monitored. Patients in group A received conventional supraclavicular approach in supine position with their head to the contralateral side(illustration-1). Sonosite portable ultrasound with 6-13MHz high-frequency linear probe was used and, put it in supraclavicular fossa and made its long axis parallel to the clavicle, the subclavian artery was found,the upper and outer aspect of which was Diamond shaped or spindle shaped honeycomb of brachial plexus (illustration-3). Using the technique of short axis plane injection must keep needle body and the probe in a plane. Firstly, local anesthetic were injected in the posterior-inferior of the brachial plexus. Then, the needle was returned to the subcutaneous tissue and adjusted the needle angle to make the tip be close to the anterosuperior of the brachial plexus to inject again. It can be injected when the tip was close to the nerve surface with the purpose of making visible nerve completely surrounded by local anaesthetics (illustration-2). Patients of group B received the same conventional method of Group A. After supraclavicular brachial plexus was blocked, then the needle was returned to the subcutaneous tissue and made the ultrasonic probe rotate 20~30°with center of the puncture point to the proximal end nerve to get image of brachial plexus again. It performed honeycomb echo tissue (evolution process of nerve from trunks to strands). Local anaesthetics was injected in the posterior-inferior and anterosuperior of the brachial plexus for making visible nerve completely surrounded by local anaesthetics(illustration-4).
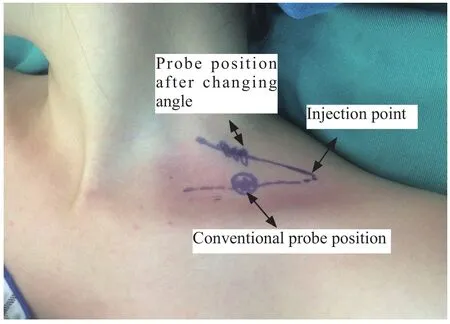
Illustration-1
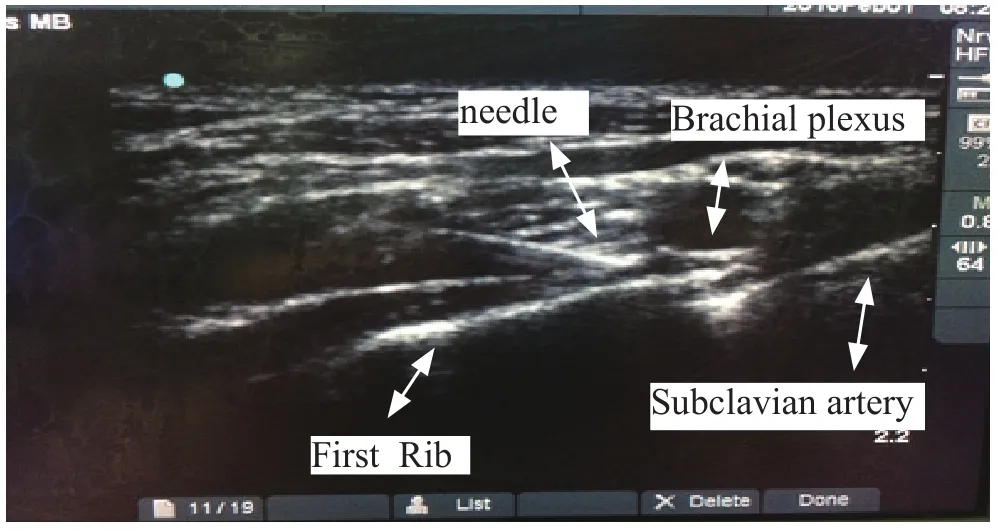
Illustration-2

Illustration-3 Brachial plexus after probe angle changed

Illustration-4 Needle after probe angle changed
Observation index and evaluate criteria
The anaesthesia operation time of two groups and observed the block conditions of median nerve, ulnar nerve, radial nerve, musculocutaneous nerve and medial antebrachial cutaneous nerve of forearm were recorded every 5min, with a total period of 30 mins. Determination of nerve block corresponding sensory areas: medial antebrachial cutaneous nerve of forearm corresponding area is medial area, the musculocutaneous nerve corresponding area is above the basal part of the first metacarpal, radial nerve corresponding area is thumb and index finger area, ulnar nerve corresponding area is hypothenar, median nerve corresponding area is second and third metacarpal palm side. Pain sensation after nerve block is divided into three level: the first level is painless, the second level is mild pain, the thirdlevel is feeling normal without block. If patients were in the third level for 30 mins, they should be remedied to block or general anesthesia. The success rate of anesthesia (no remedial block or general anesthesia) was recorded, anesthesia time (from block to pain again) complications (local anesthetics poisoning reaction, Horner syndrome,etc.), the operation time, the dose of local anesthetic and so on were also recored.
Statistical analysis
The results were analyzed using SPSS19.0. Measurement data were indicated as “mean value ±standard deviation.We used t-test to analyze measurements which conformed with normal distributions and non-parametric test to analyze measurements which conformed with non-normal distributions. We used chi-square test to analyze enumeration data. There were statistical differences (P<0.05), and there were significant statistical differences (P<0.01).
RESULTS
Age and weight of two groups were normal distribution after tested, so they were tested by independent samples T test. The results: both P were> 0.05, there was no significant difference. Gender proportion of two groups was countable data and should be taken in the chi-square test. The result: P>0.05, P=6.57, there was no significant difference (Table-1).
Table1 Comparison of the general Condition
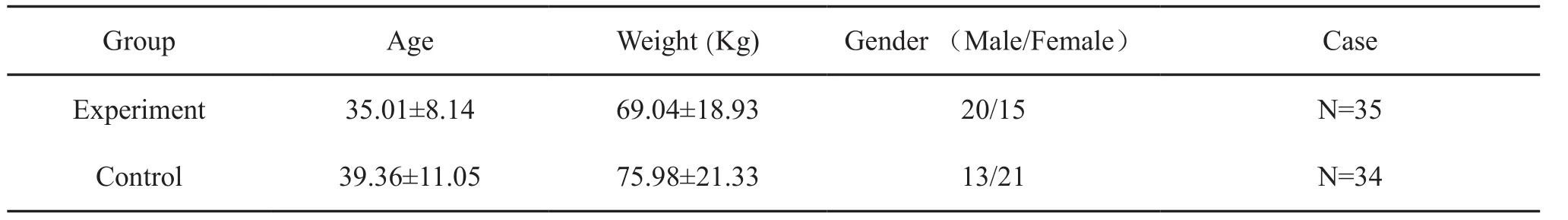
Table1 Comparison of the general Condition
Group Age Weight (Kg) Gender (Male/Female) Case Experiment 35.01±8.14 69.04±18.93 20/15 N=35 Control 39.36±11.05 75.98±21.33 13/21 N=34
Anesthesia time of one patient in group A was up to 15h. Considering that he was taken intrathecal injection, the case was eliminated. The effective rates and success rates should be taken in the chi-square test. Anesthesia time was normal distribution after being tested, so they were tested by independent samples T test. The result: ulnar nerve, medial forearm cutaneous nerve block effective rates and anesthesia success rates of group B were significantly better than that of group A(Table-2). There was no obvious adverse reaction in two groups. Follow-up visits in 48 hours after the operation. Indicated that no nerve injury was found in two groups.
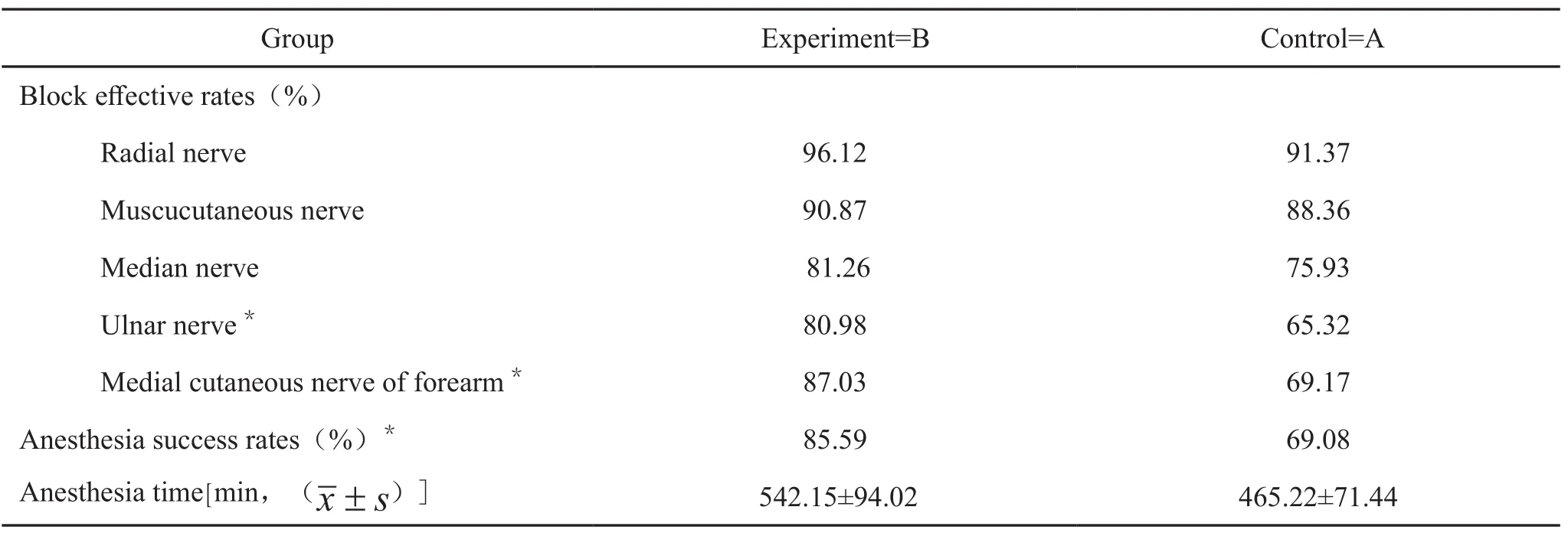
Table2 Comparison of anesthesia success rates, block effective rates and anesthesia time
DISCUSSION
Although it could avoid problems like flowing into vessels by mistake3, it’s hard for conventional method (of supraclavicular brachial plexus block) guided by ultrasound to block brachial plexus nerve completely4. A research shows that5the brachial plexus nerves in 85% individuals wrap around the outer top region of subclavian artery, while different degrees of variations occur to the rest 15%. Multiple puncture, such asrecombination of axillary or interscalene brachial plexus block are applied in clinical practice to improve success rate of anesthesia. However, it increases suffering during the process of reposition and psychological burden caused by two-time puncture. This research manifests that satisfactory result and complete upper limb block, can be achieved by “One Injection Two Points” method of supraclavicular brachial plexus nerve block, especially in patients with large range damage in upper arm that anesthetic effect is not easy to measure. Conventional method uses “bottomed bag”(forming an angle between subclavian artery and first rib) technology6and “three-point dosing” method7to improve the success rate of supraclavicular brachial plexus nerve block, but effective block in ulnar nerve and medial antebranchial cutaneous nerve is still low. The related reasons are as follows: Firstly, ulnar nerve and medial antebrachial cutaneous nerve derive from medial fasciculus, which originates in inferior trunk of brachial plexus, which are deep set; Secondly, though the graph displayed by ultrasound is visible, it fails to reveal the exact location in anatomy perspective—graph shown by ultrasound is two-dimensional, while the tissue punctured exists in three-dimensional way. Last, research from anatomy studies8indicates the diaphragm and fat exist through brachial nerve tracts, which prevent anesthetic drugs to penetrate.
“One Injection Two Points” Method of supraclavicular brachial plexus block shown in this study overcomes the shortages of the conventional one. In two-time block operation, brachial plexus changes in a process from nerve trunk to nerve tract. Graph displayed by ultrasound is not that gathered clusters as supraclavicular plexus graph, but strip-shape nerve circumvoluted by epineurium , which can be seen. Small amount of local anesthetics wrap it, two-time anesthetics cross block brachial plexus, which makes “two-time paresthesia”method used in blind puncture visible, thus makes up for inaccuracy of two-time block reciprocally.
In this study, “One Injection Two Points” method punctures distal brachial plexus and proximal ones. If distal plexus is blocked by local anesthetics, patients won’t feel numb or electric shock when puncture proximal brachial plexus. So operator is supposed to operate well, like keeping needles in the course of long axis, avoiding excessive resistance during injection in case of intrathecal injection. One patient in group A suffered from intrathecal injection, which worth powdering. No case of intercoatobrachial nerve blocked or tourniquet reaction happened in two groups, which may be concerned with cross dominance of intrathecal nerve and medial brachial cutaneous nerve over the skin of upper interior arm.
In conclusion, “One Injection Two Points” method of supraclavicular brachial plexus visualizes two-time block by ultrasound. It’s worth being applied widely in clinical practice on account of high rate of accuracy and positive effect.
REDERENCES
1 la Grange P,Foster PA,Pretorius LK. Application of the Doppler ultrasound bloodflow detector in supraclavicular brachial plexus block [J]. Br J Anaesth,1978,50(9):965-967.
2 Gamo K, Kuriyama K, Higuchi H, et al. Ultrasoundguidedsupraclavicular brachial plexus block in upper limb surgery: outcomes and patient satisfaction.[J]. Bone & Joint Journal, 2014, 96-b(6):795-799.
3 Christopher Hahn,MD,Arun Nagdev MD,Color Dopplerultrasound-guided supraclavicular brachial plexus block to prevent vascular injection.West J Emerg Med,2014 Sep:15(6):703-705.
4 Fredrickson MJ,Patel A,Young S,et,al.Speed of onset of corner pocket supraclavicular' and infraclavicular ultrasound guided brachial plexus block: a randomized observerblinded comparison.Anaesthesia,2009,64(7):738.
5 Royse CF,sha S,Soeding PF,et al. Anatomical study of the brachial plexus using surface ultrasound. Anaesth Intensive Care,2006,34(2):203-210.
6 Macfarlane AJ,Perlas A,Chan v,et al.Eight ball, corner pocket ultrasound guided supraclavicular block: avoiding a scratch. Reg Anesth Pain Med,2008(5):502.
7 Arab SA, Alharbi MK, Nada EM, et al. Ultrasound-guided supraclavicular brachial plexus block: single versus triple injection technique for upper limb arteriovenous access surgery.Anesth Analg,2014,118(5):1120.
8 Chan vw,perlas A,Rawson R,et al.Ultrasound-Guided Supraclavicular Brachial Plexus Block.Anesth Analg,2003,97(5):1514-1517.
(Accepted: March,15,2017)
a: Department of Anesthesiology, Center Hospital of Shanxian, Shandong Province, Shanxian city 274300, China
b: Department of Dermatology, Dongfang Hospital, the Second Affiliated Hospital of Beijing University of Chinese Medicine, Beijing 100000, China
c: Department of Anesthesiology, People’s Hospital of Linzi district, Shandong Province, Zibo city 255000, China
d: Yueyang Hospital of Shanghai University of Chinese Medicine, Shanghai 200000, China
e: Heilongjiang University Of Chinese Medicine, Harbin 150000, China
f:The People’s Liberation Army 404 Hospital, Weihai 264200, China
*Corresponding author: Email: xuhui8318@sina.com
